Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Suspension, Oral:
Purixan: 2000 mg/100 mL (100 mL) [contains aspartame, methylparaben, propylparaben]
Tablet, Oral:
Generic: 50 mg
Pharmacology
Mechanism of Action
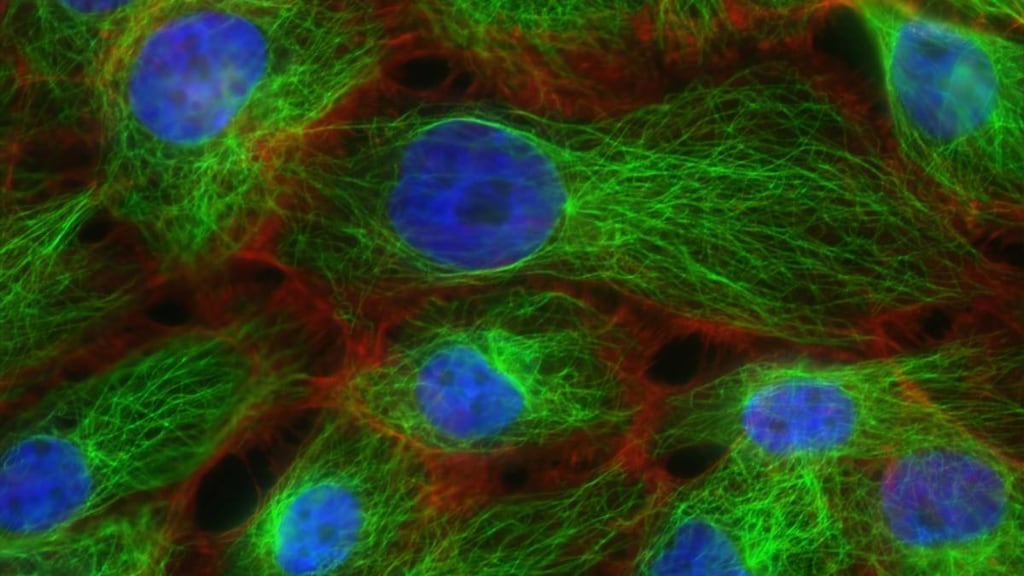
Mercaptopurine is a purine antagonist which inhibits DNA and RNA synthesis; acts as false metabolite and is incorporated into DNA and RNA, eventually inhibiting their synthesis; specific for the S phase of the cell cycle
Pharmacokinetics/Pharmacodynamics
Absorption
Variable and incomplete (~50% of a dose is absorbed); Cmax of suspension is 34% higher than the tablet
Distribution
Vd > total body water; CNS penetration is poor
Metabolism
Hepatic and via GI mucosa; hepatically via xanthine oxidase and methylation via thiopurine methyltransferase to sulfate conjugates, 6-thiouric acid, and other inactive compounds; first-pass effect
Excretion
Urine (46% as mercaptopurine and metabolites)
Time to Peak
Serum: Within 2 hours
Half-Life Elimination
Tablets: Children: 21 minutes; Adults: 47 minutes; Suspension: ~2 hours
Protein Binding
~19%
Use in Specific Populations
Special Populations: Renal Function Impairment
Renal impairment may result in slower elimination of parent drug and metabolites, and a greater cumulative effect.
Use: Labeled Indications
Acute lymphoblastic leukemia: Treatment of acute lymphoblastic leukemia (ALL), as part of a combination chemotherapy regimen
Use: Off Label
Acute promyelocytic leukemia, maintenancea
Data from a phase III study of combination chemotherapy in patients with acute promyelocytic leukemia (APL) supports the use of mercaptopurine as part of the maintenance phase of treatment Powell 2010.
Crohn disease (management after surgical resection)byes
Data from a small randomized, double-blind, placebo-controlled multicenter trial and from 2 meta-analyses support the use of mercaptopurine as management of Crohn disease after surgical resection and has demonstrated to lower endoscopic and clinical recurrence rates Hanauer 2004, Peyin-Biroulet 2009, Singh 2015. Data from a randomized, placebo controlled study suggests the benefit of mercaptopurine (after resection) may be increased when given in combination with metronidazole De Cruz 2015.
Based on the American Gastroenterological Association Institute Guidelines for the Management of Crohn's Disease after Surgical Resection, mercaptopurine is an effective prophylactic therapy in patients who are higher risk for clinical recurrence following surgical resection.
Crohn disease (remission maintenance or steroid-sparing therapy)yes
Based on the American College of Gastroenterology guidelines for the Management of Crohn disease in Adults, mercaptopurine in combination with an anti-TNF agent (eg, adalimumab, infliximab) for remission maintenance or reduction of steroid use is effective and recommended in the management of this condition. In addition, these guidelines state that mercaptopurine is not more effective than placebo to induce short-term symptomatic remission and is not recommended for this use. For moderate to severe or moderate to high-risk disease, mercaptopurine may be used in treatment of active disease or as adjunctive therapy for reducing immunogenicity.
Lymphoblastic lymphomab
Data from a small study in adolescents and adults supports the use of mercaptopurine as a component of maintenance treatment of lymphoblastic lymphoma Thomas 2004. Two studies in acute lymphoblastic leukemia also included patients with lymphoblastic lymphoma; these patients usually respond to the same mercaptopurine-containing maintenance regimens used in treatment for acute lymphoblastic leukemia Kantarjian 2000, Stock 2008.
Ulcerative colitis (remission induction)cyes
Data from a review article summarizing clinical evidence Siegel 2005 support the use of mercaptopurine in the initial management of ulcerative colitis.
Based on the American College of Gastroenterology (ACG) guidelines for ulcerative colitis in adults, a thiopurine (eg, mercaptopurine), in combination with infliximab, is recommended for induction of remission in patients with moderate to severely active ulcerative colitis when infliximab is used as induction therapy. According to the guidelines, mercaptopurine monotherapy is not recommended for remission induction in patients with moderately to severely active ulcerative colitis.
Ulcerative colitis (remission maintenance)cyes
In a meta-analysis of randomized clinical trials evaluating the efficacy of thiopurines (eg, mercaptopurine) for induction and/or maintenance of ulcerative clinical remission, evidence suggests mercaptopurine may be of benefit for the maintenance of remission in patients with ulcerative colitis Gisbert 2009.
Clinical evidence and recommendations from the British Society of Gastroenterology also suggest that mercaptopurine may be beneficial for the maintenance treatment of ulcerative colitis Carter 2004, Danese 2011.
Based on the ACG guidelines for ulcerative colitis in adults, a thiopurine (eg, mercaptopurine) may be used for maintenance of remission in patients with previously moderately to severely active ulcerative colitis currently in remission following corticosteroid induction.
Contraindications
Hypersensitivity to mercaptopurine or any component of the formulation; patients whose disease showed prior resistance to mercaptopurine
Dosage and Administration
Dosing: Adult
Note: Consider testing for thiopurine S-methyltransferase (TPMT) and nudix hydrolase 15 (nucleotide diphosphatase [NUDT15]) deficiency; patients with TPMT or NUDT15 deficiency are at increased risk for severe toxicity at conventional mercaptopurine doses and generally require dose reduction (see Dosage adjustment for TPMT or NUDT15 deficiency below) (Relling 2019).
Acute lymphoblastic leukemia (ALL): Maintenance: Oral: 1.5 to 2.5 mg/kg once daily (50 to 75 mg/m2 once daily); continue based on blood counts or
Off-label ALL dosing (combination chemotherapy; refer to specific reference for combinations):
Early intensification (two 4-week courses): 60 mg/m2/day days 1 to 14 (Larson 1995; Larson 1998).
Interim maintenance (12-week course): 60 mg/m2/day days 1 to 70 (Larson 1995; Larson 1998).
Maintenance (prolonged): 50 mg 3 times/day for 2 years (Kantarjian 2000) or 60 mg/m2/day for 2 years from diagnosis (Larson 1995; Larson 1998).
AALL0232 (Larsen 2016): Patients ≤30 years:
Consolidation: Oral: 60 mg/m2 once daily on days 1 to 14 and 29 to 42 of a 56-day cycle (in combination with cyclophosphamide, cytarabine, vincristine, pegaspargase, and intrathecal methotrexate).
Interim Maintenance 1 and 2: Oral: 25 mg/m2 once daily on days 1 to 56 (in combination with vincristine, high-dose methotrexate, and intrathecal methotrexate).
Maintenance phase: Oral: 75 mg/m2 once daily on days 1 to 84 of an 84-day cycle (in combination with vincristine, steroid, oral methotrexate, and intrathecal methotrexate). Maintenance cycles are repeated for a total duration of 2 years (females) and 3 years (males) from the start of Interim Maintenance I. During Maintenance, the mercaptopurine (and oral methotrexate) dose may be titrated to target absolute neutrophil count (ANC) and platelet count goals.
Acute promyelocytic leukemia, maintenance (off-label use): 60 mg/m2/day for 1 year (in combination with tretinoin and methotrexate) (Powell 2010).
Crohn disease, management after surgical resection (off-label use): Oral: 1.5 mg/kg/day (in combination with metronidazole) for ~18 months after surgery (De Cruz 2015) or 50 mg once daily for 24 months, beginning prior to discharge from hospital (Hanauer 2004).
Crohn disease (remission maintenance or steroid-sparing therapy) (off-label use): Oral: 0.75 to 1.5 mg/kg/day in combination with an anti-TNF agent (eg, adalimumab, infliximab) (Lichtenstein 2018).
Lymphoblastic lymphoma (off-label use): Maintenance (prolonged): 50 mg 3 times daily for 2 years (Kantarjian 2000; Thomas 2004).
Ulcerative colitis, remission induction (off-label use): Oral: Initial: 50 mg once daily; titrate up to 1.5 mg/kg/day as tolerated (Siegel 2005). Note: Monotherapy is not recommended in patients with moderately to severely active ulcerative colitis (ACG [Rubin 2019]).
Ulcerative colitis, remission maintenance (off-label use): Oral: 1 to 1.5 mg/kg/day (Carter 2004; Danese 2011).
Dosage adjustment for TPMT and/or NUDT15 deficiency:
Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines (Relling 2019):
Normal TPMT or NUDT15 activity (wild type): No initial dosage adjustment necessary; adjust dose based on condition being treated. Allow at least 2 weeks after each dosage adjustment to reach steady state. For patients receiving combination therapy, dosage adjustments (of all agents) should be made without any emphasis on mercaptopurine compared to other agents.
TPMT intermediate or possible intermediate metabolizer or NUDT15 intermediate or possible intermediate metabolizer: Initiate mercaptopurine with the dose reduced to 30% to 80% of the usual dose and adjust dose based on the degree of myelosuppression and condition being treated. Allow 2 to 4 weeks after each dosage adjustment to reach steady state. If myelosuppression occurs, the focus should be on reducing the mercaptopurine dose over other agents (depending on concomitant therapy). If the starting dose is already below the normal recommended dose, dose reduction may not be recommended.
TPMT poor metabolizer: When used for malignancy, initiate mercaptopurine at a drastically reduced dose (reduce the daily dose by 10-fold and reduce the frequency from once daily to 3 times a week). Adjust dose based on the degree of myelosuppression and condition being treated. Allow 4 to 6 weeks after each dosage adjustment to reach steady state. If myelosuppression occurs, the focus should be on reducing the mercaptopurine dose over other agents (depending on concomitant therapy). When used for nonmalignant conditions, consider alternative (non-thiopurine) immunosuppressant therapy.
NUDT15 poor metabolizer: When used for malignancy, initiate mercaptopurine at 10 mg/m2/day. Adjust dose based on the degree of myelosuppression and condition being treated. Allow 4 to 6 weeks after each dosage adjustment to reach steady state. If myelosuppression occurs, the focus should be on reducing the mercaptopurine dose over other agents (depending on concomitant therapy). When used for nonmalignant conditions, consider alternative (non-thiopurine) immunosuppressant therapy.
Manufacturer’s labeling:
Heterozygous deficiency (intermediate activity): Reduce the dose based on tolerability; most patients with heterozygous deficiency of TPMT or NUDT15 tolerate recommended doses, although some require dosage reduction. Patients who are heterozygous for both TPMT and NUDT15 may require more substantial dose reductions.
Homozygous deficiency (low or deficient activity): Reduce the mercaptopurine dose to 10% of the usual dose or lower for homozygous deficiency in either TPMT or NUDT15.
Dosage adjustment with concurrent allopurinol: Avoid concomitant use. If administered concurrently, reduce mercaptopurine dosage to 25% to 33% of the usual dose.
Dosing: Geriatric
Due to renal decline with age, initiate treatment at the low end of recommended dose range.
Dosing: Pediatric
Note: Patients with minimal or no thiopurine S-methyltransferase (TPMT) activity are at increased risk for severe toxicity at conventional mercaptopurine doses and generally require dose reduction; consider testing for TPMT and nudix hydrolase 15 (nucleotide diphosphatase [NUDT15]) deficiency (see Dosage adjustment for TPMT or NUDT15 deficiency below). Pediatric doses presented as mg/m2 and mg/kg; use extra precaution.
Acute lymphoblastic leukemia (ALL): Multiple regimens/protocols reported; limited data available; refer to specific protocols.
Standard Risk (Bostrom 2003; Stork 2010): Children 1 to <10 years: Consolidation, Interim Maintenance I and Maintenance: Oral: 75 mg/m2 once daily frequency and duration dependent on protocol phase (in combination with vincristine, steroid, methotrexate [oral and/or intrathecal]). Maintenance cycles are repeated for a total duration of 2 years (females) and 3 years (males) from the start of Interim Maintenance I. During Maintenance, oral methotrexate and mercaptopurine are adjusted to maintain a target ANC goal (generally 1,000 to 2,000/mm3, varies based on protocol)
High risk (Larsen 2016): Children 1 to <10 years:
Consolidation: Oral: 60 mg/m2 once daily on days 1 to 14 and 29 to 42 of a 56-day cycle (in combination with cyclophosphamide, cytarabine, vincristine, pegaspargase, and intrathecal methotrexate)
Interim Maintenance: Oral: 25 mg/m2 once daily on days 1 to 56 (in combination with vincristine, high-dose methotrexate, and intrathecal methotrexate)
Maintenance phase: Oral: 75 mg/m2 once daily on days 1 to 84 of an 84-day cycle (in combination with vincristine, steroid, oral methotrexate, and intrathecal methotrexate). Maintenance cycles are repeated for a total duration of 2 years (females) and 3 years (males) from the start of Interim Maintenance I. During Maintenance, the oral methotrexate and mercaptopurine are titrated to a target ANC goal (generally 1,000 to 2,000/mm3, varies based on protocol)
Acute promyelocytic leukemia (APL): Limited data available; multiple regimens reported:
Combination with tretinoin: Maintenance phase: Children and Adolescents ≤14 years: Oral: 100 mg/m2/day for 14 days of a 28-day cycle in combination with tretinoin. Cycles were repeated every 28 days for 2 years (Zhang 2011).
Combination with tretinoin and methotrexate:
Ortega 2005: PETHEMA Group: Maintenance phase: Children and Adolescents <17 years: Oral: 50 mg/m2/day for 2 years in combination with methotrexate and tretinoin. Doses of mercaptopurine and methotrexate were decreased by 50% if the WBC count was <3,500 cells/mm3 and discontinued for WBC <2,500/mm3.
Powell 2010: North American Leukemia Intergroup Study C9710: Maintenance phase: Adolescents ≥15 years: Oral: 60 mg/m2/day for 1 year; in combination with tretinoin and methotrexate
Autoimmune hepatitis: Very limited data available: Children and Adolescents: Oral: 1.5 mg/kg/day in combination with prednisone; not considered first-line, typically used for patients who do not tolerate azathioprine (Manns 2010)
Inflammatory bowel disease (eg, Crohn disease, ulcerative colitis): Limited data available: Children and Adolescents: Oral: 1 to 1.5 mg/kg/day (Markowitz 2000; Punati 2008; Sandhu 2010). Some data suggest that pediatric patients ≤6 years may require higher doses to achieve remission; a median dose of 1.68 mg/kg/day (maximum daily dose: 2.4 mg/kg/day) was reported to induce remission in 62% of patients vs 17% of those receiving lower doses (<1.5 mg/kg/day study group; median dose: 1.18 mg/kg/day) (Grossman 2008; Sandborn 2001); maximum: 50 mg/day in the first week and increase to full dose when patients experience no adverse effects (Meijer 2016)
Dosing adjustment with concurrent allopurinol: Children and Adolescents: Reduce mercaptopurine dosage; some protocols may require more aggressive reduction than others (Zerra 2016)
Dosing adjustment in TPMT and/or NUDT15 deficiency: Limited data available (Relling 2011; Relling 2013):
Heterozygous deficiency (intermediate activity): Reduce the dose based on tolerability; according to the manufacturer, most patients with heterozygous deficiency of TPMT or NUDT15 tolerate recommended doses, although some require dosage reduction. Patients who are heterozygous for both TPMT and NUDT15 may require more substantial dose reductions.
Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines for reduced TPMT activity (Relling 2011; Relling 2013): Initiate mercaptopurine at a reduced dose of 30% to 70% of the usual dose and adjust based on the degree of myelosuppression and condition being treated. Allow 2 to 4 weeks after each dosage adjustment to reach steady state. If a dosage adjustment is required based on myelosuppression, the median dose may be ~40% lower than the dose tolerated in wild-type patients. For patients receiving combination therapy who experience severe myelosuppression, the focus should be on reducing the mercaptopurine dose over other agents (depending on concomitant therapy).
Homozygous deficiency (low or deficient activity): Reduce the mercaptopurine dose to 10% of the usual dose or lower for homozygous deficiency in either TPMT or NUDT15.
CPIC guidelines for reduced TPMT activity (Relling 2011; Relling 2013): When used for cancer treatment, initiate mercaptopurine with drastically reduced doses (reduce the daily dose by 10-fold and reduce the frequency from once daily to 3 times a week). Adjust doses based on the degree of myelosuppression and condition being treated. Allow 4 to 6 weeks after each dosage adjustment to reach steady state. For patients receiving combination therapy who experience severe myelosuppression, the focus should be on reducing the mercaptopurine dose over other agents (depending on concomitant therapy). When used for nonmalignant conditions, consider alternative (non-thiopurine) immunosuppressant therapy.
Homozygous wild type (normal activity): CPIC guidelines for reduced TPMT activity (Relling 2011; Relling 2013): No initial dosage adjustment necessary. Allow 2 weeks after each dosage adjustment to reach steady state. For patients receiving combination therapy, dosage adjustments (of all agents) should be made without any emphasis on mercaptopurine compared to other agents.
Dosing: Adjustment for Toxicity
Adjust dosage for excessive hematologic toxicity.
Reconstitution
Suspension: Wear disposable gloves when handling. Shake bottle vigorously for at least 30 seconds prior to administration. Attach the bottle adaptor into the neck of the bottle (do not remove after insertion). Measure dose with an oral dosing syringe to ensure proper dose is administered. Oral syringe provided by the manufacturer is intended to be reused, wash with warm soapy water and rinse well (hold syringe under water and move plunger several times to ensure inside of syringe is clean); allow to dry completely.
Extemporaneously Prepared
A 50 mg/mL oral suspension may be prepared in a vertical flow hood with tablets and a mixture of sterile water for injection (SWFI), simple syrup, and cherry syrup. Crush thirty 50 mg tablets in a mortar and reduce to a fine powder. Add ~5 mL SWFI and mix to a uniform paste; then add ~10 mL simple syrup; mix while continuing to add cherry syrup to make a final volume of 30 mL; transfer to a calibrated bottle. Label "shake well" and "caution chemotherapy". Stable for 35 days at room temperature.
Aliabadi HM, Romanick M, Desai, S, et al, “Effect of Buffer and Antioxidant on Stability of a Mercaptopurine Suspension,” Am J Health Syst Pharm 2008, 65(5):441-7. 18281736
Administration
Administer preferably on an empty stomach (Burton 1986; Kantarjian 2000); avoid concomitant milk products if possible (de Lemos 2007). Administer at the same time(s) each day.
If adherence is limited by administering on an empty stomach in the evening or by avoiding concomitant milk products, simplification of administration (eg, take with food/dairy without regard to time of day) should be considered. In adherent patients (taking mercaptopurine regularly), no association was seen between risk of ALL relapse and mercaptopurine ingestion habits; there was also no association noted with red cell thioguanine nucleotide (TGN) levels and administration with food, dairy, or time of day (Landier 2017).
Suspension: Shake vigorously for at least 30 seconds to ensure suspension is mixed thoroughly (suspension is viscous). Measure dose with an oral dosing syringe (a 1 mL and a 5 mL oral dosing syringe are supplied by the manufacturer) to assure proper dose is administered. Patients and caregivers should be trained on appropriate measuring and administration, handling, storage, disposal, cleanup of accidental spills, and proper cleaning of oral dosing syringe. Use within 8 weeks after opening.
Storage
Tablets: Store at 20°C to 25°C (68°F to 77°F). Store in a dry place.
Suspension: Store at 15°C to 25°C (59°F to 77°F). Do not store above 25°C (77°F). Store in a dry place. Use within 8 weeks after opening.
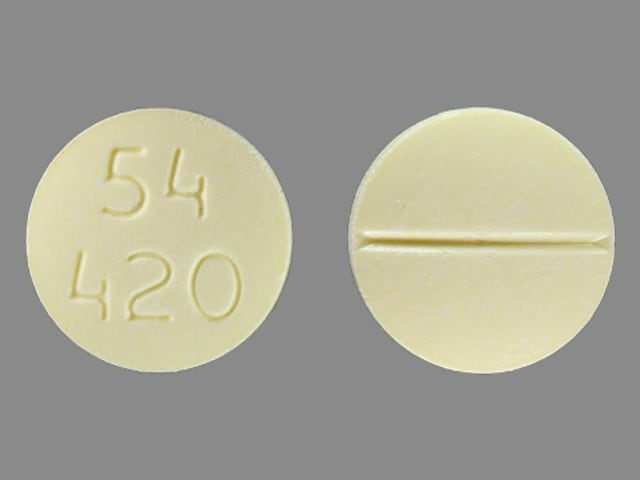
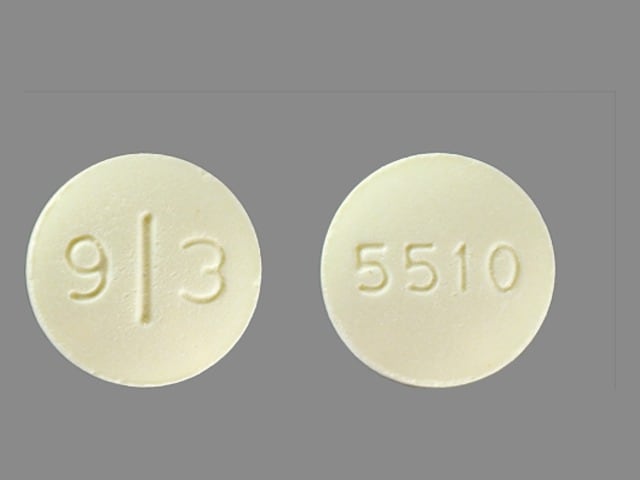
Mercaptopurine Images
Drug Interactions
5-Aminosalicylic Acid Derivatives: May decrease the metabolism of Thiopurine Analogs. Monitor therapy
Allopurinol: May increase the serum concentration of Mercaptopurine. Allopurinol may also promote formation of active thioguanine nucleotides. Management: Reduce the mercaptopurine dose to one third to one quarter of the usual dose if used with allopurinol, and monitor closely for systemic toxicity. US labeling for mercaptopurine oral suspension (Purixan brand) recommends avoiding allopurinol. Consider therapy modification
Anti-TNF Agents: May enhance the adverse/toxic effect of Thiopurine Analogs. Specifically, the risk for T-cell non-Hodgkin's lymphoma (including hepatosplenic T-cell lymphoma) may be increased. Exceptions: Lenalidomide; Pomalidomide; Thalidomide. Monitor therapy
AzaTHIOprine: May enhance the myelosuppressive effect of Mercaptopurine. Avoid combination
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
Cladribine: Agents that Undergo Intracellular Phosphorylation may diminish the therapeutic effect of Cladribine. Avoid combination
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
DOXOrubicin (Conventional): May enhance the hepatotoxic effect of Mercaptopurine. Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Febuxostat: May increase the serum concentration of Mercaptopurine. Avoid combination
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Lenograstim: Antineoplastic Agents may diminish the therapeutic effect of Lenograstim. Management: Avoid the use of lenograstim 24 hours before until 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Lipegfilgrastim: Antineoplastic Agents may diminish the therapeutic effect of Lipegfilgrastim. Management: Avoid concomitant use of lipegfilgrastim and myelosuppressive cytotoxic chemotherapy. Lipegfilgrastim should be administered at least 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Methotrexate: May increase the serum concentration of Mercaptopurine. Conversely, intracellular concentrations of thioguanine nucleotides may be decreased with the combination. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Palifermin: May enhance the adverse/toxic effect of Antineoplastic Agents. Specifically, the duration and severity of oral mucositis may be increased. Management: Do not administer palifermin within 24 hours before, during infusion of, or within 24 hours after administration of myelotoxic chemotherapy. Consider therapy modification
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Sulfamethoxazole: May enhance the myelosuppressive effect of Mercaptopurine. Monitor therapy
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Trimethoprim: May enhance the myelosuppressive effect of Mercaptopurine. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Mercaptopurine may enhance the adverse/toxic effect of Vaccines (Live). Mercaptopurine may diminish the therapeutic effect of Vaccines (Live). Management: Low-dose 6-mercaptopurine (1.5 mg/kg/day or less) is not considered sufficiently immunosuppressive to create vaccine safety concerns and is not a contraindication for administration of zoster vaccine. Higher doses of mercaptopurine should be avoided. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Mercaptopurine may diminish the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Test Interactions
TPMT testing: Recent transfusions may result in a misinterpretation of the actual TPMT activity. Concomitant drugs may influence TPMT activity in the blood.
Adverse Reactions
Frequency not always defined.
Central nervous system: Malaise (5% to 20%), drug fever
Dermatologic: Skin rash (5% to 20%), hyperpigmentation (<5%), urticaria (<5%), alopecia
Endocrine & metabolic: Hyperuricemia (<5%)
Gastrointestinal: Anorexia (5% to 20%), diarrhea (5% to 20%), nausea (5% to 20%; minimal), vomiting (5% to 20%; minimal), oral lesion (<5%), pancreatitis (<5%), cholestasis, mucositis, sprue-like symptoms, stomach pain, ulcerative bowel lesion
Genitourinary: Oligospermia, renal toxicity, uricosuria
Hematologic & oncologic: Bone marrow depression (>20%; onset 7 to 10 days; nadir 14 days; recovery: 21 days), anemia, granulocytopenia, hemorrhage, hepatosplenic T-cell lymphomas, leukopenia, lymphocytopenia, metastases, neutropenia, thrombocytopenia
Hepatic: Hyperbilirubinemia (<5%), increased serum transaminases (<5%), ascites, hepatic encephalopathy, hepatic fibrosis, hepatic injury, hepatic necrosis, hepatomegaly, hepatotoxicity, intrahepatic cholestasis, jaundice, toxic hepatitis
Immunologic: Immunosuppression
Infection: Infection
Respiratory: Pulmonary fibrosis
<1%, postmarketing, and/or case reports: Hypoglycemia, portal hypertension, skin photosensitivity
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: Dose-related leukopenia, thrombocytopenia, and anemia are common; however, may be indicative of disease progression. Hematologic toxicity may be delayed. Bone marrow may appear hypoplastic (could also appear normal). Monitor blood counts; dose may require adjusting for severe neutropenia or thrombocytopenia. Monitor for bleeding (due to thrombocytopenia) or infection (due to neutropenia). Profound severe or repeated hematologic toxicity may be indicative of thiopurine methyltransferase (TPMT) deficiency or nudix hydrolase 15 (nucleotide diphosphatase [NUDT15]) deficiency (see “TPMT or NUDT15 deficiency” below); patients who are homozygous for TPMT or NUDT15 deficiency may require substantial dosage reductions. TPMT genotyping or phenotyping or NUDT15 genotyping can identify patients with reduced TPMT or NUDT15 enzyme activity.
- Hepatotoxicity: Hepatotoxicity has been reported, including jaundice, ascites, hepatic necrosis (may be fatal), intrahepatic cholestasis, parenchymal cell necrosis, and/or hepatic encephalopathy; may be due to direct hepatic cell damage or hypersensitivity. While hepatotoxicity or hepatic injury may occur at any dose, dosages exceeding the recommended dose are associated with a higher incidence. Signs of jaundice generally appear early in treatment, after ~1 to 2 months (range: 1 week to 8 years) and may resolve following discontinuation; recurrence with rechallenge has been noted. Monitor liver function tests, including transaminases, alkaline phosphatase, and bilirubin weekly with treatment initiation, then monthly thereafter (monitor more frequently if used in combination with other hepatotoxic drugs or in patients with preexisting hepatic impairment). Consider a reduced dose in patients with baseline hepatic impairment; monitor closely for toxicity. Withhold treatment for clinical signs of jaundice (hepatomegaly, anorexia, tenderness), deterioration in liver function tests, toxic hepatitis, or biliary stasis until hepatotoxicity is ruled out.
- Immunosuppression: Mercaptopurine is immunosuppressive; immune responses to infections may be impaired and the risk for infection is increased. Common signs of infection, such as fever and leukocytosis may not occur; lethargy and confusion may be more prominent signs of infection.
- Macrophage activation syndrome: Macrophage activation syndrome (MAS), also known as hemophagocytic lymphohistiocytosis, is a life-threatening disorder which may develop in patients with autoimmune disorders (particularly inflammatory bowel disease); mercaptopurine use for the treatment of autoimmune conditions (off-label use) may cause increased susceptibility to MAS. Discontinue mercaptopurine if MAS develops or is suspected. Monitor; promptly treat infections such as Epstein-Barr virus (EBV) and cytomegalovirus (which are known triggers for MAS).
- Photosensitivity: Minimize sun exposure due to possible photosensitivity.
- Secondary malignancy: Immunosuppressive agents, including mercaptopurine, are associated with the development of lymphoproliferative disorders and other malignancies. In an analysis of T-cell lymphomas associated with TNF blockers (with or without thiopurines) for the treatment of rheumatoid arthritis, Crohn disease, ulcerative colitis, or ankylosing spondylitis (off-label uses for thiopurines), an increase in the incidence of T-cell lymphomas, most commonly mycosis fungoides/Sézary syndrome and hepatosplenic T-cell lymphoma (HSTCL) was reported (Deepak 2013). HSTCL is a rare white blood cell cancer that is usually fatal. Most HSTCL cases occurred in patients treated with a combination of TNF blockers and thiopurines, although cases of HSTCL also occurred in patients receiving azathioprine or mercaptopurine monotherapy. Skin cancers (melanoma and non-melanoma), Kaposi and non-Kaposi sarcomas, and uterine cervical cancer in situ have been reported in patients receiving immunosuppressive treatment (including mercaptopurine); risk of development may be related to the degree and duration of immunosuppression. Partial regression of lymphoproliferative disorders may occur upon therapy discontinuation. Regimens containing multiple immunosuppressants increase the risk of EBV-associated lymphoproliferative disorders; use with caution.
Disease-related concerns:
- Renal impairment: Consider dosage modification in patients with renal impairment (lower doses or extended dosing intervals). Some renal adverse effects may be minimized with hydration and prophylactic antihyperuricemic therapy.
- TPMT or NUDT15 deficiency: Patients with reduced TPMT or NUDT15 activity have a higher risk of severe myelosuppression with usual doses of thiopurines (eg, mercaptopurine, azathioprine, thioguanine) and may require substantial thiopurine dose reductions. Individuals who are TPMT homozygous or compound heterozygous deficient are at very high risk for severe myelosuppression (Relling 2019). TPMT genotyping or phenotyping and NUDT15 genotyping may assist in identifying patients at risk for developing toxicity. Consider testing for NUDT15 and TPMT deficiency in patients who experience severe bone marrow toxicities or repeated myelosuppressive episodes. Accurate phenotyping (red blood cell TPMT activity) results are not possible in patients who have received recent blood transfusions. The Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for thiopurine dosing based on TPMT and NUDT15 genotypes (Relling 2019) recommends reduced initial doses for TPMT and NUDT15 intermediate (and possible intermediate) metabolizers (with dosage adjustments based on myelosuppression). For TPMT and NUDT15 poor metabolizers, CPIC guideline recommends considering alternative nonthiopurine agents for nonmalignant conditions and drastically reduced doses if used to treat malignancy. Genetic TPMT deficiency is the primary cause of thiopurine intolerance in Europeans and Africans; NUDT15 risk alleles are associated with a majority of thiopurine intolerance in Asians and are also common in Hispanics (Relling 2019).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information. Because azathioprine is metabolized to mercaptopurine, concomitant use with azathioprine may result in a significant increase in hematologic toxicity and profound myelosuppression; avoid concurrent use. Hematologic toxicity may be exacerbated by other medications which inhibit TPMT (eg, mesalamine, olsalazine, sulfasalazine) or by other myelosuppressive drugs.
Special populations:
- Pediatric: Cases of symptomatic hypoglycemia have been reported in children receiving mercaptopurine for the treatment of ALL; cases were reported in children less than 6 years of age or with a low body mass index.
Other warnings/precautions:
- Error-prone terms: To avoid potentially serious dosage errors, the terms “6-mercaptopurine” or “6-MP” should be avoided; use of these terms has been associated with six-fold overdosages.
- Vaccines: Immune response to vaccines may be diminished. Live virus vaccines impose a risk for infection.
Monitoring Parameters
CBC with differential (weekly initially, although clinical status may require increased frequency), bone marrow exam (to evaluate leukemia status and marrow cellularity in patients with prolonged or repeated myelosuppression), liver function tests (transaminases, alkaline phosphatase, and bilirubin; weekly initially, then monthly; monitor more frequently if on concomitant hepatotoxic agents or in patients with preexisting hepatic impairment), renal function, urinalysis; signs/symptoms of macrophage activating syndrome; photosensitivity reactions. Monitor adherence.
Thiopurine S-methyltransferase (TPMT) genotyping or phenotyping: Consider testing for TPMT deficiency, particularly in patients with abnormally low CBC unresponsive to dose reduction. TPMT genotyping or phenotyping may assist in identifying patients at risk for developing toxicity (Relling 2019).
Nudix hydrolase 15 (NUDT15) genotyping: Consider genotyping for NUDT15 deficiency in patients who experience severe bone marrow toxicities or repeated myelosuppressive episodes. NUDT15 genotyping may assist in identifying patients at risk for developing toxicity (Relling 2019).
Crohn disease or ulcerative colitis (off-label uses): Monitor CBC with differential weekly for 1 month, then biweekly for 1 month, followed by monitoring every 1 to 2 months throughout the course of therapy. LFTs should be assessed every 3 months. Monitor for signs/symptoms of malignancy (eg, splenomegaly, hepatomegaly, abdominal pain, persistent fever, night sweats, weight loss).
Pregnancy
Pregnancy Considerations
May cause fetal harm if administered during pregnancy. Case reports of fetal loss have been noted with mercaptopurine administration during the first trimester; adverse effects have also been noted with second and third trimester use. Women of reproductive potential should avoid becoming pregnant during treatment.
Patient Education
What is this drug used for?
- It is used to treat a type of leukemia.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Lack of appetite
- Loss of strength and energy.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating.
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Severe diarrhea
- Severe nausea
- Severe vomiting
- Skin discoloration
- Thrush
- Severe loss of strength and energy
- Shortness of breath
- Severe abdominal pain
- Skin growths
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.