Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Tablet, Oral:
Neptazane: 25 mg [DSC]
Neptazane: 50 mg [DSC] [scored]
Generic: 25 mg, 50 mg
Pharmacology
Mechanism of Action
Noncompetitive inhibition of the enzyme carbonic anhydrase; thought that carbonic anhydrase is located at the luminal border of cells of the proximal tubule. When the enzyme is inhibited, there is an increase in urine volume and a change to an alkaline pH with a subsequent decrease in the excretion of titratable acid and ammonia.
Pharmacokinetics/Pharmacodynamics
Absorption
Slow
Distribution
Vd: 17-23 L
Metabolism
Slowly from GI tract
Excretion
Urine (~25% as unchanged drug)
Onset of Action
Slow in comparison with acetazolamide (2-4 hours); Peak effect: 6-8 hours
Duration of Action
10-18 hours
Half-Life Elimination
~14 hours
Protein Binding
~55%
Use: Labeled Indications
Glaucoma: Treatment of chronic open-angle or secondary glaucoma; short-term therapy of acute angle-closure glaucoma prior to surgery
Contraindications
Marked kidney or liver dysfunction; adrenal gland failure; cirrhosis; hyperchloremic acidosis; hyponatremia; hypokalemia; long-term treatment of angle-closure glaucoma
Dosage and Administration
Dosing: Adult
Glaucoma: Oral: 50 to 100 mg 2 to 3 times/day
Dosing: Geriatric
Refer to adult dosing.
Storage
Store at 20°C to 25°C (68°F to 77°F).
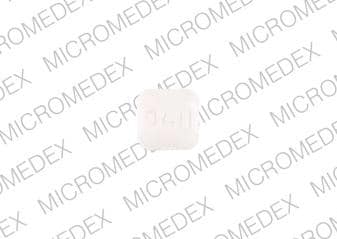
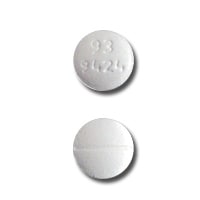
Methazolamide Images
Drug Interactions
Alpha-/Beta-Agonists (Indirect-Acting): Carbonic Anhydrase Inhibitors may increase the serum concentration of Alpha-/Beta-Agonists (Indirect-Acting). Monitor therapy
Amantadine: Carbonic Anhydrase Inhibitors may increase the serum concentration of Amantadine. Monitor therapy
Amphetamines: Carbonic Anhydrase Inhibitors may decrease the excretion of Amphetamines. Monitor therapy
CarBAMazepine: Carbonic Anhydrase Inhibitors may increase the serum concentration of CarBAMazepine. Monitor therapy
Carbonic Anhydrase Inhibitors: May enhance the adverse/toxic effect of other Carbonic Anhydrase Inhibitors. The development of acid-base disorders with concurrent use of ophthalmic and oral carbonic anhydrase inhibitors has been reported. Management: Avoid concurrent use of different carbonic anhydrase inhibitors if possible. Monitor patients closely for the occurrence of kidney stones and with regards to severity of metabolic acidosis. Avoid combination
Diacerein: May enhance the therapeutic effect of Diuretics. Specifically, the risk for dehydration or hypokalemia may be increased. Monitor therapy
Flecainide: Carbonic Anhydrase Inhibitors may increase the serum concentration of Flecainide. Monitor therapy
Fosphenytoin-Phenytoin: Carbonic Anhydrase Inhibitors may enhance the adverse/toxic effect of Fosphenytoin-Phenytoin. Specifically, the risk for osteomalacia or rickets may be increased. Monitor therapy
Lithium: Carbonic Anhydrase Inhibitors may decrease the serum concentration of Lithium. Monitor therapy
Memantine: Carbonic Anhydrase Inhibitors may increase the serum concentration of Memantine. Monitor therapy
MetFORMIN: Carbonic Anhydrase Inhibitors may enhance the adverse/toxic effect of MetFORMIN. Specifically, the risk of developing lactic acidosis may be increased. Monitor therapy
Methenamine: Carbonic Anhydrase Inhibitors may diminish the therapeutic effect of Methenamine. Management: Consider avoiding this combination. Monitor for decreased therapeutic effects of methenamine if used concomitant with a carbonic anhydrase inhibitor. Consider therapy modification
Opioid Agonists: May enhance the adverse/toxic effect of Diuretics. Opioid Agonists may diminish the therapeutic effect of Diuretics. Monitor therapy
Primidone: Carbonic Anhydrase Inhibitors may enhance the adverse/toxic effect of Primidone. Specifically, osteomalacia and rickets. Carbonic Anhydrase Inhibitors may decrease the serum concentration of Primidone. Monitor therapy
QuiNIDine: Carbonic Anhydrase Inhibitors may decrease the excretion of QuiNIDine. Monitor therapy
Salicylates: May enhance the adverse/toxic effect of Carbonic Anhydrase Inhibitors. Salicylate toxicity might be enhanced by this same combination. Management: Avoid these combinations when possible.Dichlorphenamide use with high-dose aspirin as contraindicated. If another combination is used, monitor patients closely for adverse effects. Tachypnea, anorexia, lethargy, and coma have been reported. Consider therapy modification
Sodium Phosphates: Diuretics may enhance the nephrotoxic effect of Sodium Phosphates. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with diuretics, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, hydrate adequately and monitor fluid and renal status. Consider therapy modification
Trientine: Carbonic Anhydrase Inhibitor Diuretics may decrease the serum concentration of Trientine. Monitor therapy
Test Interactions
May lead to false-negative aldosterone/renin ratio (ARR) (Funder 2016)
Adverse Reactions
Frequency not defined.
Central nervous system: Confusion, drowsiness, fatigue, flaccid paralysis, malaise, paresthesia, seizure
Dermatologic: Erythema multiforme, skin photosensitivity, skin rash, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Endocrine & metabolic: Electrolyte disturbance, glycosuria, metabolic acidosis
Gastrointestinal: Decreased appetite, diarrhea, dysgeusia, melena, nausea, vomiting
Genitourinary: Crystalluria, hematuria
Hematologic & oncologic: Agranulocytosis, aplastic anemia, bone marrow depression, hemolytic anemia, immune thrombocytopenia, leukopenia, pancytopenia
Hepatic: Fulminant hepatic necrosis, hepatic insufficiency
Hypersensitivity: Anaphylaxis, hypersensitivity reaction
Ophthalmic: Myopia
Otic: Auditory disturbance, tinnitus
Renal: Nephrolithiasis, polyuria
Miscellaneous: Fever
Warnings/Precautions
Concerns related to adverse effects:
- CNS effects: May impair mental alertness and/or physical coordination.
- Electrolyte disturbance: Initially, potassium excretion may be increased; periodically monitor serum electrolytes and signs of hypokalemia in at risk patients.
- Sulfonamide (“sulfa”) allergy: The FDA-approved product labeling for many medications containing a sulfonamide chemical group includes a broad contraindication in patients with a prior allergic reaction to sulfonamides. There is a potential for cross-reactivity between members of a specific class (eg, two antibiotic sulfonamides). However, concerns for cross-reactivity have previously extended to all compounds containing the sulfonamide structure (SO2NH2). An expanded understanding of allergic mechanisms indicates cross-reactivity between antibiotic sulfonamides and nonantibiotic sulfonamides may not occur or at the very least this potential is extremely low (Brackett 2004; Johnson 2005; Slatore 2004; Tornero 2004). In particular, mechanisms of cross-reaction due to antibody production (anaphylaxis) are unlikely to occur with nonantibiotic sulfonamides. T-cell-mediated (type IV) reactions (eg, maculopapular rash) are less well understood and it is not possible to completely exclude this potential based on current insights. In cases where prior reactions were severe (Stevens-Johnson syndrome/TEN), some clinicians choose to avoid exposure to these classes.
Disease-related concerns:
- Diabetes: Use with caution in patients with prediabetes or diabetes mellitus; may see a change in glucose control.
- Hepatic impairment: Use with caution in patients with hepatic impairment; may precipitate hepatic encephalopathy. Use is contraindicated in patients with marked liver impairment or cirrhosis.
- Respiratory disease: Use with caution in patients with respiratory disease such as emphysema or pulmonary obstruction; may precipitate or aggravate respiratory acidosis.
Concurrent drug therapy issues:
- Aspirin (high dose): Use with caution in patients taking high dose aspirin concurrently; may lead to severe adverse effects including death, coma, tachypnea, anorexia, and lethargy.
Monitoring Parameters
CBC and platelet count (baseline and periodically), serum electrolytes (periodically)
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events were observed in animal reproduction studies.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience nausea, vomiting, diarrhea, change in taste, lack of appetite, fatigue, or loss of strength and energy. Have patient report immediately to prescriber vision changes, trouble hearing, noise or ringing in the ears, burning or numbness feeling, passing a lot of urine, signs of electrolyte problems (mood changes, confusion, muscle pain or weakness, abnormal heartbeat, seizures, lack of appetite, or severe nausea or vomiting), signs of acidosis (confusion, fast breathing, fast heartbeat, abnormal heartbeat, severe abdominal pain, nausea, vomiting, fatigue, shortness of breath, or loss of strength and energy), or signs of a severe sulfonamide reaction (rash; red, swollen, blistered, or peeling skin; red or irritated eyes; mouth, throat, nose, or eye sores; fever, chills, or sore throat; cough that is new or worse; loss of strength and energy; any bruising or bleeding; or signs of liver problems like dark urine, fatigue, lack of appetite, upset stomach or stomach pain, light-colored stools, throwing up, or yellow skin) (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for healthcare professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience and judgment in diagnosing, treating and advising patients.