Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
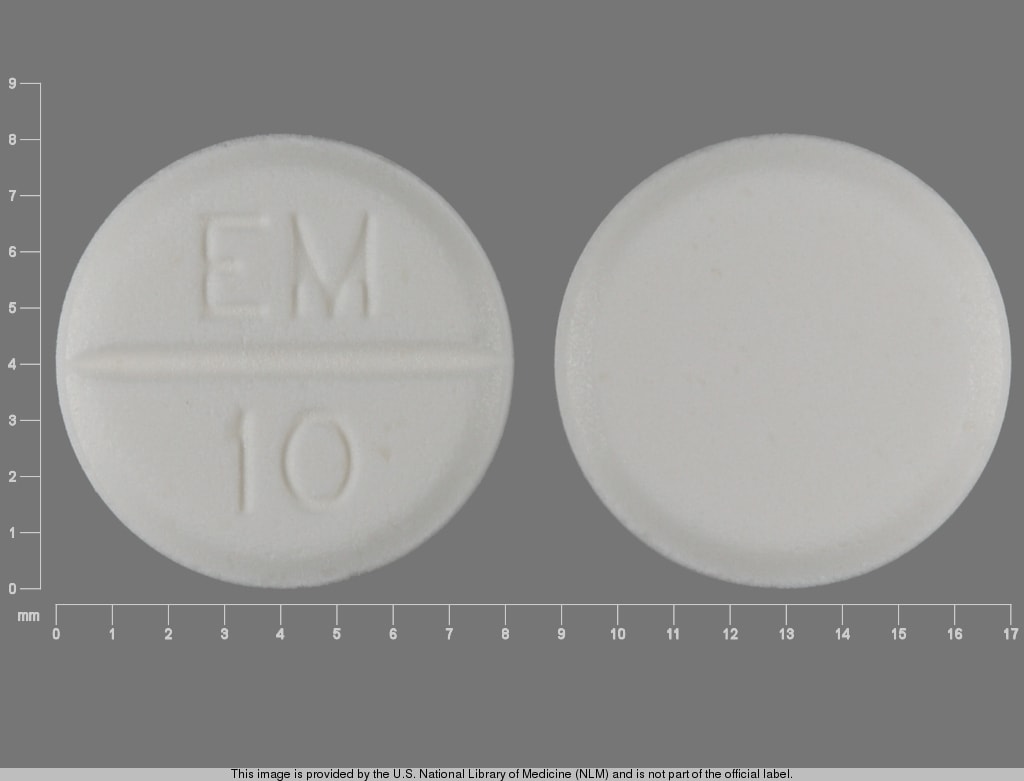
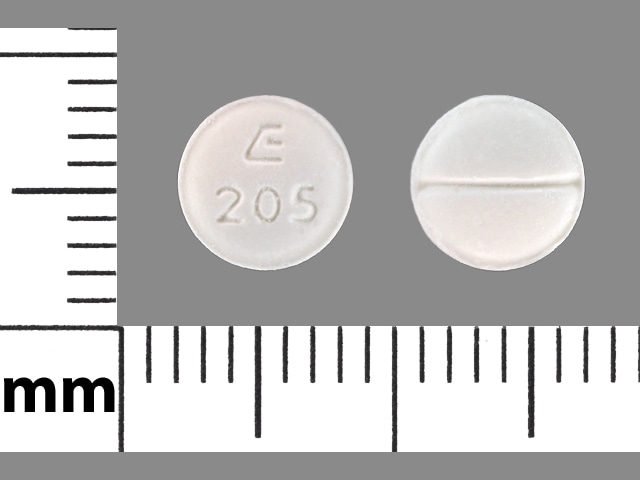
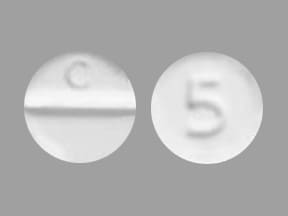
Tablet, Oral:
Tapazole: 5 mg, 10 mg [scored]
Generic: 5 mg, 10 mg
Pharmacology
Mechanism of Action
Inhibits the synthesis of thyroid hormones by blocking the oxidation of iodine in the thyroid gland; blocks synthesis of thyroxine and triiodothyronine (T3); does not inactivate circulating T4 and T3
Pharmacokinetics/Pharmacodynamics
Absorption
Almost complete (Clark 2006)
Distribution
Concentrated in thyroid gland
Metabolism
Hepatic
Excretion
Urine
Onset of Action
Antithyroid: 12 to 18 hours (Clark 2006)
Time to Peak
Serum: 1 to 2 hours (Clark 2006)
Duration of Action
36 to 72 hours (Clark 2006)
Half-Life Elimination
4 to 6 hours (Clark 2006)
Protein Binding
Plasma: None (Cooper 2005)
Use: Labeled Indications
Hyperthyroidism: Treatment of hyperthyroidism in patients with Graves’ disease or toxic multinodular goiter (surgery or radioactive iodine therapy is not appropriate); amelioration of hyperthyroid symptoms in preparation for thyroidectomy or radioactive iodine therapy.
Use: Off Label
Iodine-induced thyrotoxicosisyes
Based on the American Thyroid Association guidelines for the diagnosis and management of Hyperthyroidism and Other Causes of Thyrotoxicosis, treatment with methimazole is recommended in iodine-induced thyrotoxicosis to reduce thyroid hormone production Ross 2016.
Thyroid stormyes
Based on the American Thyroid Association guidelines for the diagnosis and management of Hyperthyroidism and Other Causes of Thyrotoxicosis, treatment with antithyroid therapy is recommended as part of a multimodal approach to the management of thyroid storm (ie, life-threatening thyrotoxicosis). Methimazole reduces thyroid hormone production. Antithyroid agents that also block peripheral conversion of T4 to T3 (eg, propylthiouracil) may be preferred over methimazole in acute settings Ross 2016.
Thyrotoxicosis (type 1 amiodarone-induced)yes
Based on the American Thyroid Association guidelines for the diagnosis and management of Hyperthyroidism and Other Causes of Thyrotoxicosis, treatment with methimazole is recommended in overt thyrotoxicosis (type 1 amiodarone-induced) to reduce thyroid hormone production Ross 2016. Use in combination with a corticosteroid if etiology of thyrotoxicosis (eg type 1 or type 2) cannot be unequivocally determined or if patient is too clinically unstable to allow a trial of monotherapy.
Contraindications
Hypersensitivity to methimazole or any component of the formulation.
Canadian labeling: Additional contraindications (not in US labeling): Breastfeeding, history of acute pancreatitis after administration of methimazole.
Dosage and Administration
Dosing: Adult
Note: Until thyroid levels normalize after initiation of therapy, additional therapy (eg, beta-blockers) may be necessary to control symptoms (Burch 2015).
Hyperthyroidism: Note: In patients with overt hyperthyroidism due to toxic multinodular goiter (TMNG) or toxic adenoma (TA), methimazole may be used temporarily to manage hyperthyroid symptoms prior to more definitive therapy, such as radioactive iodine (RAI) therapy or thyroidectomy. In patients who are not candidates for definitive therapy, chronic low-dose methimazole may be appropriate (Ross 2016).
Oral: Initial: 15 to 60 mg/day depending on severity of disease; usual maintenance dose: 5 to 15 mg/day. Total daily dose may be given as a single dose or in 2 divided doses (for doses >30 mg/day) (Burch 2015; Ross 2016).
Dosage adjustment: Adjust dosage as required to achieve and maintain serum T3, T4, and TSH levels in the normal range. An elevated T3 may be the sole indicator of inadequate treatment (Ross 2016). An elevated TSH indicates excessive antithyroid treatment.
Patients with TMNG or TA undergoing RAI therapy: If methimazole is used prior to RAI therapy, use caution to avoid RAI therapy when TSH levels are normal or elevated (increased risk of hypothyroidism due to destruction of normal thyroid tissue). If needed, may restart methimazole 3 to 7 days after RAI (Ross 2016).
Patients with TMNG or TA undergoing thyroidectomy: Methimazole may be used to achieve euthyroid status prior to surgery. Discontinue methimazole on the day of surgery (Ross 2016).
Hyperthyroidism associated with Graves disease (Ross 2016): Note: Individualize dose based on serum free T4 and T3 levels and clinical status to restore euthyroidism and minimize adverse effects. Adjunctive therapy with potassium iodide may be beneficial in controlling hyperthyroidism and may allow lower initial dosages of methimazole to be used (Sato 2015).
Oral: Initial: 10 to 30 mg once daily; based on free T4 levels, lower doses (eg, 5 mg/day) or higher doses (eg, 40 mg/day) may be considered however initial doses >30 mg/day are associated with increased adverse effects. In patients with severe disease, administering the daily dose in 2 divided doses (eg, 15 to 20 mg twice daily) may increase efficacy (methimazole duration of action may be less than 24 hours).
The following recommendations may be considered to guide initial dosing based on free T4 levels:
1 to 1.5 times ULN: 5 to 10 mg/day
>1.5 to 2 times ULN: 10 to 20 mg/day
>2 times ULN: 30 to 40 mg/day
Usual maintenance (chronic therapy): 5 to 10 mg once daily for a total of 12 to 18 months, then discontinue if thyroid function tests (eg, TSH, thyrotropin receptor antibody [TRAb]) are normal at that time.
Patients undergoing RAI therapy: Discontinue methimazole 2 to 3 days prior to planned RAI; if needed, may restart methimazole 3 to 7 days after RAI, followed by tapering of the dose as thyroid function normalizes.
Patients undergoing thyroidectomy: Discontinue methimazole on the day of surgery.
Iodine-induced thyrotoxicosis (off-label use): Oral: 20 to 40 mg daily given either once or twice daily (Ross 2016)
Thyroid storm (off-label use): Note: Use in combination with other specific agents (eg, beta-blockers, inorganic iodine, corticosteroids). Antithyroid agents that block peripheral conversion of T4 to T3 (eg, propylthiouracil) may be preferred over methimazole in acute settings (Ross 2016).
Oral: Dosages of 20 to 25 mg every 6 hours have been used; once stable, dosing frequency may be reduced to once or twice daily (Nayak 2006). The American Thyroid Association recommends 60 to 80 mg/day (Ross 2016). Rectal administration has also been described (Nabil 1982).
Thyrotoxicosis, type 1 amiodarone-induced (off-label use): Oral: 40 mg once daily to restore euthyroidism (generally 3 to 6 months). If high doses continue to be required, dividing the dose may be more effective. Note: Use in combination with a corticosteroid if etiology of thyrotoxicosis (eg, type 1 or type 2) cannot be unequivocally determined or if patient is too clinically unstable to allow a trial of monotherapy (Ross 2016).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Hyperthyroidism: Infants, Children, and Adolescents: Oral: Initial: 0.4 mg/kg/day in 3 divided doses (approximately every 8 hours); maintenance 0.2 mg/kg/day in 3 divided doses (50% of initial)
Graves disease (ATA [Ross 2016]): Note: In severe cases, higher doses may be required (50% to 100% higher); once patient euthyroid, reduce dose by ≥50% to maintain euthyroid; duration of therapy usually 1 to 2 years
Weight-based dosing: Infants, Children, and Adolescents: Oral: Initial: 0.2 to 0.5 mg/kg/dose once daily (range: 0.1 to 1 mg/kg/dose)
Fixed dosing (using 1/4, 1/2, or whole tablets): Oral:
Infants: 1.25 mg/day
Children 1 to 5 years: 2.5 to 5 mg/day
Children 5 to 10 years: 5 to 10 mg/day
Children ≥10 years and Adolescents: 10 to 20 mg/day
Extemporaneously Prepared
Suppositories can be made from methimazole tablets; dissolve 1200 mg methimazole in 12 mL of water and add to 52 mL cocoa butter containing 2 drops of Span 80. Stir the resulting mixture to form a water-oil emulsion and pour into 2.6 mL suppository molds to cool.
Nabil N, Miner DJ, and Amatruda JM, "Methimazole: An Alternative Route of Administration," J Clin Endo Metab, 1982, 54(1):180-1.7054215
Administration
Rectal: In thyrotoxic crisis, rectal administration has been described (Nabil 1982).
Storage
Store at 15°C to 30°C (59°F to 86°F).
Methimazole Images
Drug Interactions
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Cardiac Glycosides: Antithyroid Agents may increase the serum concentration of Cardiac Glycosides. Monitor therapy
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
PrednisoLONE (Systemic): MethIMAzole may decrease the serum concentration of PrednisoLONE (Systemic). Monitor therapy
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Sodium Iodide I131: Antithyroid Agents may diminish the therapeutic effect of Sodium Iodide I131. Management: Discontinue antithyroid therapy 3-4 days prior to sodium iodide I-131 administration. Avoid combination
Theophylline Derivatives: Antithyroid Agents may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Antithyroid Agents may diminish the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Adverse Reactions
Frequency not defined:
Cardiovascular: Edema, periarteritis
Central nervous system: Drowsiness, drug fever, headache, neuritis, paresthesia, vertigo
Dermatologic: Alopecia, pruritus, skin pigmentation, skin rash, urticaria
Endocrine & metabolic: Hypoglycemic coma, hypothyroidism, insulin autoimmune syndrome
Gastrointestinal: Ageusia, enlargement of salivary glands, epigastric distress, nausea, vomiting
Hematologic & oncologic: Agranulocytosis, aplastic anemia, granulocytopenia, hypoprothrombinemia, leukopenia, lymphadenopathy, thrombocytopenia
Hepatic: Hepatitis, jaundice
Neuromuscular & skeletal: Arthralgia, lupus-like syndrome, myalgia
Renal: Nephritis
Postmarketing: Acute hepatic failure, acute pancreatitis, acute renal injury, cerebral vasculitis, glomerulonephritis, hepatotoxicity, hypersensitivity angiitis, neuropathy, pulmonary alveolar hemorrhage, vasculitis (including ANCA positive)
Warnings/Precautions
Concerns related to adverse effects:
- Bleeding: May cause hypoprothrombinemia and bleeding. Monitoring is recommended, especially before surgical procedures.
- Bone marrow suppression: May cause significant bone marrow depression; the most severe manifestation is agranulocytosis. Aplastic anemia, thrombocytopenia, and leukopenia may also occur. Monitor patients closely; use with caution with concomitant use of other drugs known to cause myelosuppression (particularly agranulocytosis). Instruct patients to report immediately any signs/symptoms of infection (eg, fever, sore throat, pharyngitis, flu-like symptoms) and to discontinue therapy immediately if symptoms suggestive of agranulocytosis are present. A CBC with differential should be performed prior to initiation of therapy, during febrile illness, and at the onset of pharyngitis in all patients during therapy (Ross 2016).
- Dermatologic effects: Antithyroid agents have been associated with dermatologic reactions. Discontinue in the presence of a severe reaction.
- Fever: Discontinue in the presence of unexplained fever.
- Hepatic effects: Hepatotoxicity (including acute liver failure) may occur. Symptoms suggestive of hepatic dysfunction (eg, anorexia, pruritus, right upper quadrant pain) should prompt evaluation. Discontinue in the presence of hepatitis and clinically significant hepatic abnormality, including transaminase >3 times upper limit of normal.
- Hypothyroidism: May cause hypothyroidism; routinely monitor TSH and free T4 levels, adjust dose to maintain euthyroid state.
- Lupus-like syndrome: A lupus-like syndrome may occur.
- Vasculitis: Cases of vasculitis resulting in severe complications have been reported. Most cases were ANCA-positive and included leukocytoclastic cutaneous vasculitis, acute kidney injury and glomerulonephritis, alveolar/pulmonary hemorrhage, CNS vasculitis and neuropathy. Discontinue use for confirmed or suspected vasculitis. Some cases resolve/improve with drug discontinuation; severe cases may require further treatment (eg, corticosteroids, plasmapheresis).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Monitoring Parameters
Signs and symptoms of illness (ie fever, sore throat, skin eruptions, general malaise).
CBC with differential (baseline and if development of febrile illness or pharyngitis occurs); prothrombin time (especially before surgical procedures); LFTs (bilirubin, alkaline phosphatase, ALT, AST) at baseline and if symptoms of liver injury occur (Ross 2016).
Thyroid function tests:
Serum free T4 and total T3 2 to 6 weeks after initiation, repeat in 4 to 6 weeks if dose is adjusted and then every 2 to 3 months once euthyroid levels are achieved (with long-term therapy [ie, >18 months] may extend interval to every 4 to 6 months); in patients with Graves disease, if TRAb is negative, thyroid function tests should be monitored every 2 to 3 months for the first 6 months after discontinuing therapy, then at 4- to 6-month intervals for the next 6 months, then every 6 to 12 months thereafter (Ross 2016).
Thyroid-stimulating hormone (TSH) (periodically throughout treatment; TSH is not an adequate parameter to assess initial response as levels may remain suppressed for several months after starting therapy) (Ross 2016).
TRAb in patients with Graves disease (prior to stopping medication, elevation at the end of therapy decreases likelihood of remission) (Ross 2016).
Pregnancy
Pregnancy Risk Factor
D
Pregnancy Considerations
Methimazole crosses the placenta.
Birth defects have been observed in neonates exposed to maternal methimazole in the first trimester of pregnancy and include anomalies of the upper gastrointestinal tract (esophageal atresia or tracheoesophageal fistula), respiratory tract (choanal atresia), skin (aplasia cutis), and facial dysmorphism. Additional abdominal wall defects (umbilicocele), ventricular septal defects, and defects of the eye and urinary system have also been reported (Alexander 2017). Hypothyroidism may occur in the newborn.
Uncontrolled maternal hyperthyroidism may result in adverse neonatal and maternal outcomes. Antithyroid drugs are the treatment of choice for the control of hyperthyroidism during pregnancy, although recommendations for specific agents vary by guideline (ACOG 2015; Alexander 2017; De Groot 2012). Dose requirements of methimazole may be decreased as pregnancy progresses. To prevent adverse pregnancy outcomes, maternal TT4/FT4 should be at or just above the pregnancy specific upper limit of normal (Alexander 2017).
Patient Education
What is this drug used for?
- It is used to treat an overactive thyroid gland.
Frequently reported side effects of this drug
- Headache
- Itching
- Change in taste
- Fatigue
- Muscle pain
- Joint pain
- Hair loss
- Skin discoloration
- Vomiting
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Lupus like rash on the cheeks or other body parts, sunburn easy, muscle or joint pain, chest pain or shortness of breath, or swelling in the arms or legs.
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating.
- Shortness of breath
- Coughing up blood
- Burning or numbness feeling
- Swollen glands
- Bruising
- Bleeding
- Severe loss of strength and energy
- Edema
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.