Boxed Warning
Experienced physician:
Mitoxantrone should be administered under the supervision of a health care provider experienced in the use of cytotoxic chemotherapy agents.
Appropriate administration:
Mitoxantrone should be given slowly into a freely flowing intravenous (IV) infusion. It must never be given subcutaneously, intramuscularly (IM), or intra-arterially. Severe local tissue damage may occur if there is extravasation during administration. Not for intrathecal use. Severe injury with permanent sequelae can result from intrathecal administration.
Bone marrow suppression:
Except for the treatment of acute nonlymphocytic leukemia, mitoxantrone therapy generally should not be given to patients with baseline neutrophil counts of less than 1,500 cells/mm3. In order to monitor the occurrence of bone marrow suppression (primarily neutropenia, which may be severe and result in infection), it is recommended that frequent peripheral blood cell counts be performed on all patients receiving mitoxantrone.
Cardiotoxicity:
Congestive heart failure (CHF), potentially fatal, may occur during therapy with mitoxantrone or months to years after termination of therapy. Cardiotoxicity risk increases with cumulative mitoxantrone dose and may occur whether or not cardiac risk factors are present. Presence or history of cardiovascular disease, radiotherapy to the mediastinal/pericardial area, previous therapy with other anthracyclines or anthracenediones, or use of other cardiotoxic drugs may increase this risk. In patients with cancer, the risk of symptomatic CHF was estimated to be 2.6% for patients receiving up to a cumulative dose of 140 mg/m2. To mitigate the cardiotoxicity risk with mitoxantrone, consider the following:
All patients should be assessed for cardiac signs and symptoms by history, physical examination, and electrocardiogram (ECG) prior to start of mitoxantrone therapy.
All patients should have baseline quantitative evaluation of left ventricular ejection fraction (LVEF) using appropriate methodology (eg, echocardiogram, multigated radionuclide angiogram [MUGA], magnetic resonance imaging [MRI]).
Multiple sclerosis (MS) patients with a baseline LVEF below the lower limit of normal should not be treated with mitoxantrone.
MS patients should be assessed for cardiac signs and symptoms by history, physical examination, and ECG prior to each dose.
MS patients should undergo quantitative reevaluation of LVEF prior to each dose using the same methodology that was used to assess baseline LVEF. Additional doses of mitoxantrone should not be administered to MS patients who have experienced a drop in LVEF to below the lower limit of normal or a clinically significant reduction in LVEF during mitoxantrone therapy.
MS patients should not receive a cumulative mitoxantrone dose greater than 140 mg/m2.
MS patients should undergo yearly quantitative LVEF evaluation after stopping mitoxantrone to monitor for late-occurring cardiotoxicity.
Secondary leukemia:
Mitoxantrone therapy in patients with MS and in patients with cancer increases the risk of developing secondary acute myeloid leukemia.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Concentrate, Intravenous:
Generic: 20 mg/10 mL (10 mL); 25 mg/12.5 mL (12.5 mL); 30 mg/15 mL (15 mL)
Pharmacology
Mechanism of Action
Mitoxantrone is an anthracenedione, which is related to the anthracyclines. Mitoxantrone intercalates into DNA resulting in cross-links and strand breaks; binds to nucleic acids and inhibits DNA and RNA synthesis by template disordering and steric obstruction; replication is decreased by binding to DNA topoisomerase II and may inhibit the incorporation of uridine into RNA and thymidine into DNA; mitoxantrone is active throughout entire cell cycle (cell-cycle nonspecific).
Pharmacokinetics/Pharmacodynamics
Distribution
Vdss: >1,000 L/m2; Mitoxantrone distributes extensively into kidney, liver, heart, lungs, and bone marrow, but does not cross the blood brain barrier (Perry 2012).
Metabolism
Hepatic
Excretion
Feces (25%); urine (11%; 65% as unchanged drug)
Half-Life Elimination
Terminal: 23 to 215 hours (median: ~75 hours)
Protein Binding
78%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Clearance is reduced in patients with hepatic impairment. The AUC is at least 3 times greater in patients with severe hepatic impairment (bilirubin >3.4 mg/dL) compared to patients with normal hepatic function.
Use: Labeled Indications
Acute myeloid leukemias: Initial treatment (in combination with other agents) of acute nonlymphocytic leukemia (ANLL [includes myelogenous, promyelocytic, monocytic and erythroid leukemias]).
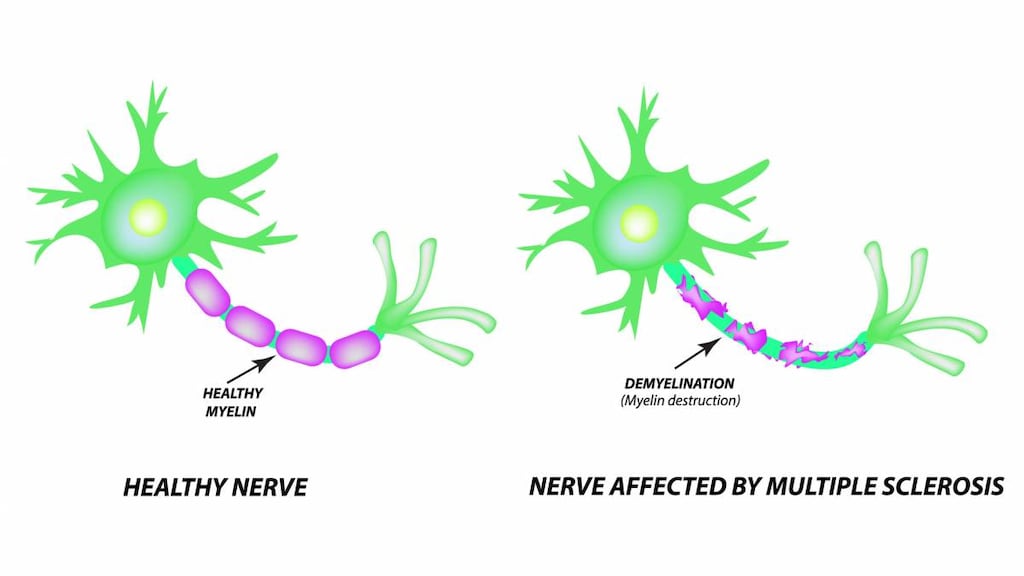
Multiple sclerosis, relapsing or secondary progressive: Treatment of secondary (chronic) progressive, progressive relapsing, or worsening or relapsing-remitting multiple sclerosis (RRMS) to reduce neurologic disability and/or the frequency of clinical relapse.
Limitation of use: Mitoxantrone is not indicated for the treatment of primary progressive MS. Reserve use for rapidly-advancing, refractory multiple sclerosis (AAN [Rae-Grant 2018]; Olek 2019).
Prostate cancer: Treatment of advanced hormone-refractory prostate cancer (in combination with corticosteroids).
Use: Off Label
Acute lymphoblastic leukemia, relapsed/refractoryb
Data from a small phase II study support the use of mitoxantrone (in combination with fludarabine and cytarabine) for salvage treatment of relapsed and refractory acute lymphoblastic leukemia Giebel 2006.
Acute myeloid leukemia, relapsed/refractoryb
Data from a multicenter phase II study support the use of mitoxantrone (in combination with cladribine, cytarabine, and filgrastim [CLAG-M regimen]) as salvage therapy in patients with poor risk relapsed or refractory acute myeloid leukemia (AML) Wierzbowska 2008. Data from a small study suggest that mitoxantrone (in combination with etoposide and cytarabine [MEC regimen]) may be beneficial in salvage treatment of refractory AML Amadori 1991. Data from a phase II study also support the use of mitoxantrone (in combination with etoposide) for the treatment of refractory AML Ho 1988.
Acute promyelocytic leukemia, newly diagnosedb
Data from two multicenter studies support the use of mitoxantrone during the second course of consolidation therapy (in combination with tretinoin [all-trans retinoic acid; ATRA]) in patients with newly diagnosed acute promyelocytic leukemia Ortega 2005, Sanz 2004.
Hematopoietic stem cell transplantation, autologous (conditioning regimen)b
Data from two studies (a phase II study and a retrospective analysis) support the use of mitoxantrone (in combination with melphalan) as a myeloablative conditioning regimen during the transplant phase in patients with relapsed/refractory Hodgkin and non-Hodgkin lymphomas Oyan 2006, Tarella 2001.
Hodgkin lymphomab
Data from a small study supports the use of mitoxantrone (in combination with mesna, ifosfamide, and etoposide [MINE] and alternating with the ESHAP regimen) for the treatment of relapsed or refractory Hodgkin lymphoma Fernandez de Larrea 2010. Data from another study supports the use of mitoxantrone (in combination with vinblastine, cyclophosphamide, procarbazine, etoposide, and bleomycin [VEPEMB regimen]) as a reduced intensity regimen for older adults (>65 years) with newly diagnosed Hodgkin lymphoma Levis 2004.
Non-Hodgkin lymphomas, relapsed/refractoryb
Data from a randomized, multicenter, open-label phase III study supports the use of mitoxantrone (in combination with rituximab, fludarabine and cyclophosphamide [R-FCM regimen]) for the treatment of relapsed and refractory follicular lymphoma Forstpointner 2004. Data from a small phase I-II study supports the use of mitoxantronein combination with rituximab, mesna, ifosfamide, and etoposide [R-MINE regimen]) for the treatment of relapsed, refractory, or poor-risk B-cell lymphomas Joyce 2003.
Contraindications
Hypersensitivity to mitoxantrone or any component of the formulation
Canadian labeling: Additional contraindications (not in the US labeling): Prior hypersensitivity to anthracyclines; prior substantial anthracycline exposure (if abnormal cardiac function prior to initiation of mitoxantrone therapy); presence of severe myelosuppression due to prior chemo- and/or radiotherapy; severe hepatic impairment; intrathecal administration
Dosage and Administration
Dosing: Adult
Acute lymphoblastic leukemia, relapsed/refractory (off-label use; based on limited data): IV: FLAM regimen: 10 mg/m2 on days 3 and 10 (in combination with fludarabine and cytarabine) (Giebel 2006).
Acute myeloid leukemias (AML), initial therapy: IV:
AML induction: 12 mg/m2 once daily for 3 days (in combination with cytarabine); for incomplete response, may repeat (7 to 10 days later) at 12 mg/m2 once daily for 2 days (in combination with cytarabine) (Arlin 1990).
AML consolidation (beginning ~6 weeks after initiation of the final induction course): 12 mg/m2 once daily for 2 days (in combination with cytarabine), repeat in 4 weeks (Arlin 1990).
Acute myeloid leukemia, relapsed/refractory (off-label use): IV:
CLAG-M regimen: 10 mg/m2 once daily for 3 days on days 1, 2, and 3 (in combination with cladribine, cytarabine, and filgrastim), may repeat once if needed (Wierzbowska 2008).
MEC regimen: 6 mg/m2 once daily for 6 days on days 1 to 6 (in combination with cytarabine and etoposide) (Amadori 1991).
Mitoxantrone/Etoposide: 10 mg/m2 once daily for 5 days on days 1 to 5 (in combination with etoposide) (Ho 1988).
Acute promyelocytic leukemia (APL), newly diagnosed (off-label use): IV: Consolidation: 10 mg/m2 once daily for 5 days on days 1 to 5 of consolidation course 2 (in combination with tretinoin all-trans retinoic acid; ATRA) (Sanz 2004).
Hematopoietic stem cell transplantation, autologous (off-label use): Conditioning regimen: IV: 60 mg/m2 administered 4 to 5 days prior to autografting (as 3 divided doses over 1 hour each at 1- to 2-hour intervals on the same day in combination with melphalan) (Oyan 2006; Tarella 2001).
Hodgkin lymphoma (off-label use): IV:
Relapsed or refractory Hodgkin lymphoma: MINE-ESHAP regimen: 10 mg/m2 on day 1 every 28 days for up to 2 cycles (MINE is combination with mesna, ifosfamide, mitoxantrone, and etoposide; MINE alternates with ESHAP for up to 2 cycles of each) (Fernandez de Larrea 2010).
Newly diagnosed Hodgkin lymphoma (reduced intensity regimen): Adults ≥66 years: VEPEMB regimen: 6 mg/m2 on day 15 every 28 days (in combination with vinblastine, cyclophosphamide, procarbazine, etoposide, and bleomycin) for 3 to 6 cycles (Levis 2004).
Non-Hodgkin lymphomas, relapsed/refractory (off-label use): IV:
B-cell lymphomas: R-MINE regimen: 8 mg/m2 on day 1 (in combination with rituximab, mesna, ifosfamide, and etoposide) for up to 3 cycles (Joyce 2003).
Follicular lymphoma: R-FCM regimen: 8 mg/m2 on day 1 every 28 days (in combination with rituximab, fludarabine, and cyclophosphamide) for 4 cycles (Forstpointner 2004).
Multiple sclerosis, relapsing or secondary progressive (alternative agent): IV: 12 mg/m2 every 3 months (maximum lifetime cumulative dose: 140 mg/m2; discontinue with LVEF <50% or clinically significant reduction in LVEF). Note: Reserve use for rapidly advancing, refractory multiple sclerosis (AAN [Rae-Grant 2018]; Olek 2019).
Prostate cancer (advanced, hormone-refractory): IV: 12 mg/m2 once every 3 weeks (in combination with prednisone or prednisolone) for up to 10 cycles (Tannock 2004) or 12 to 14 mg/m2 once every 3 weeks (in combination with prednisone) until disease progression or unacceptable toxicity, up to a maximum cumulative mitoxantrone dose of 144 mg/m2 (Petrylak 2004).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dosing regimens may vary by dose, cycles, and combination therapy; refer to individual protocols. Mitoxantrone is associated with a low emetic potential (Dupuis 2011); antiemetics are recommended to prevent nausea and vomiting (Dupuis 2013).
Acute lymphocytic leukemia (ALL), relapsed: Limited data available: Children and Adolescents: Induction: 10 mg/m2/dose once daily on days 1 and 2 (in combination with dexamethasone, vincristine, pegaspargase, and intrathecal methotrexate), with follow-up therapy (allogeneic stem cell transplant or continued chemotherapy) determined by risk stratification (Parker 2010)
Acute myeloid leukemia (AML): Limited data available:
Gamis 2014: Infants, Children, and Adolescents: Note: Some aspects of protocol dosing presented in previous reports (Cooper 2012)
Intensification Course 2:
BSA <0.6 m2: IV: 0.4 mg/kg once daily for 4 days on Days 3 to 6 of a 28-day cycle (in combination with cytarabine)
BSA ≥0.6 m2: IV: 12 mg/m2 once daily for 4 days on Days 3 to 6 of a 28-day cycle (in combination with cytarabine)
Perel 2002: LAME 89/91 regimen: Infants, Children, and Adolescents:
Remission Induction:
<1 year: IV: 8 mg/m2 once daily for 5 days (in combination with cytarabine); if persistent disease, additional course of 8 mg/m2 for 2 days (in combination with cytarabine) was administered
≥1 year: IV: 12 mg/m2 once daily for 5 days (in combination with cytarabine); if persistent disease, additional course of 12 mg/m2 for 2 days (in combination with cytarabine) was administered
Gibson 2011: MAE and MidAC regimens:
Induction Course 1 (MAE 3+10+5) or Course 2 (MAE 3+8+5):
Infants: IV: 9 mg/m2 once daily on Days 1, 3, and 5 (in combination with cytarabine and etoposide)
Children and Adolescents <17 years: IV: 12 mg/m2 once daily on Days 1, 3, and 5 (in combination with cytarabine and etoposide)
Consolidation Course 4/5 (MidAC):
Infants: IV: 7.5 mg/m2 once daily on Days 1 to 5 (in combination with cytarabine)
Children and Adolescents <17 years: IV: 10 mg/m2 once daily on Days 1 to 5 (in combination with cytarabine)
Acute promyelocytic leukemia (APL): Limited data available: Consolidation Course 2: Children ≥2 years and Adolescents: IV: 10 mg/m2 once daily for 5 days of a 28-day cycle (combined with tretinoin [ATRA]) (Ortega 2005; Sanz 2004)
Dosing adjustment for toxicity: The presented dosing adjustments are based on experience in adult patients; specific recommendations for pediatric patients are limited. Refer to specific protocol for management in pediatric patients if available.
Adult:
Oncology uses: Severe or life-threatening nonhematologic toxicity: Withhold treatment until toxicity resolves
Multiple sclerosis:
Neutrophils <1,500/mm3: Use is not recommended
Signs/symptoms of HF: Evaluate for cardiac signs/symptoms and monitor LVEF
LVEF <50% or baseline LVEF below the lower limit of normal (LLN): Use is not recommended
Dosing: Adjustment for Toxicity
AML: Severe or life-threatening nonhematologic toxicity: Withhold treatment until toxicity resolves.
MS:
Neutrophils <1,500/mm3: Use is not recommended.
Signs/symptoms of HF: Evaluate for cardiac signs/symptoms and monitor LVEF.
LVEF <50% or baseline LVEF below the lower limit of normal (LLN): Use is not recommended.
Dosing: Obesity
ASCO Guidelines for appropriate chemotherapy dosing in obese adults with cancer (excludes HSCT dosing): Utilize patient's actual body weight (full weight) for calculation of body surface area- or weight-based dosing, particularly when the intent of therapy is curative; manage regimen-related toxicities in the same manner as for nonobese patients; if a dose reduction is utilized due to toxicity, consider resumption of full weight-based dosing with subsequent cycles, especially if cause of toxicity (eg, hepatic or renal impairment) is resolved (Griggs 2012).
Reconstitution
Dilute in at least 50 mL of NS or D5W. May further dilute in D5W, NS, or D5NS, use immediately after preparation.
Administration
IV: For IV administration only; do not administer intrathecally, subcutaneously, intramuscularly, or intra-arterially. Must be diluted prior to use. Usually administered as a short IV infusion over 5 to 15 minutes; do not infuse over less than 3 to 5 minutes.
Mitoxantrone was infused over 20 to 30 minutes in some (off-label) regimens; refer to protocol for infusion details. High doses for bone marrow transplant (off-label use) are usually given as 3 divided doses over 1 hour each at 1-to 2-hour intervals on the same day (Oyan 2006; Tarella 2001).
Irritant with vesicant-like properties; ensure proper needle or catheter placement prior to and during infusion; avoid extravasation.
Extravasation management: If extravasation occurs, stop infusion immediately and disconnect (leave cannula/needle in place); gently aspirate extravasated solution (do NOT flush the line); remove needle/cannula; elevate extremity. Initiate antidote (dexrazoxane or dimethyl sulfate [DMSO]). Apply dry cold compresses for 20 minutes 4 times daily for 1 to 2 days (Pérez Fidalgo 2012); withhold cooling beginning 15 minutes before dexrazoxane infusion; continue withholding cooling until 15 minutes after infusion is completed. Topical DMSO should not be administered in combination with dexrazoxane; may lessen dexrazoxane efficacy.
Dexrazoxane: 1,000 mg/m2 (maximum dose: 2,000 mg) IV (administer in a large vein remote from site of extravasation) over 1 to 2 hours days 1 and 2, then 500 mg/m2 (maximum dose: 1,000 mg) IV over 1 to 2 hours day 3; begin within 6 hours of extravasation. Day 2 and day 3 doses should be administered at approximately the same time (±3 hours) as the dose on day 1 (Mouridsen 2007; Pérez Fidalgo 2012). Note: Reduce dexrazoxane dose by 50% in patients with moderate to severe renal impairment (CrCl <40 mL/minute).
DMSO: Apply topically to a region covering twice the affected area every 8 hours for 7 days; begin within 10 minutes of extravasation; do not cover with a dressing (Pérez Fidalgo 2012).
Storage
Store intact vials at 15°C to 25°C (59°F to 77°F); do not freeze. Opened vials may be stored at room temperature for 7 days or under refrigeration for up to 14 days. Solutions diluted in D5W or NS for administration are stable for 7 days at room temperature or under refrigeration, although the manufacturer recommends immediate use.
Drug Interactions
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
CycloSPORINE (Systemic): May increase the serum concentration of MitoXANTRONE. Management: Consider mitoxantrone dose reduction, as clinically appropriate, when used with cyclosporine. Use this combination with caution and monitor closely for toxic effects of mitoxantrone. Consider therapy modification
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Lenograstim: Antineoplastic Agents may diminish the therapeutic effect of Lenograstim. Management: Avoid the use of lenograstim 24 hours before until 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Lipegfilgrastim: Antineoplastic Agents may diminish the therapeutic effect of Lipegfilgrastim. Management: Avoid concomitant use of lipegfilgrastim and myelosuppressive cytotoxic chemotherapy. Lipegfilgrastim should be administered at least 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Palifermin: May enhance the adverse/toxic effect of Antineoplastic Agents. Specifically, the duration and severity of oral mucositis may be increased. Management: Do not administer palifermin within 24 hours before, during infusion of, or within 24 hours after administration of myelotoxic chemotherapy. Consider therapy modification
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Adverse Reactions
Includes events reported with any indication; incidence varies based on treatment, dose, and/or concomitant medications.
>10%:
Cardiovascular: Edema (10% to 30%), cardiac disease (≤18%), cardiac arrhythmia (3% to 18%), ECG changes (≤11%)
Central nervous system: Pain (8% to 41%), fatigue (≤39%), headache (6% to 13%)
Dermatologic: Alopecia (20% to 61%), nail bed changes (≤11%)
Endocrine & metabolic: Menstrual disease (26% to 61%), amenorrhea (28% to 53%), hyperglycemia (10% to 31%), weight gain (≤17%), weight loss (≤17%), increased gamma-glutamyl transferase (3% to 15%)
Gastrointestinal: Nausea (26% to 76%), vomiting (6% to 72%), diarrhea (14% to 47%), mucositis (10% to 29%; onset: ≤1 week), stomatitis (8% to 29%; onset: ≤1 week), anorexia (22% to 25%), constipation (10% to 16%), gastrointestinal hemorrhage (2% to 16%), abdominal pain (9% to 15%), dyspepsia (5% to 14%)
Genitourinary: Urinary tract infection (7% to 32%), hematuria (≤11%), urine abnormality (5% to 11%)
Hematologic & oncologic: Neutropenia (79% to 100%; onset: ≤3 weeks; grade 4: 23% to 54%), leukopenia (9% to 100%), lymphocytopenia (72% to 95%), anemia (≤75%), decreased hemoglobin (≤75%), thrombocytopenia (33% to 39%; grades 3/4: 3% to 4%), bruise (≤11%), febrile neutropenia (≤11%), petechia (≤11%)
Hepatic: Increased serum alkaline phosphatase (≤37%), increased serum transaminases (5% to 20%)
Infection: Infection (4% to 60%), sepsis (≤34%), fungal infection (9% to 15%)
Neuromuscular & skeletal: Weakness (≤24%)
Renal: Increased blood urea nitrogen (≤22%), increased serum creatinine (≤13%)
Respiratory: Upper respiratory tract infection (7% to 53%), pharyngitis (≤19%), dyspnea (6% to 18%), cough (5% to 13%)
Miscellaneous: Fever (6% to 78%)
1% to 10%:
Cardiovascular: Cardiac failure (≤5%), ischemia (≤5%), decreased left ventricular ejection fraction (≤5%), hypertension (≤4%)
Central nervous system: Chills (≤5%), anxiety (5%), depression (5%), seizure (2% to 4%)
Dermatologic: Diaphoresis (≤9%), skin infection (≤5%)
Endocrine & metabolic: Hypocalcemia (10%), hypokalemia (7% to 10%), hyponatremia (9%), hypermenorrhea (7%)
Gastrointestinal: Aphthous stomatitis (≤10%)
Genitourinary: Impotence (≤7%), proteinuria (≤6%), sterility (≤5%)
Hematologic & oncologic: Granulocytopenia (6%), hemorrhage (5% to 6%), acute leukemia (≤3%; secondary; includes AML, APL)
Hepatic: Jaundice (3% to 7%)
Infection: Fungal infection (cutaneous: ≤10%)
Neuromuscular & skeletal: Back pain (6% to 8%), arthralgia (≤5%), myalgia (≤5%)
Ophthalmic: Conjunctivitis (≤5%), blurred vision (≤3%)
Renal: Renal failure (≤8%)
Respiratory: Rhinitis (10%), pneumonia (≤9%), sinusitis (≤6%)
<1%, postmarketing, and/or case reports: Anaphylactoid reaction, anaphylaxis, chest pain, dehydration, hypersensitivity reaction, interstitial pneumonitis (with combination chemotherapy), hyperuricemia, hypotension, ocular discoloration (blue discoloration of sclera), phlebitis (at infusion site), skin rash, tachycardia, urine discoloration (blue-green), urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: Mitoxantrone may lead to severe myelosuppression (at any dose). [US Boxed Warning]: Usually should not be administered if baseline neutrophil count <1,500/mm3 (except for in the treatment of AML). Monitor blood counts frequently and monitor for infection due to neutropenia. Unless the expected benefit outweighs the risk, mitoxantrone is generally not recommended in patients with preexisting myelosuppression due to prior chemotherapy.
- Extravasation: Mitoxantrone is an irritant with vesicant-like properties. [US Boxed Warning]: For IV administration only into a free-flowing IV; may cause severe local tissue damage if extravasation occurs. Extravasation resulting in burning, erythema, pain, swelling, and skin discoloration (blue) has been reported; may result in tissue necrosis and require debridement for skin graft. Ensure proper needle or catheter placement prior to and during infusion. Avoid extravasation.
- Hypersensitivity: May contain sodium metabisulfite, which is associated with allergic-type reactions (including anaphylactic symptoms and potentially severe asthmatic episodes). The risk for hypersensitivity is higher in patients with asthma.
- Myocardial toxicity: [US Boxed Warning]: May cause myocardial toxicity and potentially fatal heart failure (HF); risk increases with cumulative dosing. Cardiotoxicity may occur during therapy or may be delayed (months or years after completion of therapy). Predisposing factors for mitoxantrone-induced cardiotoxicity include prior anthracycline or anthracenedione therapy, prior or current cardiovascular disease, concomitant use of cardiotoxic drugs, and mediastinal/pericardial irradiation, although may also occur in patients without risk factors. Prior to therapy initiation, evaluate all patients for cardiac-related signs/symptoms, including history, physical exam, and ECG; and evaluate baseline left ventricular ejection fraction (LVEF) with echocardiogram or multigated radionuclide angiography (MUGA) or MRI. Mitoxantrone is not recommended for use in MS patients when baseline LVEF below the lower limit of normal (LLN). Evaluate for cardiac signs/symptoms (by history, physical exam, and ECG) and evaluate LVEF (using same method as baseline LVEF) in MS patients prior to each dose. Patients with MS should not receive a cumulative dose of >140 mg/m2. Do not administer mitoxantrone if LVEF falls below LLN or if a significant decrease in LVEF is observed during treatment. Patients with MS should undergo annual LVEF evaluation following discontinuation of therapy to monitor for delayed cardiotoxicity. Evaluate potential risk versus benefit in patients who have previously received anthracycline therapy. If signs/symptoms of heart failure develop, evaluate LVEF and ECG.
- Secondary malignancy: [US Boxed Warning]: Treatment with mitoxantrone increases the risk of developing secondary acute myeloid leukemia (AML) in patients with cancer and in patients with MS; acute promyelocytic leukemia (APL) has also been observed. Symptoms of acute leukemia include excessive bruising, bleeding and recurrent infections. The risk for secondary leukemia is increased in patients who are heavily pretreated, with higher doses, and/or with combination chemotherapy.
- Tumor lysis syndrome: Rapid lysis of tumor cells may lead to hyperuricemia and tumor lysis syndrome. Monitor uric acid and administer antihyperuricemic therapy and aggressive hydration as indicated.
Disease-related concerns:
- Hepatic impairment: Clearance is reduced in patients with hepatic impairment; use with caution; dosage adjustment recommended. Not for treatment of multiple sclerosis in patients with concurrent hepatic impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate administration: [US Boxed Warning]: For IV administration only; do not administer subcutaneously, intramuscularly, or intra-arterially. Do not administer intrathecally; may cause serious and permanent neurologic damage.
- Blue-green coloration: May cause urine, saliva, tears, and sweat to turn blue-green for 24 hours postinfusion; whites of eyes may have blue-green tinge.
- Experienced physician: [US Boxed Warning]: Should be administered under the supervision of a physician experienced in cancer chemotherapy agents.
Monitoring Parameters
CBC with differential, serum uric acid (for leukemia treatment), liver function tests; for the treatment of multiple sclerosis, obtain pregnancy test (prior to treatment in females of reproductive potential; prior to each dose in females with MS); monitor injection site for extravasation.
Cardiac monitoring: Prior to initiation, evaluate all patients for cardiac-related signs/symptoms, including history, physical exam, and ECG; evaluate baseline and periodic left ventricular ejection fraction (LVEF) with echocardiogram or multigated radionuclide angiography (MUGA) or MRI. In patients with MS, evaluate for cardiac signs/symptoms (by history, physical exam, and ECG) and evaluate LVEF (using same method as baseline LVEF) prior to each dose and if signs/symptoms of HF develop. Patients with MS should undergo annual LVEF evaluation following discontinuation of therapy to monitor for delayed cardiotoxicity.
Pregnancy
Pregnancy Considerations
Based on the mechanism of action and adverse events observed in animal reproduction studies, mitoxantrone may cause fetal harm if administered during pregnancy. Information related to pregnancy outcomes following maternal use of mitoxantrone in pregnancy is limited (Amato 2015; Frau 2018; Houtchens 2013; NTP 2013).
In general, disease-modifying therapies for multiple sclerosis (MS) are stopped prior to a planned pregnancy, and not initiated during pregnancy, except in females at high risk of MS activity (AAN [Rae-Grant 2018]). Consider use of agents other than mitoxantrone for females at high risk of disease reactivation who are planning a pregnancy. Delaying pregnancy is recommended for females with persistent high disease activity; when disease-modifying therapy is needed in these patients, other agents are preferred (ECTRIMS/EAN [Montalban 2018]).
The European Society for Medical Oncology has published guidelines for diagnosis, treatment, and follow-up of cancer during pregnancy. The guidelines recommend referral to a facility with expertise in cancer during pregnancy and encourage a multidisciplinary team (obstetrician, neonatologist, oncology team). In general, if chemotherapy is indicated, it should be avoided in the first trimester, there should be a 3-week time period between the last chemotherapy dose and anticipated delivery, and chemotherapy should not be administered beyond week 33 of gestation (Peccatori 2013).
Pregnancy status should be evaluated prior to treatment in females of reproductive potential. Mitoxantrone is associated with amenorrhea, ovarian failure, and male infertility (AAN [Rae-Grant 2018]).
Patient Education
What is this drug used for?
- It is used to treat prostate cancer.
- It is used to treat a type of leukemia.
- It is used to treat MS (multiple sclerosis).
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Blue or green urine
- Eye discoloration
- Nausea
- Vomiting
- Abdominal pain
- Diarrhea
- Constipation
- Lack of appetite
- Headache
- Mouth irritation
- Mouth sores
- Common cold symptoms
- Hair loss
- Back pain
- No menstrual periods
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Heart problems like cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out
- Infection
- Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding
- Excessive weight loss
- Yellow skin
- Severe loss of strength and energy
- Bone pain
- Night sweats
- Blue/gray skin discoloration
- Severe injection site redness, pain, swelling, or irritation
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.