Dosage Forms
Tablet, oral
Generic: 2 mg [500s] [contains lactose, sodium lauryl sulfate]
Pharmacology
Mechanism of Action
Moxidectin, an anthelminthic agent, is active against the microfilariae of O. volvulus, but not effective in killing the adult worms. Studies with other nematodes suggest moxidectin binds to glutamate-gated chloride ions channels, gamma-aminobutyric acid (GABA) receptors, and/or APT-binding cassette transporters. This leads to increased permeability, influx of chloride ions, hyperpolarization, and muscle paralysis. There is also a reduction in motility of all stages of the parasite, excretion of immunomodulatory proteins, and the fertility of both male and female adult worms.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: 2,421 ± 1,658 L
Metabolism
Minimal
Excretion
Feces: 2% (as unchanged drug)
Time to Peak
4 hours
Half-Life Elimination
23.3 days (559 hours)
Protein Binding
Unknown
Use: Labeled Indications
Onchocerciasis: Treatment of onchocerciasis due to Onchocerca volvulus in patients ≥12 years of age.
Limitations of use: Moxidectin does not kill adult O. volvulus; follow-up evaluation is advised. Safety and efficacy of repeat administration of moxidectin in patients with O. volvulus has not been studied.
Contraindications
There are no contraindications listed in the manufacturer’s labeling.
Dosage and Administration
Dosing: Adult
Onchocerciasis: Oral: 8 mg as a single dose
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Onchocerciasis: Children ≥12 years and Adolescents: Oral: 8 mg as a single dose
Administration
Oral: Administer without regard to meals.
Storage
Store below 30°C (86°F). Protect from light. Once opened, administer within 24 hours. Discard unused tablets.
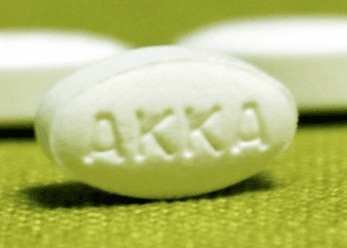
Moxidectin Images
Drug Interactions
There are no known significant interactions.
Adverse Reactions
>10%:
Cardiovascular: Tachycardia (39%), postural orthostatic tachycardia (34%), hypotension (30%), orthostatic hypotension (22%), peripheral edema (11%)
Central nervous system: Headache (58%), chills (≤27%), lymph node pain (13%), dizziness (12%)
Dermatologic: Pruritus (65%), skin rash (37%)
Endocrine & metabolic: Hyponatremia (12%)
Gastrointestinal: Abdominal pain (31%), diarrhea (≤15%), enteritis (≤15%), gastroenteritis (≤15%)
Hematologic & oncologic: Eosinophilia (18% to 74%; severe: 18%), lymphocytopenia (48%: grade 3: 23%), leukocytosis (25%), neutropenia (20%: grade 4: 7%)
Neuromuscular & skeletal: Musculoskeletal pain (64%)
Respiratory: Flu-like symptoms (23%), cough (17%)
Miscellaneous: Fever (≤27%)
1% to 10%:
Cardiovascular: Symptomatic orthostatic hypotension (5%)
Endocrine & metabolic: Increased gamma-glutamyl transferase (3%)
Hematologic & oncologic: Eosinopenia (5%)
Hepatic: Hyperbilirubinemia (3%), increased serum alanine aminotransferase (1%), increased serum aspartate aminotransferase (1%)
Ophthalmic: Eye pain (8%), eye pruritus (7%), visual impairment (3%; including blurred vision, low vision acuity), allergic conjunctivitis (2%), eyelid edema (2%), conjunctival hyperemia (≤2%), ocular hyperemia (≤2%), increased lacrimation (1%)
Frequency not defined: Dermatologic: Mazzotti reaction
Warnings/Precautions
Concerns related to adverse effects:
- Mazzoti reaction: Moxidectin treatment may cause cutaneous, ophthalmological, and/or systemic reactions (Mazzoti reaction) of varying severity, due to allergic and inflammatory host responses to the death of microfilariae. These reactions generally occur and resolve in the first week post-treatment. Risk may be increased in patients with higher microfilarial burden. Treatment of severe Mazzoti reactions is not definitive, but includes supportive care (eg, hydration and/or parenteral corticosteroids) to treat postural hypotension. Antihistamines and/or aspirin have been used for most mild to moderate reactions.
- Orthostatic hypotension: Orthostatic hypotension may occur, most commonly on the first 1 to 2 days after treatment. Decrease in blood pressure was transient and managed by resuming recumbency.
Disease-related concerns:
- Loiasis: Pretreatment assessment for loiasis is recommended in any patient with exposure to Loa loa-endemic areas; serious, sometimes fatal, encephalopathy may occur following treatment with moxidectin in onchocerciasis patients with concomitant loiasis.
Other warnings/precautions:
- Hyperreactive onchodermatitis: Patients with hyperreactive dermatitis (sowda) may be at increased risk for severe edema and worsening of onchodermatitis following treatment with moxidectin.
Monitoring Parameters
Skin microfilarial counts; screening for loiasis prior to treatment in patients exposed to Loa loa-endemic areas; signs and symptoms of Mazzotti reaction, including symptomatic orthostatic hypotension
Pregnancy
Pregnancy Considerations
Adverse events were observed in some animal reproduction studies.
Females of reproductive potential were required to use long acting contraception during clinical studies (Awadzi 2014; Korth-Bradley 2011) likely due to the long terminal half-life of moxidectin.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience abdominal pain, diarrhea, or cough. Have patient report immediately to prescriber signs of low sodium (headache, difficulty focusing, trouble with memory, confusion, weakness, seizures, or change in balance), signs of infection, itching, headache, flu-like symptoms, dizziness, passing out, fast heartbeat, swollen glands, muscle pain, joint pain, chills, weakness, burning or numbness feeling, eye redness, eye pain, eye itching, eye edema, blurred vision, watery eyes, light sensitivity, or edema (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.