Boxed Warning
Serious adverse reactions:
Fluoroquinolones have been associated with disabling and potentially irreversible serious adverse reactions that have occurred together, including tendinitis and tendon rupture, peripheral neuropathy, and CNS effects. Discontinue moxifloxacin immediately and avoid the use of fluoroquinolones in patients who experience any of these serious adverse reactions. Because fluoroquinolones have been associated with serious adverse reactions, reserve moxifloxacin for use in patients who have no alternative treatment options for the following indications: acute bacterial sinusitis and acute bacterial exacerbation of chronic bronchitis.
Myasthenia gravis:
Fluoroquinolones may exacerbate muscle weakness in persons with myasthenia gravis. Avoid moxifloxacin in patients with known history of myasthenia gravis.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Intravenous [preservative free]:
Avelox: 400 mg/250 mL (250 mL [DSC]) [latex free]
Avelox: 400 mg/250 mL (250 mL)
Generic: 400 mg/250 mL (250 mL)
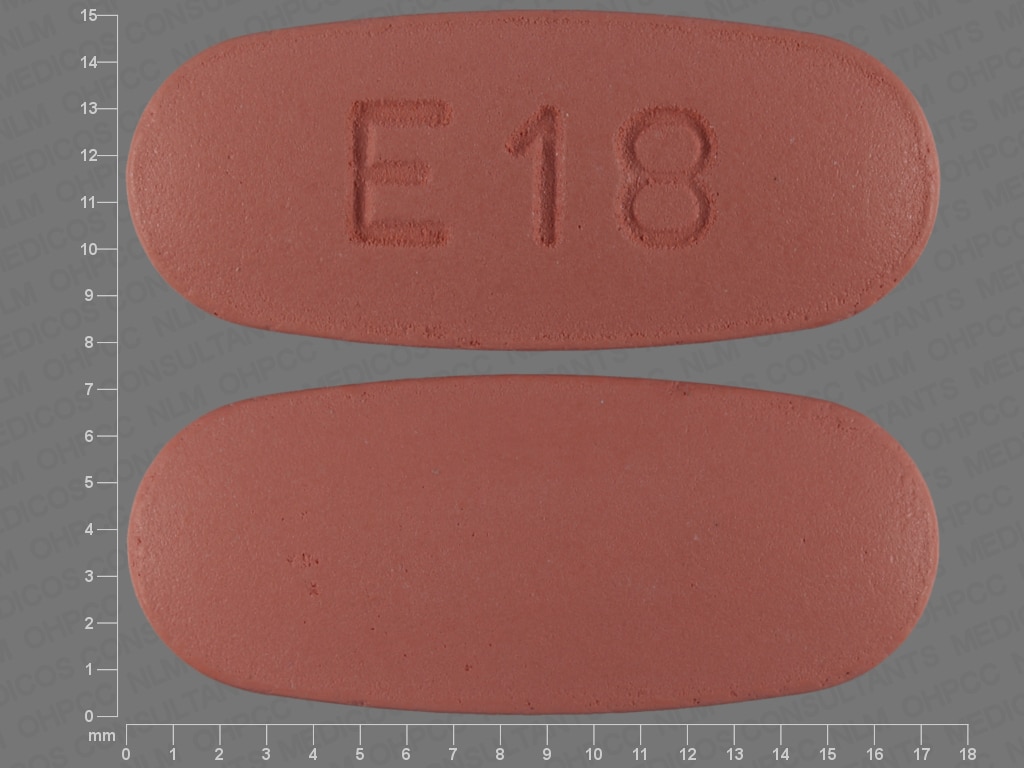
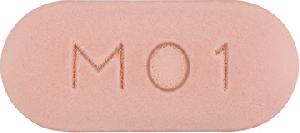
Tablet, Oral:
Avelox: 400 mg [DSC]
Avelox ABC Pack: 400 mg [DSC]
Generic: 400 mg
Pharmacology
Mechanism of Action
Moxifloxacin is a DNA gyrase inhibitor, and also inhibits topoisomerase IV. DNA gyrase (topoisomerase II) is an essential bacterial enzyme that maintains the superhelical structure of DNA. DNA gyrase is required for DNA replication and transcription, DNA repair, recombination, and transposition; inhibition is bactericidal.
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed; not affected by high-fat meal or yogurt
Distribution
Vd: 1.7 to 2.7 L/kg; tissue concentrations often exceed plasma concentrations in respiratory tissues, alveolar macrophages, abdominal tissues/fluids, uterine tissue (endometrium, myometrium), and sinus tissues
Metabolism
Hepatic (~52% of dose) via glucuronide (~14%) and sulfate (~38%) conjugation
Excretion
Urine (as unchanged drug [20%] and glucuronide conjugates); feces (as unchanged drug [25%] and sulfate conjugates)
Half-Life Elimination
Single dose: Oral: 12-16 hours; IV: 8-15 hours
Protein Binding
~30% to 50%
Use: Labeled Indications
Treatment of mild to moderate community-acquired pneumonia, including multidrug-resistant Streptococcus pneumoniae (MDRSP); acute bacterial exacerbation of chronic bronchitis; acute bacterial rhinosinusitis; complicated and uncomplicated skin and skin structure infections; complicated intra-abdominal infections; prophylaxis and treatment of plague, including pneumonic and septicemic plague, due to Yersinia pestis.
Limitations of use: Because fluoroquinolones have been associated with disabling and potentially irreversible serious adverse reactions (eg, tendinitis and tendon rupture, peripheral neuropathy, CNS effects), reserve moxifloxacin for use in patients who have no alternative treatment options for acute exacerbation of chronic bronchitis or acute sinusitis.
Use: Off Label
Anthraxyes
Based on the Centers for Disease Control and Prevention (CDC) Expert Panel Meetings on Prevention and Treatment of Anthrax in Adults, moxifloxacin is as an effective and recommended agent for the treatment of cutaneous anthrax and an alternative agent for postexposure prophylaxis and treatment of systemic anthrax (with or without possible/confirmed meningitis).
Bite wounds (animal/human)yes
Based on the Infectious Diseases Society of America (IDSA) guidelines for the diagnosis and management of skin and soft tissue infections (SSTI), moxifloxacin is an effective and recommended alternative option for treatment of bite wounds, particularly in patients with a human bite wound who are hypersensitive to beta-lactams.
Diabetic foot infectionsyes
Based on the Infectious Diseases Society of America (IDSA) guidelines for diagnosis and treatment of diabetic foot infections, moxifloxacin is an effective and recommended treatment option for moderate to severe diabetic foot infections.
Meningitis, bacterialyes
Based on the Infectious Diseases Society of America (IDSA) guidelines for the management of bacterial meningitis and health care-associated ventriculitis and meningitis, moxifloxacin is an effective and recommended alternative agent for the treatment of meningitis caused by penicillin- and cephalosporin-resistant Streptococcus pneumoniae.
Mycoplasma genitaliumcyes
Noncontrolled trials support the use of moxifloxacin as alternative treatment in patients with persistent detection of Mycoplasma genitalium who have not responded to or are intolerant of azithromycin.
Centers for Disease Control and Prevention (CDC) guidelines for treatment of sexually transmitted diseases (STDs) state that moxifloxacin is the preferred second-line agent for urethritis, cervicitis, or pelvic inflammatory disease (PID) in patients resistant to azithromycin and/or with persistent detection of M. genitalium.
Nocardiosisyes
Data from a limited number of patients studied suggest that moxifloxacin, with or without other antimicrobials, may be beneficial for the treatment of infections caused by susceptible Nocardia spp. Fihman 2006, Kandasamy 2008, Tripodi 2011. Additional data may be necessary to further define the role of moxifloxacin in this condition.
Pelvic inflammatory diseaseyes
Based on the Centers for Disease Control and Prevention (CDC) sexually transmitted diseases treatment guidelines, moxifloxacin may be considered as alternative treatment in patients allergic to cephalosporins with pelvic inflammatory disease. The CDC recommends use as an alternative therapy only if standard parenteral cephalosporin therapy is not feasible and community prevalence of quinolone-resistant gonococcal organisms is low. Culture sensitivity must be confirmed.
Surgical prophylaxisyes
Based on the American Society of Health-System Pharmacists (ASHP), the Infectious Diseases Society of America (IDSA), the Surgical Infection Society (SIS), and the Society of Healthcare Epidemiology of America (SHEA) guidelines for antimicrobial prophylaxis in surgery, moxifloxacin (systemic) may be administered (in combination with either clindamycin or vancomycin) as an alternative regimen in patients with beta-lactam allergy.
Tuberculosis (second-line therapy)yes
Based on the American Thoracic Society, Centers for Disease Control and Prevention (CDC), and Infectious Diseases Society of America (IDSA) Treatment of Tuberculosis guidelines, moxifloxacin (systemic) given for second-line therapy of tuberculosis is effective and recommended in the management of this condition.
Contraindications
Hypersensitivity to moxifloxacin, other quinolone antibiotics, or any component of the formulation
Dosage and Administration
Dosing: Adult
Anthrax (off-label use) (CDC [Hendricks 2014]):
Inhalational (postexposure prophylaxis): Oral: 400 mg every 24 hours for 60 days
Cutaneous (without systemic involvement): Oral: 400 mg every 24 hours for 7 to 10 days for naturally acquired infection; 60 days for bioterrorism-related cases
Systemic (including meningitis), treatment: IV: 400 mg every 24 hours; use in combination with a protein synthesis inhibitor (eg, clindamycin, linezolid); if meningitis is suspected or cannot be ruled out, use in combination with another bactericidal antimicrobial (eg, beta-lactam) and a protein synthesis inhibitor (eg, clindamycin, linezolid). Duration of therapy is 2 weeks or until clinically stable when meningitis has been excluded; ≥2 to 3 weeks for possible/confirmed meningitis. Patients exposed to aerosolized spores require prophylaxis to complete an antimicrobial course of 60 days from illness onset.
Bite wounds (animal/human) (off-label use): Oral, IV: Note: Recommended as an alternative therapy for human bite wound in patients hypersensitive to beta-lactams: 400 mg once daily (IDSA [Stevens 2014])
Chronic bronchitis, acute bacterial exacerbation: Oral, IV: 400 mg every 24 hours for 5 days
Community-acquired pneumonia (CAP) (including MDRSP): Oral, IV: 400 mg every 24 hours (manufacturer’s labeling) for 5 days (IDSA [Mandell 2007])
Diabetic foot infection (off-label use): Oral, IV: 400 mg once daily (Vick-Fragoso 2009)
Intra-abdominal infections, complicated: Oral, IV: 400 mg every 24 hours for 5 to 14 days (initiate with IV); Note: 2010 IDSA guidelines recommend a treatment duration of 4 to 7 days (provided source controlled) for community-acquired, mild to moderate IAI
Meningitis, bacterial (alternative agent) (off-label use): IV: 400 mg every 24 hours (IDSA [Tunkel 2004]; IDSA [Tunkel 2017]); some experts give in combination with vancomycin or a third generation cephalosporin (IDSA [Tunkel 2017]).
Mycoplasma genitalium (off-label use): Oral: 400 mg every 24 hours for 7, 10, or 14 days (Bissessor 2015; CDC [Workowski 2015])
Nocardiosis (off-label use): Oral, IV: 400 mg once daily; may be used in combination with other antimicrobials (Fihman 2006; Kandasamy 2008; Tripodi 2011). Additional data may be necessary to further define the role of moxifloxacin in this condition.
Pelvic inflammatory disease (in patients allergic to cephalosporins) (off-label use): Oral: 400 mg every 24 hours for 14 days. Note: The CDC recommends use as an alternative therapy only if standard parenteral cephalosporin therapy is not feasible and community prevalence of quinolone-resistant gonococcal organisms is low. Culture sensitivity must be confirmed (CDC [Workowski 2015])
Plague: Oral, IV: 400 mg every 24 hours for 10 to 14 days
Rhinosinusitis, acute bacterial (alternative agent): Oral: 400 mg every 24 hours for 5 to 7 days (initial therapy) or 7 to 10 days (for patients who have not responded to initial therapy) (IDSA [Chow 2012]; Patel 2018). Note: In uncomplicated acute bacterial rhinosinusitis, initial observation and symptom management without antibiotic therapy is appropriate in most patients (AAO-HNS [Rosenfeld 2015]; ACP/CDC [Harris 2016]). Fluoroquinolone use in acute sinusitis should be reserved for those who have no alternative treatment options due to serious risks associated with use compared to benefits (FDA Drug Safety Communication 2016).
Manufacturer’s labeling: Dosing in the prescribing information may not reflect current clinical practice. IV: 400 mg every 24 hours
Skin and skin structure infections: Oral, IV:
Complicated: 400 mg every 24 hours for 7 to 21 days
Uncomplicated: 400 mg every 24 hours for 7 days
Surgical (perioperative) prophylaxis (off-label use): IV: 400 mg within 120 minutes prior to surgical incision (Bratzler 2013).
Tuberculosis, drug-resistant tuberculosis, or intolerance to first-line agents (off-label use): Oral: 400 mg every 24 hours (CDC 2003)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: In pediatric patients, fluoroquinolones are not routinely first-line therapy, but after assessment of risks and benefits, can be considered a reasonable alternative for situations where no safe and effective substitute is available (eg, multidrug resistance) or in situations where the only alternative is parenteral therapy and moxifloxacin offers an oral therapy option (AAP [Jackson 2016]).
Anthrax, systemic (including meningitis), treatment (AAP [Bradley 2014]): Limited data available: Note: Administer as part of triple therapy, duration 2 to 3 weeks or longer until clinical criteria for stability are met; will require prophylaxis to complete an antimicrobial course of up to 60 days from onset of illness.
Infants ≥3 months and Children <2 years: IV: 6 mg/kg/dose every 12 hours; maximum dose: 200 mg/dose
Children 2 to 5 years: IV: 5 mg/kg/dose every 12 hours; maximum dose: 200 mg/dose
Children 6 to 11 years: IV: 4 mg/kg/dose every 12 hours; maximum dose: 200 mg/dose
Children and Adolescents 12 to 17 years:
Body weight <45 kg: IV: 4 mg/kg/dose every 12 hours; maximum dose: 200 mg/dose
Body weight ≥45 kg: IV: 400 mg every 24 hours
Pneumonia, community-acquired (M. pneumoniae, C. pneumoniae, C. trachomatis), mild infection/step-down therapy: Limited data available: Adolescents with skeletal maturity: Oral: 400 mg once daily (IDSA/PIDS [Bradley 2011])
Surgical (perioperative) prophylaxis: Limited data available: Children and Adolescents: IV: 10 mg/kg within 120 minutes prior to surgical incision; maximum dose: 400 mg/dose. Note: While fluoroquinolones have been associated with an increased risk of tendinitis/tendon rupture in all ages, use of these agents for single-dose prophylaxis is generally safe; not the preferred agent in pediatric patients (ASHP/IDSA/SIS/SHEA [Bratzler 2013]).
Tuberculosis, treatment; multidrug resistant: Limited data available, optimal dose not defined: Note: Use in combination with at least 2 to 3 additional anti-TB agents; regimen and duration vary depending upon susceptibility profile/patterns; consult current TB guidelines for detailed information (ATS/CDC/IDSA [Nahid 2016]; WHO 2014). Recent pharmacokinetic studies suggest that higher doses may be necessary in infants and children to achieve serum concentrations similar to adult standard dosing (Srivastava 2016; Thee 2015).
Infants, Children, and Adolescents <15 years: IV, Oral: 10 mg/kg/dose every 24 hours; maximum dose: 400 mg/dose (ATS/CDC/IDSA [Nahid 2016])
Adolescents ≥15 years: IV, Oral: 400 mg every 24 hours (ATS/CDC/IDSA [Nahid 2016])
Extemporaneously Prepared
A 20 mg/mL oral suspension may be made using tablets. Crush three 400 mg tablets and reduce to a fine powder. Carefully sieve powder from enteric-coating remnants to improve pharmaceutical elegance. Add a small amount of a 1:1 mixture of Ora-Plus® and Ora-Sweet® or Ora-Sweet® SF and mix to a uniform paste; mix while adding the vehicle in geometric proportions to almost 60 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 60 mL. Label "shake well". Stable 90 days at room temperature.
Hutchinson DJ, Johnson CE, and Klein KC, "Stability of Extemporaneously Prepared Moxifloxacin Oral Suspensions," Am J Health Syst Pharm, 2009, 66(7):665-7.19299374
Administration
Oral: Administer without regard to meals. Administer at least 4 hours before or 8 hours after products containing magnesium, aluminum, iron, or zinc, including antacids, sucralfate, multivitamins, and didanosine (buffered tablets for oral suspension or the pediatric powder for oral solution).
IV: Infuse over 60 minutes; do not infuse by rapid or bolus intravenous infusion.
Dietary Considerations
Avelox IV infusion (premixed in sodium chloride 0.8%) contains sodium 34.2 mEq (~787 mg)/250 mL.
Storage
Store at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Avoid high humidity. Do not refrigerate infusion solution; discard unused portion.
Moxifloxacin (Systemic) Images
Drug Interactions
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Amphetamines: May enhance the cardiotoxic effect of Quinolones. Monitor therapy
Antacids: May decrease the absorption of Quinolones. Of concern only with oral administration of quinolones. Management: Avoid concurrent administration of quinolones and antacids to minimize the impact of this interaction. Recommendations for optimal dose separation vary by specific quinolone. Exceptions: Sodium Bicarbonate. Consider therapy modification
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Blood Glucose Lowering Agents: Quinolones may enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Quinolones may diminish the therapeutic effect of Blood Glucose Lowering Agents. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Corticosteroids (Systemic): May enhance the adverse/toxic effect of Quinolones. Specifically, the risk of tendonitis and tendon rupture may be increased. Monitor therapy
Delamanid: QT-prolonging Quinolone Antibiotics (Moderate Risk) may enhance the QTc-prolonging effect of Delamanid. Delamanid may enhance the QTc-prolonging effect of QT-prolonging Quinolone Antibiotics (Moderate Risk). Management: Avoid concomitant use of delamanid and quinolone antibiotics if possible. If coadministration is considered to be unavoidable, frequent monitoring of electrocardiograms throughout the full delamanid treatment period should occur. Consider therapy modification
Didanosine: Quinolones may decrease the serum concentration of Didanosine. Didanosine may decrease the serum concentration of Quinolones. Management: Administer oral quinolones at least 2 hours before or 6 hours after didanosine. Monitor for decreased therapeutic effects of quinolones, particularly if doses cannot be separated as recommended. This does not apply to unbuffered enteric coated didanosine. Consider therapy modification
Domperidone: QT-prolonging Agents (Moderate Risk) may enhance the QTc-prolonging effect of Domperidone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Haloperidol: May enhance the QTc-prolonging effect of QT-prolonging Quinolone Antibiotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Heroin: Quinolones may enhance the adverse/toxic effect of Heroin. Monitor therapy
Iron Preparations: May decrease the serum concentration of Quinolones. Management: Give oral quinolones at least several hours before (4 h for moxi- and sparfloxacin, 2 h for others) or after (8 h for moxi-, 6 h for cipro/dela-, 4 h for lome-, 3 h for gemi-, and 2 h for levo-, nor-, oflox-, pefloxacin, or nalidixic acid) oral iron. Exceptions: Ferric Carboxymaltose; Ferric Derisomaltose; Ferric Gluconate; Ferric Hydroxide Polymaltose Complex; Ferric Pyrophosphate Citrate; Ferumoxytol; Iron Dextran Complex; Iron Sucrose. Consider therapy modification
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Lanthanum: May decrease the serum concentration of Quinolones. Management: Administer oral quinolone antibiotics at least one hour before or four hours after lanthanum. Consider therapy modification
Magnesium Salts: May decrease the serum concentration of Quinolones. Management: Administer oral quinolones several hours before (4 h for moxi/pe/spar-, 2 h for others) or after (8 h for moxi-, 6 h for cipro/dela-, 4 h for lome/pe-, 3 h for gemi-, and 2 h for levo-, nor-, or ofloxacin or nalidixic acid) oral magnesium salts. Consider therapy modification
Mequitazine: Moxifloxacin (Systemic) may enhance the arrhythmogenic effect of Mequitazine. Avoid combination
Methylphenidate: May enhance the cardiotoxic effect of Quinolones. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May decrease the serum concentration of Quinolones. Specifically, polyvalent cations in multivitamin products may decrease the absorption of orally administered quinolone antibiotics. Management: Interactions can be minimized by administering the oral quinolone at least 2 hours before, or 6 hours after, the dose of a multivitamin that contains polyvalent cations (i.e., calcium, iron, magnesium, selenium, zinc). Consider therapy modification
Multivitamins/Minerals (with AE, No Iron): May decrease the serum concentration of Quinolones. Specifically, minerals in the multivitamin/mineral product may impair absorption of quinolone antibiotics. Management: Interactions can be minimized by administering the oral quinolone at least 2 hours before, or 6 hours after, the dose of a multivitamin that contains polyvalent cations (i.e., calcium, iron, magnesium, selenium, zinc). Consider therapy modification
Mycophenolate: Quinolones may decrease the serum concentration of Mycophenolate. Specifically, quinolones may decrease concentrations of the active metabolite of mycophenolate. Monitor therapy
Nadifloxacin: May enhance the adverse/toxic effect of Quinolones. Avoid combination
Nonsteroidal Anti-Inflammatory Agents: May enhance the neuroexcitatory and/or seizure-potentiating effect of Quinolones. Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Quinolones. Monitor therapy
Ondansetron: May enhance the QTc-prolonging effect of QT-prolonging Quinolone Antibiotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Pentamidine (Systemic): May enhance the QTc-prolonging effect of QT-prolonging Quinolone Antibiotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Pimozide: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
QT-prolonging Agents (Highest Risk): May enhance the QTc-prolonging effect of Moxifloxacin (Systemic). Exceptions: Delamanid. Avoid combination
QT-prolonging Antidepressants (Moderate Risk): QT-prolonging Quinolone Antibiotics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Antidepressants (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Antipsychotics (Moderate Risk): QT-prolonging Quinolone Antibiotics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Pimozide. Monitor therapy
QT-prolonging Class IC Antiarrhythmics (Moderate Risk): QT-prolonging Quinolone Antibiotics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Class IC Antiarrhythmics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Kinase Inhibitors (Moderate Risk): QT-prolonging Quinolone Antibiotics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Miscellaneous Agents (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Quinolone Antibiotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Domperidone. Monitor therapy
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): QT-prolonging Quinolone Antibiotics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Quinolone Antibiotics (Moderate Risk): May enhance the QTc-prolonging effect of other QT-prolonging Quinolone Antibiotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk): QT-prolonging Quinolone Antibiotics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Quinapril: May decrease the serum concentration of Quinolones. Management: Separate doses of quinapril and oral quinolones by at least 2 hours in order to reduce the risk of interaction. Monitor for reduced efficacy of the quinolone if these products are used concomitantly. Consider therapy modification
Sevelamer: May decrease the absorption of Quinolones. Management: Administer oral quinolones at least 2 hours before or 6 hours after sevelamer. Consider therapy modification
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Strontium Ranelate: May decrease the serum concentration of Quinolones. Management: In order to minimize any potential impact of strontium ranelate on quinolone antibiotic concentrations, it is recommended that strontium ranelate treatment be interrupted during quinolone therapy. Avoid combination
Sucralfate: May decrease the serum concentration of Quinolones. Management: Avoid concurrent administration of quinolones and sucralfate to minimize the impact of this interaction. Recommendations for optimal dose separation vary by specific quinolone. Consider therapy modification
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Varenicline: Quinolones may increase the serum concentration of Varenicline. Management: Monitor for increased varenicline adverse effects with concurrent use of levofloxacin or other quinolone antibiotics, particularly in patients with severe renal impairment. International product labeling recommendations vary. Consult appropriate labeling. Monitor therapy
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Quinolones may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Zinc Salts: May decrease the serum concentration of Quinolones. Management: Give oral quinolones at least several hours before (4 h for moxi- and sparfloxacin, 2 h for others) or after (8 h for moxi-, 6 h for cipro/dela-, 4 h for lome-, 3 h for gemi-, and 2 h for levo-, nor-, pe- or ofloxacin or nalidixic acid) oral zinc salts. Exceptions: Zinc Chloride. Consider therapy modification
Test Interactions
Some quinolones may produce a false-positive urine screening result for opioids using commercially-available immunoassay kits. This has been demonstrated most consistently for levofloxacin and ofloxacin, but other quinolones have shown cross-reactivity in certain assay kits. Confirmation of positive opioid screens by more specific methods should be considered.
Adverse Reactions
1% to 10%:
Central nervous system: Headache (4%), dizziness (3%), insomnia (2%)
Endocrine & metabolic: Decreased serum glucose (≥2%), hyperchloremia (≥2%), increased serum albumin (≥2%), hypokalemia (1%)
Gastrointestinal: Nausea (7%), diarrhea (6%), decreased amylase (≥2%), constipation (2%), vomiting (2%), abdominal pain (1% to 2%), dyspepsia (1%)
Hematologic & oncologic: Decreased basophils (≥2%), decreased red blood cells (≥2%), eosinopenia (≥2%), increased MCH (≥2%), increased neutrophils (≥2%), leukocytosis (≥2%), prolonged prothrombin time (≥2%), anemia (1%)
Hepatic: Decreased serum bilirubin (≥2%), increased serum bilirubin (≥2%), increased serum alanine aminotransferase (1%)
Immunologic: Increased serum globulins (≥2%)
Renal: Increased ionized serum calcium (≥2%)
Respiratory: Hypoxia (≥2%)
Miscellaneous: Fever (1%)
<1%, postmarketing, and/or case reports: Abdominal distention, abdominal distress, abnormal gait, abnormal hepatic function tests, agitation, agranulocytosis, allergic dermatitis, anaphylactic shock, anaphylaxis, angina pectoris, angioedema, anorexia, anxiety, aplastic anemia, arthralgia, asthenia, asthma, ataxia, atrial fibrillation, auditory impairment, back pain, blurred vision, bradycardia, bronchospasm, candidiasis, cardiac failure, chest discomfort, chest pain, chills, cholestatic hepatitis, Clostridioides difficile associated diarrhea, Clostridioides difficile colitis, confusion, deafness, decreased appetite, dehydration, delirium, depression, disorientation, disturbance in attention, drowsiness, dysesthesia, dysgeusia, dyspnea, dysuria, edema, eosinophilia, erythema of skin, exacerbation of myasthenia gravis, facial edema, facial pain, fatigue, flatulence, fungal infection, gastritis, gastroenteritis, gastroesophageal reflux disease, hallucination, hemolytic anemia, hepatic failure, hepatic necrosis, hepatitis, hepatotoxicity (idiosyncratic) (Chalasani 2014), hyperglycemia, hyperhidrosis, hyperlipidemia, hypersensitivity pneumonitis, hypersensitivity reaction, hypertension, hypoesthesia, hypoglycemia, hypotension, idiopathic intracranial hypertension, increased amylase, increased blood urea nitrogen, increased gamma-glutamyl transferase, increased intracranial pressure, increased lactate dehydrogenase, increased serum alkaline phosphatase, increased serum aspartate aminotransferase, increased serum creatinine, increased serum lipase, increased serum triglycerides, increased uric acid, interstitial nephritis, jaundice, laryngeal edema, lethargy, leukopenia, limb pain, loss of consciousness, malaise, memory impairment, muscle spasm, musculoskeletal pain, myalgia, myasthenia, nervousness, neutropenia, nightmares, night sweats, pain, palpitations, pancytopenia, paranoid ideation, paresthesia, peripheral neuropathy (may be irreversible), pharyngeal edema, phlebitis, phototoxicity, polyneuropathy, prolonged partial thromboplastin time, prolonged QT interval on ECG, pruritus, renal failure syndrome, renal insufficiency, restlessness, rupture of tendon, seizure, serum sickness, skin photosensitivity, skin rash, Stevens-Johnson syndrome, suicidal ideation, suicidal tendencies, syncope, tachycardia, tendonitis, thrombocythemia, thrombocytopenia, thrombotic thrombocytopenic purpura, tingling sensation, tinnitus, torsades de pointes, toxic epidermal necrolysis, toxic psychosis, tremor, urticaria, vaginal infection, vasculitis, ventricular tachyarrhythmia, vertigo, vision loss, vulvovaginal pruritus, wheezing, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- Altered cardiac conduction: Fluoroquinolones may prolong QTc interval; avoid use in patients with known QTc prolongation, ventricular arrhythmias including torsades de pointes, proarrhythmic conditions (eg, clinically significant bradycardia, acute myocardial ischemia), uncorrected hypokalemia, hypomagnesemia, or concurrent administration of other medications known to prolong the QT interval (including Class Ia and Class III antiarrhythmics, cisapride, erythromycin, antipsychotics, and tricyclic antidepressants).
- Aortic aneurysm and dissection: Fluoroquinolones have been associated with aortic aneurysm ruptures or dissection within 2 months following use, particularly in elderly patients. Fluoroquinolones should not be used in patients with a known history of aortic aneurysm or those at increased risk, including patients with peripheral atherosclerotic vascular diseases, hypertension, genetic disorders involving blood vessel changes (eg, Marfan syndrome, Ehlers-Danlos syndrome), and elderly patients, unless no other treatment options are available. Longer treatment duration (eg, >14 days) may increase risk (Lee 2018).
- Glucose regulation: Fluoroquinolones have been associated with disturbances in glucose regulation, including hyperglycemia and hypoglycemia. These events have occurred most often in elderly patients or patients receiving concomitant oral hypoglycemic agents or insulin. Severe cases of hypoglycemia, including coma and death, have been reported. Diabetic patients should be monitored closely for signs/symptoms of disordered glucose regulation. Discontinue if a hypoglycemic reaction occurs and immediately initiate appropriate therapy.
- Hepatotoxicity: Fulminant hepatitis potentially leading to liver failure (including fatalities) has been reported with use; patients should be advised to discontinue treatment and promptly report signs/ symptoms of hepatitis (eg, abdominal pain, jaundice, dark urine, pale stools).
- Hypersensitivity reactions: Severe hypersensitivity reactions, including anaphylaxis, have occurred with quinolone therapy. The spectrum of these reactions can vary widely; reactions may present as typical allergic symptoms (eg, itching, urticaria, rash, edema) after a single dose, or may manifest as severe idiosyncratic dermatologic (eg, Stevens-Johnson, toxic epidermal necrolysis), vascular (eg, vasculitis), pulmonary (eg, pneumonitis), renal (eg, nephritis), hepatic (eg, hepatic failure or necrosis), and/or hematologic (eg, anemia, cytopenias) events, usually after multiple doses. Prompt discontinuation of drug should occur if skin rash or other symptoms arise.
- Photosensitivity: Avoid excessive sunlight and take precautions to limit exposure (eg, loose fitting clothing, sunscreen); may rarely cause moderate to severe phototoxicity reactions. Discontinue use if phototoxicity occurs.
- Serious adverse reactions: [US Boxed Warning]: Fluoroquinolones are associated with disabling and potentially irreversible serious adverse reactions that may occur together, including tendinitis and tendon rupture, peripheral neuropathy, and CNS effects. Discontinue moxifloxacin immediately and avoid use of fluoroquinolones in patients who experience any of these serious adverse reactions. Patients of any age or without pre-existing risk factors have experienced these reactions; may occur within hours to weeks after initiation.
- CNS effects: Fluoroquinolones have been associated with an increased risk of CNS effects including seizures, increased intracranial pressure (including pseudotumor cerebri), lightheadedness, dizziness, and tremors. May occur following the first dose; discontinue immediately and avoid further use of fluoroquinolones in patients who experience these reactions. Use with caution in patients with known or suspected CNS disorder, or risk factors that may predispose to seizures or lower the seizure threshold.
- Peripheral neuropathy: Fluoroquinolones have been associated with an increased risk of peripheral neuropathy; may occur soon after initiation of therapy and may be irreversible; discontinue if symptoms of sensory or sensorimotor neuropathy occur. Avoid use in patients who have previously experienced peripheral neuropathy.
- Psychiatric reactions: Fluoroquinolones have been associated with an increased risk of psychiatric reactions, including toxic psychosis, hallucinations, or paranoia; may also cause nervousness, agitation, delirium, attention disturbances, insomnia, anxiety, nightmares, memory impairment, confusion, depression, and suicidal thoughts or actions. Use with caution in patients with a history of or risk factor for depression. Reactions may occur following the first dose; discontinue if reaction occurs and institute appropriate therapy.
- Tendinitis/tendon rupture: Fluoroquinolones have been associated with an increased risk of tendonitis and tendon rupture in all ages; risk may be increased with concurrent corticosteroids, solid organ transplant recipients, and in patients >60 years of age, but has also occurred in patients without these risk factors. Rupture of the Achilles tendon has been reported most frequently; but other tendon sites (eg, rotator cuff, biceps, hand) have also been reported. Inflammation and rupture may occur bilaterally. Cases have been reported within hours or days of initiation, and up to several months after discontinuation of therapy. Strenuous physical activity, renal failure, and previous tendon disorders may be independent risk factor for tendon rupture. Discontinue at first sign of tendon pain, swelling, inflammation or rupture. Avoid use in patients with a history of tendon disorders or who have experienced tendinitis or tendon rupture.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with significant bradycardia or acute myocardial ischemia.
- Diabetes: Use with caution in patients with diabetes mellitus; glucose regulation may be altered.
- Hepatic impairment: Use with caution in patients with mild, moderate, or severe hepatic impairment or liver cirrhosis; may increase the risk of QT prolongation.
- Myasthenia gravis: [US Boxed Warning]: May exacerbate muscle weakness related to myasthenia gravis; avoid use in patients with known history of myasthenia gravis. Cases of severe exacerbations, including the need for ventilatory support, and deaths have been reported.
- Renal impairment: Use with caution in patients with renal failure; may increase risk of tendon rupture.
- Rheumatoid arthritis: Use with caution in patients with rheumatoid arthritis; may increase risk of tendon rupture.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Adverse effects (eg, tendon rupture, QT changes) may be increased in elderly patients.
- G6PD deficiency: Hemolytic reactions may (rarely) occur with quinolone use in patients with latent or actual G6PD deficiency.
- Pediatric: Efficacy of systemically administered moxifloxacin (oral, intravenous) have not been established in pediatric patients.
Other warnings/precautions:
- Appropriate use: [US Boxed Warning]: Reserve use of moxifloxacin for treatment of acute bacterial sinusitis or acute bacterial exacerbation of chronic bronchitis for patients who have no alternative treatment options because of the risk of disabling and potentially serious adverse reactions (eg, tendinitis and tendon rupture, peripheral neuropathy, CNS effects).
Monitoring Parameters
WBC, signs of infection, signs/symptoms of disordered glucose regulation, ECG in patients with liver cirrhosis
Pregnancy
Pregnancy Considerations
Moxifloxacin crosses the placenta (Ozyüncü and Beksac 2010; Ozyüncü and Nemutlu 2010).
Due to pregnancy-induced physiologic changes, some pharmacokinetic properties of moxifloxacin may be altered (Nemutlu 2010; van Kampenhout 2017).
Patient Education
What is this drug used for?
- It is used to treat bacterial infections.
Frequently reported side effects of this drug
- Nausea
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
• Clostridioides (formerly Clostridium) difficile (C. diff)-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools
- Tendon inflammation or rupture like pain, bruising, or swelling in the back of the ankle, shoulder, hand, or other joints
- Depression like thoughts of suicide, anxiety, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating
- Chest pain
- Fast heartbeat
- Trouble focusing
- Trouble with memory
- Abnormal heartbeat
- Passing out
- Dizziness
- Chills
- Severe loss of strength and energy
- Muscle pain
- Muscle weakness
- Nightmares
- Restlessness
- Sensing things that seem real but are not
- Seizures
- Severe headache
- Sore throat
- Shortness of breath
- Bruising
- Bleeding
- Tremors
- Trouble sleeping
- Abnormal gait
- Vaginal pain, itching, and discharge
- Thrush
- Vision changes
- Severe or persistent abdominal pain
- Severe or persistent chest pain
- Severe or persistent back pain
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.