Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Amerge: 1 mg, 2.5 mg
Generic: 1 mg, 2.5 mg
Pharmacology
Mechanism of Action
Selective agonist for serotonin (5-HT1B and 5-HT1D receptors) in cranial arteries; causes vasoconstriction and reduces sterile inflammation associated with antidromic neuronal transmission correlating with relief of migraine
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed
Distribution
Vdss: 170 L
Metabolism
Hepatic via CYP
Excretion
Urine (50% of total dose as unchanged drug; 30% of total dose as metabolites)
Onset of Action
~1 to 2 hours (Bomhof 1999; Tfelt-Hansen 2000)
Time to Peak
2 to 3 hours
Half-Life Elimination
6 hours; Increased in renal impairment (moderate impairment; mean: 11 hours; range: 7 to 20 hours); Increased in hepatic impairment (moderate impairment: 8 to 16 hours)
Protein Binding
Plasma: 28% to 31%
Use in Specific Populations
Special Populations: Renal Function Impairment
Naratriptan clearance is reduced 50% with moderate impairment (CrCl 18 to 39 mL/minute); mean Cmax increased ~40%.
Special Populations: Hepatic Function Impairment
Naratriptan clearance is decreased 30% in patients with moderate impairment (Child-Pugh class A or B).
Special Populations: Elderly
Clearance is decreased ~26% in healthy elderly subjects (65 to 77 years) compared with younger patients.
Special Populations: Gender
Cmax is 50% higher in women.
Use: Labeled Indications
Migraines: Acute treatment of migraine attacks with or without aura in adults.
Use: Off Label
Menstrual migraine preventionbyes
Data from 3 randomized, double-blind, placebo-controlled studies support the use of naratriptan in the short-term prevention of menstrual migraines Mannix 2007, Newman 2001.
Based on the American Academy of Neurology and the American Headache Society guidelines for the pharmacologic treatment of episodic migraine prevention in adults, naratriptan is probably effective for the short-term prevention of menstrual migraine Silberstein 2012.
Contraindications
Ischemic coronary artery disease (CAD) (angina pectoris, history of myocardial infarction [MI], or documented silent ischemia); coronary artery vasospasm, including Prinzmetal's angina; Wolff-Parkinson-White syndrome or arrhythmias associated with other cardiac accessory conduction pathway disorders; history of stroke, transient ischemic attack (TIA), or history of hemiplegic or basilar migraine; peripheral vascular disease; ischemic bowel disease; uncontrolled hypertension; recent use (within 24 hours) of another 5-HT1 agonist, ergotamine-containing medication, or ergot-type medication (eg, dihydroergotamine or methysergide); severe renal impairment (CrCl <15 mL/minute) or severe hepatic impairment; hypersensitivity to naratriptan or any component of the formulation
Canadian labeling: Additional contraindications (not in US labeling): Severe hypertension, cardiac arrhythmias (especially tachycardias); valvular heart disease, congenital heart disease, atherosclerotic disease; management of ophthalmoplegic migraine
Documentation of allergenic cross-reactivity for triptans is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Note: If the first dose is ineffective, diagnosis needs to be re-evaluated. The safety of treating >4 migraines/month has not been established.
Acute migraine: Oral: Initial: 1 to 2.5 mg; if headache recurs or does not fully resolve, a second dose may be administered after 4 hours (maximum: 5 mg in a 24-hour period)
Menstrual migraine prevention (off-label use): Oral: 1 mg twice daily beginning 2 to 3 days prior to expected onset of symptoms; continue for a total of 5 to 6 days (Mannix 2007; Newman 2001).
Dosing: Geriatric
Refer to adult dosing. Dosing should generally start at the lower end of the dosing range due to possible increased incidence of hepatic, renal, and cardiac impairment.
Extemporaneously Prepared
A 0.5 mg/mL oral suspension may be made using tablets. Crush fifty 2.5 mg tablets and reduce to a fine powder. In small amounts, add 125 mL of Ora-Plus® and mix well after each addition. Transfer to a calibrated bottle, rinse mortar with vehicle, then add quantity of Ora-Sweet® or Ora-Sweet® SF sufficient to make 250 mL. Label "shake well" and "refrigerate". Stable 90 days refrigerated.
Nahata MC, Pai VB, and Hipple TF, Pediatric Drug Formulations, 5th ed, Cincinnati, OH: Harvey Whitney Books Co, 2004.
Administration
Oral: Administer orally as soon as symptoms appear; may take with or without food. Do not crush or chew tablet; swallow whole with water.
Storage
Store at 20°C to 25°C (68°F to 77°F).
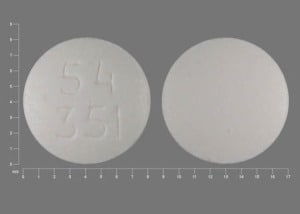
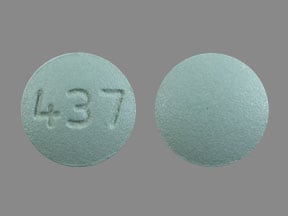
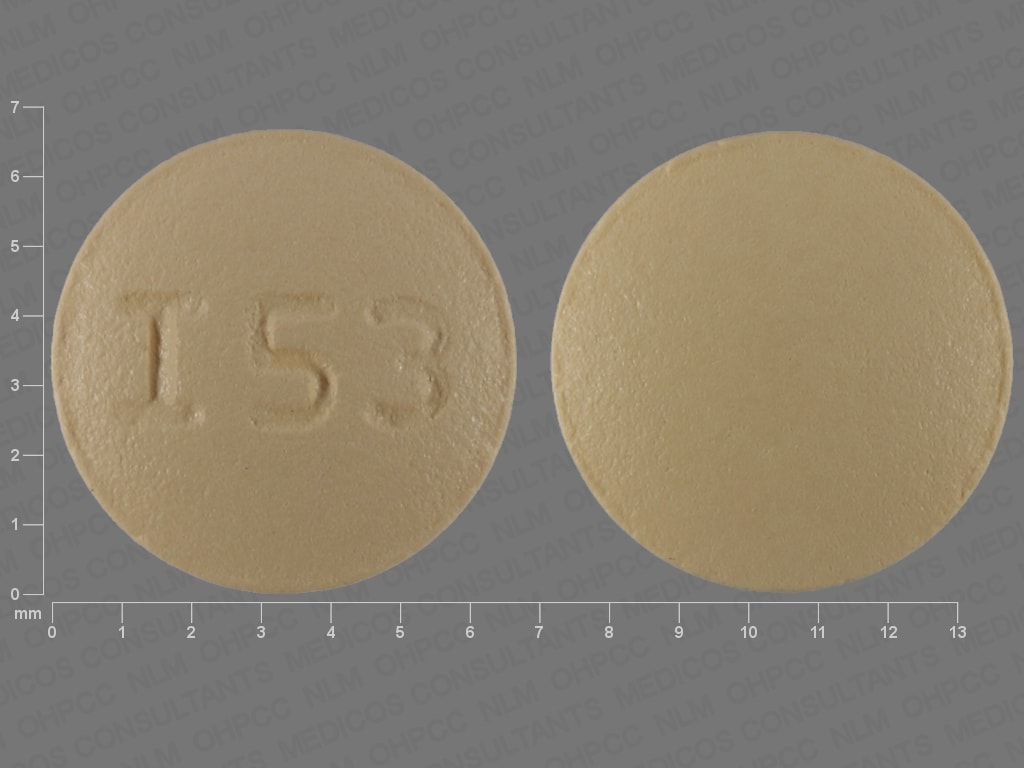
Naratriptan Images
Drug Interactions
Droxidopa: Serotonin 5-HT1D Receptor Agonists (Triptans) may enhance the hypertensive effect of Droxidopa. Monitor therapy
Ergot Derivatives: May enhance the vasoconstricting effect of Serotonin 5-HT1D Receptor Agonists (Triptans). Serotonin 5-HT1D Receptor Agonists (Triptans) may enhance the vasoconstricting effect of Ergot Derivatives. Exceptions: Nicergoline. Avoid combination
Monoamine Oxidase Inhibitors: Serotonin 5-HT1D Receptor Agonists (Triptans) may enhance the serotonergic effect of Monoamine Oxidase Inhibitors. This could result in serotonin syndrome. Monoamine Oxidase Inhibitors may increase the serum concentration of Serotonin 5-HT1D Receptor Agonists (Triptans). Exceptions: Rasagiline; Safinamide; Selegiline. Avoid combination
Serotonergic Agents (High Risk): Serotonin 5-HT1D Receptor Agonists (Triptans) may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Isocarboxazid; Linezolid; Methylene Blue; Moclobemide; Phenelzine; Tranylcypromine. Monitor therapy
SUMAtriptan: Serotonin 5-HT1D Receptor Agonists (Triptans) may enhance the adverse/toxic effect of SUMAtriptan. Avoid combination
Adverse Reactions
1% to 10%:
Central nervous system: Pain (4%), fatigue (2%), dizziness (1% to 2%), drowsiness (1% to 2%), paresthesia (1% to 2%), hot and cold flashes (1%), sensation of pressure (1%; chest/neck/throat/jaw), vertigo (1%)
Gastrointestinal: Nausea (4% to 5%), vomiting (1%), xerostomia (1%)
Neuromuscular & skeletal: Neck pain (2%)
Ophthalmic: Photophobia (1%)
Respiratory: Constriction of the pharynx (2%), ENT infection (1%)
<1%, postmarketing, and/or case reports (limited to important or life-threatening): Abnormal bilirubin levels, abnormal hepatic function tests, anaphylactoid reaction, anaphylaxis, anemia, angina pectoris, angioedema, bradycardia, cerebral infarction, colonic ischemia, coronary artery vasospasm, depression, dyspnea, ECG changes (atrial fibrillation, atrial flutter, premature ventricular contractions, PR prolongation, or QTc prolongation), glycosuria, hallucination, heart murmur, hypercholesterolemia, hyperglycemia, hyperlipidemia, hypersensitivity reaction (some cases severe, including circulatory collapse), hypertension, hypotension, hypothyroidism, ischemic heart disease, ketonuria, myocardial infarction, palpitations, panic, seizure, serotonin syndrome, skin rash, subarachnoid hemorrhage, subconjunctival hemorrhage, syncope, thrombocytopenia, transient ischemic attacks, ventricular fibrillation, ventricular tachycardia
Warnings/Precautions
Concerns related to adverse effects:
- Anaphylactic reactions: Anaphylaxis and hypersensitivity reactions (including angioedema) have occurred; may be life-threatening or fatal. Use is contraindicated in patients with known hypersensitivity to naratriptan.
- Cardiac events: Coronary artery vasospasm, transient ischemia, myocardial infarction, ventricular tachycardia/fibrillation, cardiac arrest, and death have been reported with 5-HT1 agonist administration; some events have occurred within a few hours of administration. Discontinue if these events occur. Patients who experience sensations of chest pain/pressure/tightness or symptoms suggestive of angina following dosing should be evaluated for coronary artery disease (CAD) or Prinzmetal's angina before receiving additional doses; if dosing is resumed and similar symptoms recur, monitor with ECG. Use is contraindicated in patients with ischemic or vasospastic CAD and Wolff-Parkinson-White syndrome or arrhythmias associated with other cardiac accessory conduction pathway disorders.
- Cerebrovascular events: Cerebral/subarachnoid hemorrhage and stroke (some fatal) have been reported with 5-HT1 agonist administration. Use is contraindicated in patients with a history of stroke or transient ischemic attack.
- CNS depression: May cause CNS depression, such as dizziness, weakness, or drowsiness, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Elevated blood pressure: Significant elevation in blood pressure, including hypertensive crisis with acute impairment of organ systems, has been reported on rare occasions in patients with and without a history of hypertension. Monitor blood pressure; use is contraindicated in patients with uncontrolled hypertension.
- Headaches: Acute migraine agents (eg, triptans, opioids, ergotamine, or a combination of the agents) used for 10 or more days per month may lead to worsening of headaches (medication overuse headache); withdrawal treatment may be necessary in the setting of overuse.
- Vasospasm-related events: Peripheral vascular ischemia and colonic ischemia, gastrointestinal vascular ischemia and infarction, splenic infarction, and Raynaud syndrome have been reported with 5-HT1 agonist administration.
- Visual effects: Partial vision loss and blindness (transient and permanent) have been reported with use of 5-HT1 agonists; a causal relationship between these events and 5-HT1 agonist administration has not been clearly determined.
Disease-related concerns:
- Coronary artery disease: Should not be given to patients who have risk factors for CAD (eg, hypertension, hypercholesterolemia, smoker, obesity, diabetes, strong family history of CAD, menopause, male >40 years of age) without adequate cardiac evaluation. Use is contraindicated if there is evidence of CAD or coronary artery vasospasm. Patients with suspected CAD should have cardiovascular evaluation to rule out CAD before considering use; if cardiovascular evaluation is “satisfactory,” first dose should be given in the health care provider's office (consider ECG monitoring). Periodic evaluation of cardiovascular status should be done in all patients.
- Hepatic impairment: Use is contraindicated in patients with severe hepatic impairment (Child-Pugh grade C).
- Renal impairment: Use is contraindicated in patients with severe renal impairment (CrCl <15 mL/minute).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Serotonin syndrome: Symptoms of agitation, confusion, hallucinations, hyper-reflexia, myoclonus, shivering, and tachycardia may occur with concomitant proserotonergic drugs (ie, SSRIs/SNRIs or triptans) or agents which reduce naratriptan's metabolism. Concurrent use of serotonin precursors (eg, tryptophan) is not recommended. If concomitant administration with SSRIs is warranted, monitor closely, especially at initiation and with dose increases. Discontinue naratriptan if serotonin syndrome is suspected.
Special populations:
- Elderly: Blood pressure increases may be more pronounced in the elderly.
Other warnings/precautions:
- Appropriate use: Only indicated for the acute treatment of migraine; not indicated for migraine prophylaxis, or for the treatment of cluster headache, hemiplegic, or basilar migraine. If a patient does not respond to the first dose, the diagnosis of migraine should be reconsidered; rule out underlying neurologic disease in patients with atypical headache and in patients with no prior history of migraine.
Monitoring Parameters
Headache severity, blood pressure, signs/symptoms suggestive of angina; perform a cardiovascular evaluation in triptan-naïve patients who have multiple cardiovascular risk factors (eg, increased age, diabetes, hypertension, smoking, obesity, strong family history of CAD), monitor ECG with first dose in patients with multiple cardiovascular risk factors who have a negative cardiovascular evaluation and consider periodic cardiovascular evaluation in such patients if they are intermittent long-term users; signs/symptoms of serotonin syndrome and hypersensitivity reactions.
Pregnancy
Pregnancy Considerations
Pregnancy outcome information for naratriptan is available from a pregnancy registry sponsored by GlaxoSmithKline. As of September 2012, data were available for 57 infants/fetuses exposed to naratriptan, and seven exposed to both naratriptan and sumatriptan. Following naratriptan exposure, there was one infant born with a birth defect; this infant was also exposed to sumatriptan during the first trimester of pregnancy. The pregnancy registry was closed to enrollment in January 2012, and additional information may be obtained from the manufacturer. Additional information related to the use of naratriptan in pregnancy is limited (Källén 2011; Nezvalová-Henriksen 2010; Nezvalová-Henriksen 2012). Until additional information is available, other agents are preferred for the initial treatment of migraine in pregnancy (Da Silva 2012; MacGregor 2012; Williams 2012).
Patient Education
What is this drug used for?
- It is used to treat migraine headaches.
Frequently reported side effects of this drug
- Fatigue
- Loss of strength and energy
- Flushing
- Sensation of warmth
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or vision changes
- Heart attack like chest pain; pain in arms, back, neck, jaw, or abdomen; shortness of breath; cold sweats; severe dizziness; passing out; or severe nausea or vomiting
- Serotonin syndrome like dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, or severe diarrhea
- Abnormal heartbeat
- Skin discoloration
- Severe headache
- Severe dizziness
- Passing out
- Vision changes
- Blindness
- Burning or numbness feeling
- Constipation
- Diarrhea
- Severe nausea
- Vomiting
- Severe abdominal pain
- Bloody diarrhea
- Weight loss
- Leg cramps
- Sensation of leg heaviness
- Sensation of cold
- Shortness of breath
- Burning or aching of feet or toes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.