Boxed Warning
Neurologic adverse reactions:
Severe neurologic adverse reactions have been reported with the use of nelarabine. These reactions have included altered mental states, including severe somnolence; CNS effects, including convulsions; and peripheral neuropathy, ranging from numbness and paresthesias to motor weakness and paralysis. There have also been reports of adverse reactions associated with demyelination and ascending peripheral neuropathies similar in appearance to Guillain-Barré syndrome.
Full recovery from these reactions has not always occurred with cessation of therapy with nelarabine. Monitor frequently for signs and symptoms of neurologic toxicity during treatment with nelarabine. Discontinue nelarabine for neurologic reactions of National Cancer Institute (NCI) Common Toxicity Criteria for Adverse Events (CTCAE) grade 2 or greater.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Intravenous [preservative free]:
Arranon: 5 mg/mL (50 mL)
Pharmacology
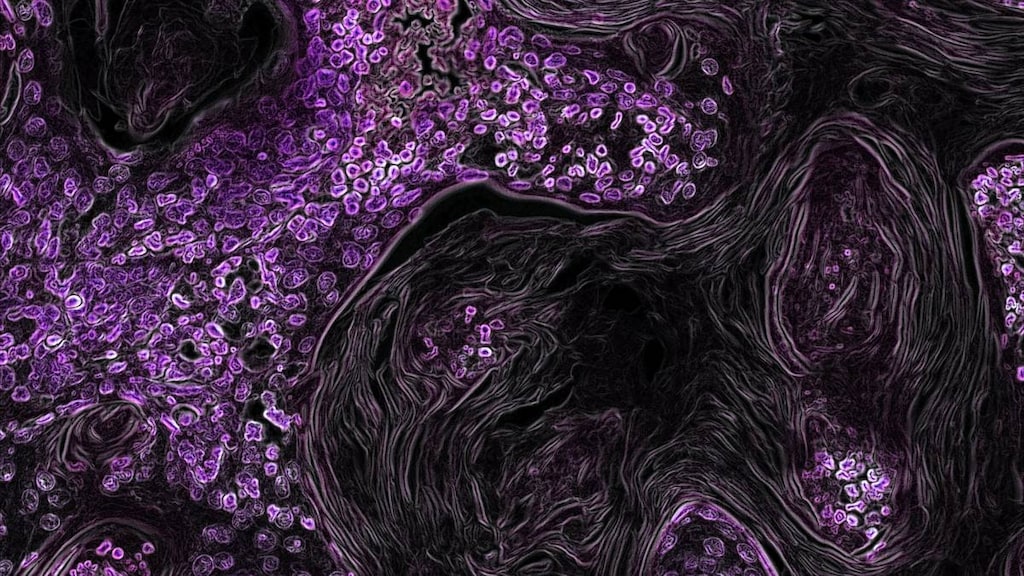
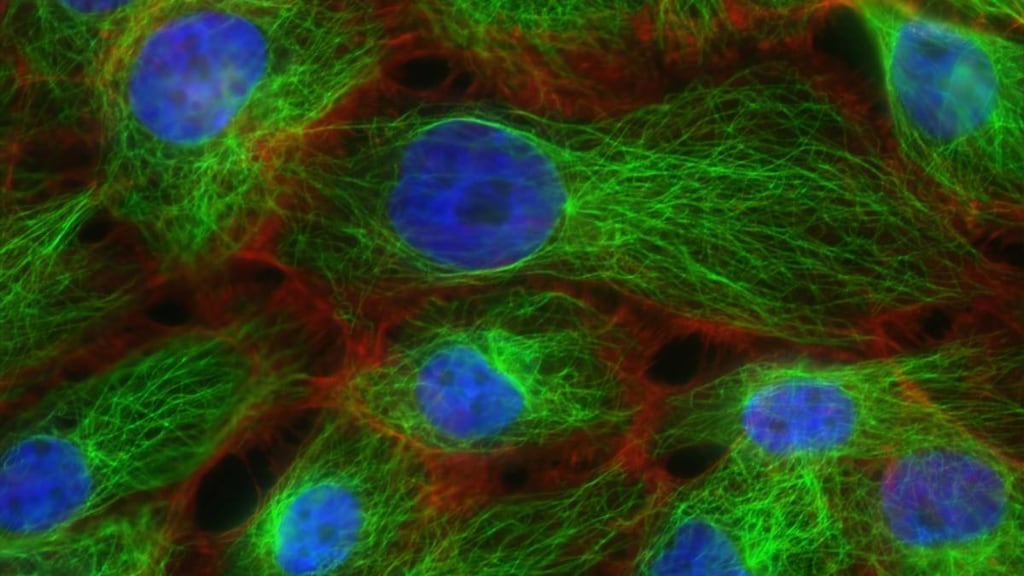
Mechanism of Action
Nelarabine, a prodrug of ara-G, is demethylated by adenosine deaminase to ara-G and then converted to ara-GTP. Ara-GTP is incorporated into the DNA of the leukemic blasts, leading to inhibition of DNA synthesis and inducing apoptosis. Ara-GTP appears to accumulate at higher levels in T-cells, which correlates to clinical response.
Pharmacokinetics/Pharmacodynamics
Distribution
Vss:
Nelarabine: Pediatric patients: 213 ± 358L/m2; Adults: 197 ± 216 L/m2
Ara-G: Pediatric patients: 33 ± 9.3 L/m2; Adults: 50 ± 24 L/m2
Metabolism
Hepatic; demethylated by adenosine deaminase to form ara-G (active); also hydrolyzed to form methylguanine. Both ara-G and methylguanine metabolized to guanine. Guanine is deaminated into xanthine, which is further oxidized to form uric acid, which is then oxidized to form allantoin.
Excretion
Urine (nelarabine 5% to 10%, Ara-G 20% to 30%)
Nelarabine clearance is ~30% higher in pediatric patients (259 ± 409 L/hour/m2) than in adults (197 ± 189 L/hour/m2); Ara-G clearance in pediatric patients (11.3 ± 4.2 L/hour/m2) is similar to adults (10.5 ± 4.5 L/hour/m2)
Time to Peak
Adults: 3 to 25 hours (of day 1)
Half-Life Elimination
Pediatric patients: Nelarabine: 13 minutes, Ara-G: 2 hours; Adults: Nelarabine: 18 minutes, Ara-G: 3.2 hours
Protein Binding
Nelarabine and ara-G: <25%
Use in Specific Populations
Special Populations: Renal Function Impairment
Clearance of Ara-G is reduced 15% in patients with mild renal impairment (CrCl 50 to 80 mL/minute) and 40% in patients with moderate renal impairment (CrCl <50 mL/minute), compared to patients with normal renal function.
Special Populations: Elderly
Reduced renal function in elderly patients may reduce Ara-G clearance.
Special Populations: Race
Mean clearance and Vd values tended to be higher in white patients than in black patients (by approximately 10%). The opposite is true for ara-G; mean apparent Cl and Vd values tended to be lower in white patients than in black patients (by approximately 15% to 20%).
Use: Labeled Indications
T-cell acute lymphoblastic leukemia/lymphoma: Treatment of relapsed or refractory T-cell acute lymphoblastic leukemia/lymphoma in patients ≥1 year of age following at least 2 chemotherapy regimens
Contraindications
There are no contraindications listed in the manufacturer's US labeling.
Canadian labeling: Hypersensitivity to nelarabine or any component of the formulation.
Dosage and Administration
Dosing: Adult
Note: Adequate hydration and prophylactic antihyperuricemic therapy are recommended to prevent tumor lysis syndrome.
T-cell acute lymphoblastic leukemia/lymphoma: IV: 1,500 mg/m2/dose on days 1, 3, and 5; repeat every 21 days until a transplant candidate, disease progression, unacceptable toxicity, or until no longer benefiting from therapy.
Dosing: Geriatric
Refer to adult dosing. Age ≥65 years may be associated with increased neurotoxicity; monitor closely.
Dosing: Pediatric
Note: Dosing and frequency may vary by protocol and/or treatment phase; refer to specific protocol. Adequate IV hydration and prophylactic antihyperuricemic therapy are recommended to prevent tumor lysis syndrome.
T-cell acute lymphoblastic leukemia (T-ALL); newly diagnosed, high risk: Limited data available: Note: Nelarabine was not administered within 2 weeks of other chemotherapies known to cause central or peripheral toxicities.
Children and Adolescents: IV:
Consolidation: 650 mg/m2/dose on days 1 through 5 and 43 through 47 of a 77-day cycle (in combination with vincristine, pegaspargase, cyclophosphamide, cytarabine, mercaptopurine, and intrathecal methotrexate) (Winter 2015; Winter 2018).
Delayed intensification: 650 mg/m2/dose on days 29 through 33 of a 63-day cycle (in combination with vincristine, dexamethasone, pegaspargase, cyclophosphamide, cytarabine, thioguanine, doxorubicin, and intrathecal methotrexate) (Winter 2015; Winter 2018).
Maintenance: 650 mg/m2/dose on days 29 through 33 of an 84-day cycle; during first 3 cycles only (in combination with vincristine, mercaptopurine, prednisone, oral methotrexate, and intrathecal methotrexate) (Winter 2015; Winter 2018).
T-cell acute lymphoblastic leukemia (T-ALL), T-cell lymphoblastic lymphoma; relapsed/refractory: Children and Adolescents: IV:
Monotherapy: 650 mg/m2/dose on days 1 through 5; repeat cycle every 21 days until transplant, disease progression, or unacceptable toxicity (Zwaan 2017).
Combination therapy: Limited data available: 650 mg/m2/dose for 5 consecutive days (in combination with etoposide and cyclophosphamide) for up to 2 cycles. In the clinical trial, nelarabine was administered either before (days 1 through 5) or 1 to 2 days after other chemotherapy (days 7 or 8 through 11 or 12) (in combination with etoposide and cyclophosphamide) for up to 2 cycles (Commander 2010).
Dosage adjustment for toxicity: Children and Adolescents:
Neurologic toxicity ≥ grade 2: Discontinue treatment.
Hematologic or other (non-neurologic) toxicity: Consider treatment delay.
Dosing: Adjustment for Toxicity
Neurologic toxicity ≥ grade 2: Discontinue treatment.
Hematologic or other (non-neurologic) toxicity: Consider treatment delay.
Reconstitution
Administer undiluted; reconstitution is not required; the appropriate dose should be added to an empty polyvinylchloride bag or glass container.
Administration
Adequate IV hydration and prophylactic antihyperuricemic therapy are recommended to prevent tumor lysis syndrome.
Infuse over 2 hours on days 1, 3, and 5.
Storage
Store intact vials at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Stable in a polyvinylchloride infusion bag or a glass container for up to 8 hours at 30°C (86°F).
Drug Interactions
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
Cladribine: Agents that Undergo Intracellular Phosphorylation may diminish the therapeutic effect of Cladribine. Avoid combination
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Lenograstim: Antineoplastic Agents may diminish the therapeutic effect of Lenograstim. Management: Avoid the use of lenograstim 24 hours before until 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Lipegfilgrastim: Antineoplastic Agents may diminish the therapeutic effect of Lipegfilgrastim. Management: Avoid concomitant use of lipegfilgrastim and myelosuppressive cytotoxic chemotherapy. Lipegfilgrastim should be administered at least 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Palifermin: May enhance the adverse/toxic effect of Antineoplastic Agents. Specifically, the duration and severity of oral mucositis may be increased. Management: Do not administer palifermin within 24 hours before, during infusion of, or within 24 hours after administration of myelotoxic chemotherapy. Consider therapy modification
Pentostatin: May diminish the antineoplastic effect of Nelarabine. Conversion of nelarabine, a pro-drug, to its active form may be inhibited by pentostatin. Avoid combination
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Adverse Reactions
>10%:
Cardiovascular: Peripheral edema (adults: 15%), edema (adults: 11%)
Central nervous system: Fatigue (adults: 50%), drowsiness (adults: 23%; children and adolescents: 7%), dizziness (adults: 21%), hypoesthesia (adults: 17%; children and adolescents: 6%), headache (15% to 17%), paresthesia (adults: 15%; children and adolescents: 4%), peripheral sensory neuropathy (6% to 13%; children and adolescents, grade 3: 6%), pain (adults: 11%)
Endocrine & metabolic: Decreased serum potassium (children and adolescents: 11%)
Gastrointestinal: Nausea (adults: 41%), diarrhea (adults: 22%), vomiting (adults: 22%; children and adolescents: 10%), constipation (adults: 21%)
Hematologic & oncologic: Anemia (95% to 99%; children and adolescents, grade 3: 45%; adults, grade 3: 20%; grades ≥4: 10% to 14%), neutropenia (children and adolescents: 94%; adults: 81%; grade 3: 14% to 17%, children and adolescents, grades ≥4: 62%, adults, grades ≥4: 49%), thrombocytopenia (86% to 88%; adults, grade 3: 37%; children and adolescents, grade 3: 27%; children and adolescents, grades ≥4: 32%; adults, grades ≥4: 22%), leukopenia (children and adolescents: 38%; children and adolescents, grade 3: 14%; children and adolescents, grades ≥4: 7%), febrile neutropenia (adults: 12%; adults, grade 3: 9%; adults, grades ≥4: 1%), petechia (adults: 12%; adults, grade 3: 2%)
Hepatic: Increased serum transaminases (children and adolescents: 12%)
Neuromuscular & skeletal: Asthenia (adults: 17%; children and adolescents: 6%), myalgia (adults: 13%)
Respiratory: Cough (adults: 25%), dyspnea (adults: 20%)
Miscellaneous: Fever (adults: 23%)
1% to 10%:
Cardiovascular: Hypotension (adults: 8%), sinus tachycardia (adults: 8%), chest pain (adults: 5%)
Central nervous system: Ataxia (adults: 9%; children and adolescents: 2%), confusion (adults: 8%), myasthenia (adults: 8%), rigors (adults: 8%), insomnia (adults: 7%), peripheral motor neuropathy (4% to 7%; grade 3: 1% to 2%), abnormal gait (adults: 6%), depression (adults: 6%), impaired consciousness (adults: 6%), seizure (children and adolescents: 6%; adults, grade 3: 1%), peripheral neuropathy (5% to 6%; grade 3: 1% to 2%), noncardiac chest pain (adults: 5%), motor dysfunction (children and adolescents: 4%), neuropathy (adults: 4%), amnesia (adults: 3%), balance impairment (adults: 2%), abnormal sensory symptoms (1% to 2%), aphasia (adults, grade 3: 1%), burning sensation (adults: 1%), cerebral hemorrhage (adults, grade 4: 1%), cranial nerve palsy (third and sixth nerve, children and adolescents: 1%), coma (adults, grade 4: 1%), disturbance in attention (adults: 1%), dysarthria (1%), encephalopathy (children and adolescents, grade 4: 1%), hemiparesis (adults, grade 3: 1%), hydrocephalus (children and adolescents: 1%), hypertonia (children and adolescents, grade 3: 1%), hyporeflexia (1%), intracranial hemorrhage (adults, grade 4: 1%), lethargy (children and adolescents: 1%), leukoencephalopathy (adults, grade 4: 1%), loss of consciousness (adults, grade 3: 1%), mental status changes (children and adolescents: 1%), nerve palsy (adults: 1%), paralysis (children and adolescents: 1%), neuralgia (adults: 1%), sciatica (adults: 1%), speech disturbance (adults: 1%), status epilepticus (children and adolescents: 1%)
Endocrine & metabolic: Decreased serum albumin (children and adolescents: 10%), decreased serum calcium (children and adolescents: 8%), dehydration (adults: 7%), decreased serum glucose (children and adolescents: 6%), decreased serum magnesium (children and adolescents: 6%), hyperglycemia (adults: 6%)
Gastrointestinal: Abdominal pain (adults: 9%), anorexia (adults: 9%), stomatitis (adults: 8%; grade 3: 1%), abdominal distention (adults: 6%), dysgeusia (adults: 3%)
Hepatic: Increased serum bilirubin (children and adolescents: 10%), increased serum aspartate aminotransferase (adults: 6%)
Infection: Infection (5% to 9%)
Neuromuscular & skeletal: Arthralgia (adults: 9%), back pain (adults: 8%), limb pain (adults: 7%), tremor (4% to 5%)
Ophthalmic: Blurred vision (adults: 4%), nystagmus disorder (adults: 1%)
Renal: Increased serum creatinine (children and adolescents: 6%)
Respiratory: Pleural effusion (adults: 10%), epistaxis (adults: 8%), pneumonia (adults: 8%), dyspnea on exertion (adults: 7%), sinusitis (adults: 7%), wheezing (adults: 5%), sinus headache (adults: 1%)
Postmarketing: Demyelinating disease, increased creatine phosphokinase in blood specimen, opportunistic infection, progressive multifocal leukoencephalopathy, rhabdomyolysis, tumor lysis syndrome
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: Leukopenia, thrombocytopenia, anemia, and neutropenia (including neutropenic fever) are associated with nelarabine treatment. Monitor blood counts regularly.
- CNS depression: Nelarabine may cause somnolence during and for several days after treatment, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
- Neurotoxicity: [US Boxed Warning]: Severe neurotoxicities, including mental status changes, severe somnolence, seizures, and peripheral neuropathy (ranging from numbness and paresthesias to motor weakness and paralysis), have been reported. Monitor frequently during treatment for signs and symptoms of neurotoxicity; discontinue if ≥ grade 2. Adverse reactions associated with demyelination and ascending peripheral neuropathies similar in appearance to Guillain-Barré syndrome have also been reported. Neurologic toxicities may not fully return to baseline after treatment cessation. Common signs and symptoms of neurotoxicity include somnolence, headache, paresthesia, dysesthesia, dizziness, neuropathy (sensory and motor), cerebellar disturbances, tremor, and, in severe cases, coma, status epilepticus, craniospinal demyelination, and ascending neuropathy. Symptom onset from start of first infusion is often within a median of 5 to 8 days (range: 1 to 269 days), with a median duration of 2 to 6 days (range: 1 to 393 days). Monitor closely for neurologic toxicity during and for at least 24 hours after each treatment. Risk of neurotoxicity may be increased in patients with concurrent or previous intrathecal chemotherapy or prior craniospinal irradiation.
- Tumor lysis syndrome: Tumor lysis syndrome (TLS) may occur as a consequence of leukemia treatment. May lead to life-threatening acute renal failure. Ensure adequate hydration prior to and during treatment to prevent hyperuricemia and TLS; consider prophylactic antihyperuricemic therapy. Monitor closely.
Disease-related concerns:
- Hepatic impairment: Monitor closely for toxicities. Risk of adverse reactions may be higher with severe hepatic dysfunction.
- Renal impairment: Monitor closely for toxicities. Ara-G clearance may be reduced with renal dysfunction and the risk of adverse reactions may be higher in patients with moderate to severe impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Vaccines: Avoid administration of live vaccines to immunocompromised patients.
Monitoring Parameters
CBC with differential, liver and kidney function; verify pregnancy status prior to therapy initiation in females of reproductive potential; monitor closely for neurologic toxicity (severe somnolence, seizure, peripheral neuropathy, confusion, ataxia, paresthesia, hypoesthesia, coma, or craniospinal demyelination), especially during and for at least 24 hours after each treatment; monitor for signs and symptoms of tumor lysis syndrome; monitor hydration status
Pregnancy
Pregnancy Considerations
Based on its mechanism of action and findings in animal reproduction studies, nelarabine may cause fetal harm if administered during pregnancy. Verify pregnancy status in females of reproductive potential prior to therapy initiation. Females of reproductive potential should use effective contraception during nelarabine therapy. Male patients (including those who have had vasectomies) with female partners of reproductive potential should use condoms during nelarabine treatment and for 3 months after the last nelarabine dose.
The European Society for Medical Oncology has published guidelines for diagnosis, treatment, and follow-up of cancer during pregnancy. The guidelines recommend referral to a facility with expertise in cancer during pregnancy and encourage a multidisciplinary team (obstetrician, neonatologist, oncology team). In general, if chemotherapy is indicated, it should be avoided during the first trimester, there should be a 3-week time period between the last chemotherapy dose and anticipated delivery, and chemotherapy should not be administered beyond week 33 of gestation. Specific use of nelarabine is not discussed (Peccatori 2013).
Patient Education
What is this drug used for?
- It is used to treat types of leukemia and lymphoma.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Constipation
- Diarrhea
- Back pain
- Abdominal pain
- Mouth irritation
- Mouth sores
- Abdominal swelling
- Lack of appetite
- Trouble sleeping
- Headache
- Joint pain
- Tremors
- Painful extremities
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Fluid and electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, severe dizziness, passing out, fast heartbeat, increased thirst, seizures, loss of strength and energy, lack of appetite, not passing urine or change in amount of urine passed, dry mouth, dry eyes, or nausea or vomiting
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
- Shortness of breath
- Pale skin
- Bruising
- Bleeding
- Severe loss of strength and energy
- Confusion
- Severe fatigue
- Not able to move
- Burning or numbness feeling
- Change in balance
- Seizures
- Trouble with performing functions of daily living
- Abnormal gait
- Chest pain
- Fast heartbeat
- Swelling
- Severe dizziness
- Passing out
- Muscle weakness
- Depression
- Tumor lysis syndrome like fast heartbeat or abnormal heartbeat; any passing out; unable to pass urine; muscle weakness or cramps; nausea, vomiting, diarrhea or lack of appetite; or feeling sluggish
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.