Boxed Warning
Hepatotoxicity:
Severe, life-threatening, and, in some cases, fatal hepatotoxicity, particularly in the first 18 weeks, has been reported in patients treated with nevirapine. In some cases, patients presented with nonspecific prodromal signs or symptoms of hepatitis and progressed to hepatic failure. These events are often associated with rash. Women and patients with higher CD4+ cell counts at initiation of therapy are at increased risk. Women with CD4+ cell counts higher than 250 cells/mm3, including pregnant women receiving nevirapine in combination with other antiretrovirals for treatment of HIV-1 infection, are at the greatest risk. However, hepatotoxicity associated with nevirapine use can occur in both genders, at all CD4+ cell counts, and at any time during treatment. Hepatic failure has also been reported in patients without HIV taking nevirapine for postexposure prophylaxis. Use of nevirapine for occupational and nonoccupational postexposure prophylaxis is contraindicated. Patients with signs or symptoms of hepatitis, or with increased transaminases combined with rash or other systemic symptoms, must discontinue nevirapine and seek medical evaluation immediately.
Skin reactions:
Severe, life-threatening skin reactions, including fatal cases, have occurred in patients treated with nevirapine. These have included cases of Stevens-Johnson syndrome, toxic epidermal necrolysis, and hypersensitivity reactions characterized by rash, constitutional findings, and organ dysfunction. Patients developing signs or symptoms of severe skin reactions or hypersensitivity reactions must discontinue nevirapine and seek medical evaluation immediately. Check transaminase levels immediately for all patients who develop a rash in the first 18 weeks of treatment. The 14-day lead-in period with nevirapine 200 mg immediate release daily dosing has been observed to decrease the incidence of rash and must be followed.
Monitoring for hepatotoxicity and skin reactions
Patients must be monitored intensively during the first 18 weeks of therapy with nevirapine to detect potentially life-threatening hepatotoxicity or skin reactions. Extra vigilance is warranted during the first 6 weeks of therapy, which is the period of greatest risk of these reactions. Do not restart nevirapine following clinical hepatitis, transaminase elevations combined with rash or other systemic symptoms, or following severe skin rash or hypersensitivity reactions. In some cases, hepatic injury has progressed despite discontinuation of treatment.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Suspension, Oral:
Viramune: 50 mg/5 mL (240 mL) [contains methylparaben, polysorbate 80, propylparaben, sorbitol]
Generic: 50 mg/5 mL (240 mL)
Tablet, Oral:
Viramune: 200 mg [scored]
Generic: 200 mg
Tablet Extended Release 24 Hour, Oral:
Viramune XR: 100 mg [DSC], 400 mg
Generic: 100 mg, 400 mg
Pharmacology
Mechanism of Action
As a non-nucleoside reverse transcriptase inhibitor, nevirapine has activity against HIV-1 by binding to reverse transcriptase. It consequently blocks the RNA-dependent and DNA-dependent DNA polymerase activities including HIV-1 replication. It does not require intracellular phosphorylation for antiviral activity.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and readily absorbed; Immediate release: >90%
Distribution
Widely; Vd: 1.2 L/kg; CSF penetration approximates 40% to 50% of plasma
Metabolism
Extensively hepatic via CYP3A4 and CYP2B6 (hydroxylation to inactive compounds); may undergo enterohepatic recycling
Excretion
Urine (~81%, primarily as metabolites, <3% as unchanged drug); feces (~10%)
Clearance: Women have a 13.8% lower clearance compared to men; Body size does not totally explain the gender difference
Time to Peak
Serum: Immediate release: 4 hours; Extended release:~24 hours
Half-Life Elimination
Decreases over 2- to 4-week time with chronic dosing due to autoinduction (ie, half-life = 45 hours initially [single dose] and decreases to 25 to 30 hours [multiple dosing])
Protein Binding
Plasma: ~60%
Use: Labeled Indications
HIV-1 infection: Treatment of HIV-1, in combination therapy with other antiretroviral agents, in adults and pediatric patients ≥15 days of age (immediate release) and ≥6 years of age with a BSA of ≥1.17 m2 (ER).
Limitations of use: Not recommended to be initiated, unless the benefit outweighs the risk, in adult females with CD4+ cell counts >250 cells/mm3 or adult males with CD4+ cell counts >400 cells/mm3.
Use: Off Label
Prevention of perinatal HIV transmissionyes
Based on the Health and Human Services (HHS) Perinatal HIV Guidelines, nevirapine, in combination with zidovudine, is a recommended regimen for prophylactic therapy and nevirapine, in combination with zidovudine and lamivudine, is a recommended regimen for empiric therapy to reduce the risk of perinatal transmission of HIV in HIV-exposed infants at higher risk of HIV-acquisition, including those born to HIV-infected women who did not receive antepartum or intrapartum antiretroviral drugs (ARV), who received only intrapartum ARV drugs, or who received antepartum and intrapartum ARV drugs but who had a detectable viral load near delivery (particularly if delivery was vaginal), or mothers with acute HIV infection during pregnancy or breastfeeding. There is a paucity of data to evaluate the optimal prophylactic therapy; however, the 2-drug regimen is currently preferred. Empiric therapy with the 3-drug regimen provides prophylaxis against HIV acquisition and provides early treatment if HIV infection is later confirmed.
Contraindications
Moderate to severe hepatic impairment (Child-Pugh class B or C); use in occupational or nonoccupational postexposure prophylaxis (PEP) regimens
Canadian labeling: Additional contraindications (not in US labeling): Clinically significant hypersensitivity to nevirapine or any component of the formulation; therapy rechallenge in patients with prior hypersensitivity reactions, severe rash, rash accompanied by constitutional symptoms, or clinical hepatitis due to nevirapine; severe hepatic dysfunction or AST or ALT >5 times ULN (pretreatment or during prior use of nevirapine); hereditary conditions of galactose intolerance (eg, galactosemia, Lapp lactase deficiency, glucose-galactose malabsorption); concomitant use of herbal products containing St John's wort
Dosage and Administration
Dosing: Adult
HIV-1 infection, treatment: Oral:
Note: Therapy in antiretroviral naive patients should not be initiated in patients with elevated CD4+-cell counts unless the benefit of therapy outweighs the risk of serious hepatotoxicity (adult/postpubertal females: CD4+-cell counts >250 cells/mm3; adult males: CD4+-cell counts >400 cells/mm3).
Initial: Immediate release: 200 mg once daily for 14 days
Maintenance:
Immediate release: 200 mg twice daily (in combination with additional antiretroviral agents) if there is no rash or untoward effects during initial dosing period
Extended release: 400 mg once daily; maintenance therapy using the extended release must follow a 14-day initial dosing period (lead-in) using the immediate release formulation unless patient is already maintained on a nevirapine immediate release regimen
Note: If patient experiences a non-severe rash (in the absence of transaminase elevations) during the 14-day lead-in period, dose should not be increased until the rash has resolved. A lead-in period must always be done with immediate-release formulation and regimen should not exceed 28 days; alternative treatment should be considered at that point. If a rash occurs within the first 18 weeks of therapy, immediately check serum transaminases. Discontinue if severe rash, rash with constitutional symptoms, or rash with elevated hepatic transaminases is noted. If therapy with any formulation is interrupted for >7 days, restart with initial dose of immediate-release formulation for 14 days.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
HIV-1 infection, treatment: Note: Use in combination with other antiretroviral (ARV) agents. Gene mutation and ARV resistance patterns should be evaluated (refer to https://www.iasusa.org/ for more information) when necessary.
Although lead-in dosing recommended in pediatric patients ≥2 years of age when initiating therapy to allow for enzymatic autoinduction and reduce the occurrence of rash, it may not be necessary in infants and children <2 years of age (HHS [pediatric] 2019). If patient experiences a nonsevere rash (in the absence of transaminase elevations) during the first 14 days of therapy, do not increase dose until rash has resolved. If rash continues beyond 28 days, use an alternative regimen. Discontinue nevirapine if severe rash, rash with constitutional symptoms, or rash with elevated hepatic transaminases occurs. If nevirapine therapy is interrupted for ≤14 days (infants/children) or <7 days (adolescents), restart at the full-dose due to mechanisms of nevirapine resistance, half-life of CYP enzymes, and clinical trial results (HHS [adult] 2019; HHS [pediatric] 2019).
AIDSinfo guidelines (HHS [pediatric] 2019):
Immediate release: Oral:
Infants and Children <8 years:
With lead-in dosing: Initial: 200 mg/m2/dose once daily (maximum dose: 200 mg/dose) for the first 14 days of therapy; increase to 200 mg/m2/dose twice daily (maximum dose: 200 mg/dose) if no rash or other adverse effects occur.
Without lead-in dosing: Infants and Children <2 years: 200 mg/m2/dose twice daily (maximum dose: 200 mg/dose); monitor patients for tolerability (eg, rash).
Children ≥8 years: Initial (lead-in dosing): 120 to 150 mg/m2/dose once daily (maximum dose: 200 mg/dose) for the first 14 days of therapy; increase to 120 to 150 mg/m2/dose twice daily (maximum dose: 200 mg/dose) if no rash or other adverse effects occur. Note: In a growing child, do not decrease the mg dose when the child reaches 8 years; leave the mg dose the same to achieve the appropriate mg/m2/dose as the child grows larger (as long as there are no adverse effects).
Adolescents: Initial: 200 mg once daily for the first 14 days; increase to 200 mg every 12 hours if no rash or other adverse effects occur; if patient able to swallow tablets whole, may convert maintenance dose to the extended release formulation (400 mg once daily).
Extended release: Oral: Note: For patients established on full-dose nevirapine, may initiate extended-release preparation without lead-in dosing. If initiating nevirapine therapy, begin with the age-appropriate once daily dose of the immediate-release formulation for the first 14 days of therapy; at 14 days, if no rash or other adverse effects have occurred, increase dose to the age-appropriate dose administered once daily for the extended-release formulation. Extended-release tablets should not be divided to achieve daily dose.
Children ≥6 years: Must be able to swallow tablets whole: BSA-directed dosing (HHS [pediatric] 2019):
BSA 0.58 to 0.83 m2: 200 mg once daily.
BSA 0.84 to 1.16 m2: 300 mg once daily.
BSA ≥1.17 m2: 400 mg once daily.
Adolescents: 400 mg once daily.
HIV-1 perinatal transmission, empiric therapy in neonates at high risk of transmission (3-drug regimen): Limited data available: (HHS [perinatal] 2018): Note: Dosing addresses completion of courses initiated at birth; if the neonate is diagnosed as HIV positive, discontinue empiric dosing and transition to a treatment regimen and monitoring (see HIV-1 infection, treatment). Recommended in combination with zidovudine and lamivudine for empiric treatment of HIV in neonates at higher risk of perinatal transmission; see guidelines for additional information on high-risk definitions (HHS [perinatal] 2018). Duration of therapy undefined; some experts suggest a full 6 weeks of therapy and others suggest that antiretroviral therapy can be discontinued once a negative nucleic acid test (NAT) is returned.
Infant ≤6 weeks: Oral: Immediate release: 200 mg/m2/dose twice daily; maximum dose: 200 mg/dose.
Administration
Oral: May be administered with or without food; may be administered with an antacid or didanosine. Shake suspension gently prior to administration; the use of an oral dosing syringe is recommended, especially if the dose is ≤5 mL; if using a dosing cup, after administration, rinse cup with water and also administer rinse. Extended release tablets must be swallowed whole and not crushed, chewed, or divided.
Storage
Store at 25°C (77°F); excursion permitted to 15°C to 30°C (59°F to 86°F).
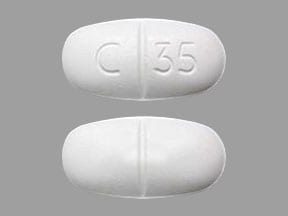
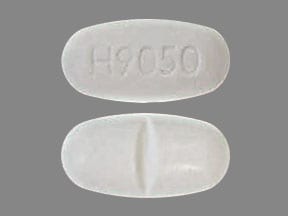
Nevirapine Images
Drug Interactions
Amodiaquine: Nevirapine may decrease the serum concentration of Amodiaquine. Monitor therapy
Artemether: Nevirapine may decrease the serum concentration of Artemether. Nevirapine may also increase or decrease serum concentrations of lumefantrine. Monitor therapy
Artesunate: Nevirapine may decrease serum concentrations of the active metabolite(s) of Artesunate. Nevirapine may increase the serum concentration of Artesunate. Monitor therapy
Atazanavir: May increase the serum concentration of Nevirapine. Nevirapine may decrease the serum concentration of Atazanavir. Avoid combination
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Cabozantinib: MRP2 Inhibitors may increase the serum concentration of Cabozantinib. Monitor therapy
CarBAMazepine: May decrease the serum concentration of Nevirapine. Avoid combination
Caspofungin: Inducers of Drug Clearance may decrease the serum concentration of Caspofungin. Management: Consider using an increased caspofungin dose of 70 mg daily in adults (or 70 mg/m2, up to a maximum of 70 mg, daily in pediatric patients) when coadministered with known inducers of drug clearance. Consider therapy modification
CloZAPine: CYP3A4 Inducers (Weak) may decrease the serum concentration of CloZAPine. Monitor therapy
CYP2B6 Substrates (High risk with Inducers): CYP2B6 Inducers (Moderate) may decrease the serum concentration of CYP2B6 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Daclatasvir: Nevirapine may decrease the serum concentration of Daclatasvir. Management: Increase the daclatasvir dose to 90 mg once daily. Consider therapy modification
Darunavir: May increase the serum concentration of Nevirapine. Nevirapine may increase the serum concentration of Darunavir. Management: No action is required if darunavir/ritonavir is combined with nevirapine. The combination of darunavir/cobicistat and nevirapine should be avoided. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Dolutegravir: Nevirapine may decrease the serum concentration of Dolutegravir. Avoid combination
Doravirine: Nevirapine may decrease the serum concentration of Doravirine. Avoid combination
Efavirenz: May enhance the adverse/toxic effect of Nevirapine. Nevirapine may enhance the adverse/toxic effect of Efavirenz. Nevirapine may decrease the serum concentration of Efavirenz. Avoid combination
Elvitegravir: Nevirapine may decrease the serum concentration of Elvitegravir. Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Ergonovine: Reverse Transcriptase Inhibitors (Non-Nucleoside) may increase the serum concentration of Ergonovine. Specifically, this would be most likely with delavrdine, while other Non-Nucleoside Reverse Transcriptase Inhibitors may be more likely to decrease the concentration of Ergonovine. Avoid combination
Estriol (Systemic): Nevirapine may decrease the serum concentration of Estriol (Systemic). Monitor therapy
Estriol (Topical): Nevirapine may decrease the serum concentration of Estriol (Topical). Monitor therapy
Etravirine: Reverse Transcriptase Inhibitors (Non-Nucleoside) may decrease the serum concentration of Etravirine. This has been observed with the NNRTIs efavirenz and nevirapine. Reverse Transcriptase Inhibitors (Non-Nucleoside) may increase the serum concentration of Etravirine. This has been observed with delavirdine. Avoid combination
Fluconazole: May increase the serum concentration of Nevirapine. Monitor therapy
Fosamprenavir: Nevirapine may decrease serum concentrations of the active metabolite(s) of Fosamprenavir. Management: Coadministration of nevirapine and fosamprenavir is not recommended without concurrent ritonavir. However, when nevirapine and fosamprenavir/ritonavir (twice daily) are used in combination, no dose adjustment is required. Consider therapy modification
Indinavir: Nevirapine may decrease the serum concentration of Indinavir. Management: Increased indinavir doses may be needed when used with nevirapine; however, specific dosing guidelines have not been established. Consider therapy modification
Itraconazole: Nevirapine may decrease the serum concentration of Itraconazole. Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Ketoconazole (Systemic): Nevirapine may decrease the serum concentration of Ketoconazole (Systemic). Avoid combination
Letermovir: Nevirapine may diminish the therapeutic effect of Letermovir. Avoid combination
Levomethadone: Reverse Transcriptase Inhibitors (Non-Nucleoside) may decrease the serum concentration of Levomethadone. Management: Levomethadone dosage adjustments will likely be required with efavirenz and nevirapine, and may be necessary with rilpivirine as well. Monitor therapy
Lopinavir: Nevirapine may decrease the serum concentration of Lopinavir. Management: Avoid once daily use of lopinavir/ritonavir with nevirapine. Avoid use of this combination in patients less than 6 months of age. See lopinavir/ritonavir prescribing information for recommended dose increases in other patients. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Methadone: Reverse Transcriptase Inhibitors (Non-Nucleoside) may increase the metabolism of Methadone. Management: Methadone dosage adjustments will likely be required with efavirenz and nevirapine, and may be necessary with rilpivirine as well. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Nelfinavir: Nevirapine may decrease serum concentrations of the active metabolite(s) of Nelfinavir. Nevirapine may decrease the serum concentration of Nelfinavir. Monitor therapy
NiMODipine: CYP3A4 Inducers (Weak) may decrease the serum concentration of NiMODipine. Monitor therapy
Orlistat: May decrease the serum concentration of Antiretroviral Agents. Monitor therapy
QuiNINE: Nevirapine may decrease the serum concentration of QuiNINE. Monitor therapy
Rifabutin: Nevirapine may increase serum concentrations of the active metabolite(s) of Rifabutin. Nevirapine may increase the serum concentration of Rifabutin. Monitor therapy
RifAMPin: May decrease the serum concentration of Nevirapine. Management: Avoid whenever possible. When this combination is necessary, use immediate-release nevirapine (avoid extended-release nevirapine) at a dose of 200 mg twice daily with no lead-in (per adult/adolescent HIV guidelines). Monitor nevirapine response closely. Consider therapy modification
Rilpivirine: Reverse Transcriptase Inhibitors (Non-Nucleoside) may increase the serum concentration of Rilpivirine. This mechanism applies to coadministration of delavirdine. Reverse Transcriptase Inhibitors (Non-Nucleoside) may decrease the serum concentration of Rilpivirine. This mechanism applies to coadministration of efavirenz, etravirine, and nevirapine. Avoid combination
Rivaroxaban: Nevirapine may decrease the serum concentration of Rivaroxaban. Monitor therapy
Saquinavir: Nevirapine may decrease the serum concentration of Saquinavir. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: Nevirapine may decrease the serum concentration of Simeprevir. Avoid combination
St John's Wort: May decrease the serum concentration of Reverse Transcriptase Inhibitors (Non-Nucleoside). Specifically, St. Johns Wort may increase the metabolism of Reverse Transcriptase Inhibitors (Non-Nucleoside). Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Ubrogepant: CYP3A4 Inducers (Weak) may decrease the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 100 mg and second dose (if needed) of 100 mg when used with a weak CYP3A4 inducer. Consider therapy modification
Velpatasvir: CYP2B6 Inducers (Moderate) may decrease the serum concentration of Velpatasvir. Avoid combination
Voriconazole: Reverse Transcriptase Inhibitors (Non-Nucleoside) may decrease the serum concentration of Voriconazole. Voriconazole may increase the serum concentration of Reverse Transcriptase Inhibitors (Non-Nucleoside). Management: Consider avoiding when possible. Use efavirenz with voriconazole only if voriconazole is dosed at 400 mg every 12 hours and efavirenz is dosed at 300 mg daily (adult doses) throughout therapy. Avoid Atripla (efavirenz/emtricitabine/tenofovir). Consider therapy modification
Warfarin: Nevirapine may diminish the anticoagulant effect of Warfarin. Monitor therapy
Adverse Reactions
>10%:
Endocrine & metabolic: Increased serum cholesterol (3% to 19%), increased LDL cholesterol (5% to 15%)
Hematologic & oncologic: Decreased serum phosphate (≤38%), neutropenia (1% to 13%)
Hepatic: Increased serum alanine aminotransferase (2% to 14%)
1% to 10%:
Central nervous system: Fatigue (2% to 5%), headache (1% to 4%)
Dermatologic: Skin rash (4% to 7%; children: 1%)
Endocrine & metabolic: Increased amylase (≤5%)
Gastrointestinal: Nausea (1% to 9%), abdominal pain (2% to 3%), diarrhea (2% to 4%)
Hematologic & oncologic: Granulocytopenia (≤2%)
Hepatic: Increased serum aspartate aminotransferase (2% to 9%), increased serum transaminases (asymptomatic; >5x ULN: 6%), hepatic disease (4%), hepatitis (2% to 4%; may be hypersensitivity related)
Neuromuscular & skeletal: Arthralgia (2%)
Miscellaneous: Fever (1% to 2%)
Frequency not defined:
Dermatologic: Erythematous maculopapular rash, pruritus
<1%, postmarketing, and/or case reports: Abnormal transaminase, anaphylaxis, anemia, angioedema, aphthous stomatitis, autoimmune disease, bullous rash, cholestatic hepatitis, conjunctivitis, DRESS syndrome, drowsiness, drug withdrawal, eosinophilia, facial edema, flu-like symptoms, fulminant hepatitis, Graves disease, Guillain-Barre syndrome, hepatic encephalopathy, hepatic failure, hepatic necrosis, hepatomegaly, hepatotoxicity, hyperbilirubinemia, hypersensitivity reaction, immune reconstitution syndrome, jaundice, lipotrophy, liver tenderness, lymphadenopathy, malaise, myalgia, oral lesion, paresthesia, polymyositis, prolonged partial thromboplastin time, redistribution of body fat, renal insufficiency, rhabdomyolysis, skin blister, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria, vomiting
Warnings/Precautions
Concerns related to adverse effects:
- Fat redistribution: May cause redistribution/accumulation of fat (eg, central obesity, buffalo hump, peripheral wasting, facial wasting, breast enlargement, cushingoid appearance).
- Hepatotoxicity: [US Boxed Warning]: Severe, life-threatening, and in some cases fatal hepatotoxicity, particularly in the first 18 weeks, has been reported in patients treated with nevirapine. In some cases, patients have presented with non-specific prodromal signs/symptoms of hepatitis that have progressed to hepatic failure. May be associated with rash. Risk is greatest in the first 6 weeks of therapy. Female gender and higher CD4+ cell counts at treatment initiation increase risk of hepatotoxicity; women with CD4+ cell counts >250 cells/mm3, including pregnant women, are at greatest risk. Hepatic failure has also been reported in patients without HIV taking nevirapine for post-exposure prophylaxis (PEP); use is contraindicated for occupational or non-occupational PEP. Monitor patients intensively during the first 18 weeks of therapy. Discontinue treatment in patients with signs/symptoms of hepatitis or with increased transaminases combined with rash or other systemic symptoms; in some cases, hepatic injury has progressed despite discontinuation. Do not restart nevirapine following clinical hepatitis or transaminase elevations combined with rash or other systemic symptoms. Patients with a history of chronic hepatitis (B or C) or increased baseline transaminase levels may be at increased risk of later symptomatic events (≥6 weeks after treatment initiation) and asymptomatic increases in AST or ALT.
- Immune reconstitution syndrome: Patients may develop immune reconstitution syndrome, resulting in the occurrence of an inflammatory response to an indolent or residual opportunistic infection during initial HIV treatment or activation of autoimmune disorders (eg, Graves disease, polymyositis, Guillain-Barré syndrome) later in therapy; further evaluation and treatment may be required.
- Rhabdomyolysis: Has been observed in conjunction with skin and/or hepatic adverse events. Discontinuation of therapy is warranted with evidence of severe skin or liver toxicity.
- Skin reactions: [US Boxed Warning]: Severe, life-threatening skin reactions (eg, Stevens-Johnson syndrome, toxic epidermal necrolysis, hypersensitivity reactions with rash and organ dysfunction), including fatal cases, have occurred. The 14-day lead-in dosing period must be followed and has been shown to decrease incidence of rash. The greatest risk of these reactions is within the initial 6 weeks of treatment; intensive monitoring is required during the initial 18 weeks of therapy to detect potentially life-threatening dermatologic and hypersensitivity reactions. Discontinue use in patients who develop signs/symptoms of severe skin reactions or hypersensitivity reactions; do not restart nevirapine in these patients. Immediately evaluate transaminase levels in all patients who develop rash in the first 18 weeks of treatment. If mild to moderate rash without constitutional symptoms occurs during the 14-day lead-in period, do not increase dose until resolution of rash. If rash continues beyond 28 days, consider an alternative regimen. Coadministration of prednisone during the first 6 weeks of therapy increases incidence and severity of rash; concomitant prednisone is not recommended to prevent rash.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with preexisting dysfunction; monitor closely for drug-induced hepatotoxicity. Use is contraindicated in patients with moderate to severe impairment (Child-Pugh class B or C).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy.
Dosage form specific issues:
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley, 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer's labeling.
Other warnings/precautions:
- Appropriate use: When initiating therapy, a 14-day lead-in dose with the immediate release formulation should be used to decrease risk of skin reactions. If rash appears during the 14-day lead-in period, do not increase the dose or initiate the extended release formulation until the rash has resolved. An alternative regimen should be used if the lead-in dose period exceeds 28 days. Therapy in antiretroviral naive patients should not be initiated in patients with elevated CD4+-cell counts unless the benefit of therapy outweighs the risk of serious hepatotoxicity (adult/postpubertal females: CD4+-cell counts >250 cells/mm3; adult males: CD4+-cell counts >400 cells/mm3). If CD4+-cell counts increase above these thresholds as a result of nevirapine-containing therapy, therapy may be continued. After the lead-in period, patients may be switched to the extended-release formulation.
- Resistance: Due to rapid emergence of resistance, nevirapine should not be used as monotherapy or the only agent added to a failing regimen for the treatment of HIV. Resistance may occur with a single mutation and cross-resistance may be conferred to other non-nucleoside reverse transcriptase inhibitors (HHS [adult] 2016). When discontinuing an antiretroviral regimen containing nevirapine, take into account the long half-life of nevirapine. If other agents with shorter half-lives are stopped concurrently, low nevirapine plasma concentrations may persist for a week or longer and virus resistance may subsequently develop.
Monitoring Parameters
Monitor CBC and viral load. Intensive monitoring is required during the initial 18 weeks of therapy to detect potentially life-threatening hepatic, dermatologic, and hypersensitivity reactions. Baseline and repeat liver function tests; optimal frequency has not been established, some experts recommend testing at baseline, prior to dose escalation, and 2 weeks post-escalation. HIV treatment guidelines for pediatric patients recommend AST/ALT testing at baseline, 2 and 4 weeks, and every 3 months thereafter (HHS [pediatric] 2016). Guidelines for adult patients recommend ALT, AST, and bilirubin should be monitored at baseline, 2 to 8 weeks, and every 3 to 6 months (HHS [adult] 2016). Assess/evaluate AST/ALT immediately in any patients with a rash.
Pregnancy
Pregnancy Considerations
Nevirapine has a high level of transfer across the human placenta.
No increased risk of overall birth defects following first trimester exposure according to data collected by the antiretroviral pregnancy registry. Maternal antiretroviral therapy (ART) may be associated with adverse pregnancy outcomes including preterm delivery, stillbirth, low birth weight, and small for gestational age infants. Actual risks may be influenced by maternal factors such as disease severity, gestational age at initiation of therapy, and specific ART regimen, therefore close fetal monitoring is recommended. Because there is clear benefit to appropriate treatment, maternal ART should not be withheld due to concerns for adverse neonatal outcomes. Long-term follow-up is recommended for all infants exposed to antiretroviral medications; children without HIV but who were exposed to ART in utero and develop significant organ system abnormalities of unknown etiology (particularly of the CNS or heart) should be evaluated for potential mitochondrial dysfunction.
[US Boxed Warning]: Severe, life-threatening, and in some cases fatal hepatotoxicity, particularly in the first 18 weeks, has been reported in patients treated with nevirapine. Female gender and higher CD4+ cell counts at initiation of therapy place patients at increased risk; women with CD4+ cell counts greater than 250 cells/mm3, including pregnant women receiving nevirapine in combination with other antiretrovirals for the treatment of HIV-1 infection, are at the greatest risk. Pregnancy itself does not appear to increase this risk. Patients must be monitored intensively during the first 18 weeks of therapy. Extra vigilance is warranted during the first 6 weeks of therapy, which is the period of greatest risk of these events.
The Health and Human Services (HHS) perinatal HIV guidelines do not recommend nevirapine as an initial non-nucleoside reverse transcriptase inhibitor for use in antiretroviral-naive pregnant patients because of the potential for adverse events, complex dosing, and low barrier to resistance. Use is not recommended (except in special circumstances) in pregnant females who have had ART therapy in the past but are restarting, who require a new ART regimen (due to poor tolerance or poor virologic response of current regimen), and who are not yet pregnant but are trying to conceive. Females who become pregnant while taking nevirapine may continue if viral suppression is effective and the regimen is well tolerated. Pharmacokinetics of the immediate-release formulation are not significantly altered during pregnancy; dose adjustment is not currently recommended (data not available for extended-release formulation).
In general, ART is recommended for all pregnant females living with HIV to keep the viral load below the limit of detection and reduce the risk of perinatal transmission. Therapy should be individualized following a discussion of the potential risks and benefits of treatment during pregnancy. Monitoring of pregnant females is more frequent than in nonpregnant adults. ART should be continued postpartum for all females living with HIV and can be modified after delivery.
Health care providers are encouraged to enroll pregnant females exposed to antiretroviral medications as early in pregnancy as possible in the Antiretroviral Pregnancy Registry (1-800-258-4263 or http://www.APRegistry.com). Health care providers caring for pregnant females living with HIV and their infants may contact the National Perinatal HIV Hotline (1-888-448-8765) for clinical consultation (HHS [perinatal] 2019).
Patient Education
What is this drug used for?
- It is used to treat HIV infection.
Frequently reported side effects of this drug
- Nausea
- Tablet shell in stool
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Kidney problems like not able to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Infection
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Change in body fat
- Loss of strength and energy
- Flu-like symptoms
- Joint pain
- Muscle pain
- Swollen glands
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.