Boxed Warning
Interstitial pneumonitis:
Interstitial pneumonitis has been reported in 2% of patients in controlled clinical trials in patients exposed to nilutamide. A small study in Japanese patients showed that 17% of patients developed interstitial pneumonitis. Reports of interstitial changes, including pulmonary fibrosis that led to hospitalization and death, have been reported rarely in postmarketing. Symptoms included exertional dyspnea, cough, chest pain, and fever. X-rays showed interstitial or alveolo-interstitial changes, and pulmonary function tests revealed a restrictive pattern with decreased diffusing capacity of lungs for carbon monoxide. Most cases occurred within the first 3 months of treatment with nilutamide, and most reversed with discontinuation of therapy. Perform a routine chest x-ray prior to initiating treatment with nilutamide. Consider baseline pulmonary function tests. Instruct patients to report any new or worsening shortness of breath that they experience while on nilutamide. If symptoms occur, immediately discontinue nilutamide until it can be determined if the symptoms are drug related.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Nilandron: 150 mg [contains corn starch]
Generic: 150 mg
Pharmacology
Mechanism of Action
Nilutamide is a nonsteroidal antiandrogen which blocks testosterone effects at the androgen receptor level, preventing androgen response.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and complete
Metabolism
Hepatic (extensive), forms active metabolites
Excretion
Urine (62%; <2% as unchanged drug); feces (1% to 7%)
Half-Life Elimination
Terminal: 38 to 59 hours; Metabolites: 59 to 126 hours
Use: Labeled Indications
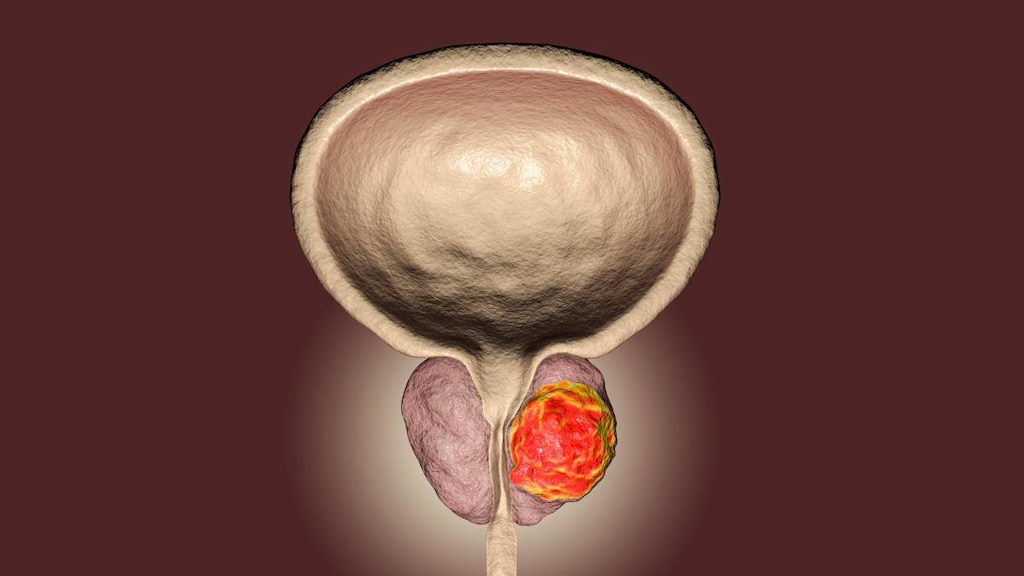
Prostate cancer, metastatic: Treatment of metastatic prostate cancer (in combination with surgical castration)
Contraindications
Hypersensitivity to nilutamide or any component of the formulation; severe hepatic impairment; severe respiratory insufficiency
Canadian labeling: Additional contraindications (not in US labeling): Use in women and children
Dosage and Administration
Dosing: Adult
Prostate cancer, metastatic: Oral: 300 mg once daily (starting the same day or day after surgical castration) for 30 days, followed by 150 mg once daily. Consider therapy discontinuation in patients with evidence of disease progression.
Dosing: Geriatric
Refer to adult dosing.
Administration
Administer without regard to meals.
Storage
Store at 25°C (77°F); excursions permitted between 15°C to 30°C (59°F to 86°F). Protect from light.
Nilutamide Images
Drug Interactions
Alcohol (Ethyl): Nilutamide may enhance the adverse/toxic effect of Alcohol (Ethyl). Specifically, nilutamide may increase the likelihood of alcohol intolerance (eg, facial flushing, malaise, hypotension). Avoid combination
Choline C 11: Antiandrogens may diminish the therapeutic effect of Choline C 11. Monitor therapy
CYP2C19 Inducers (Moderate): May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
CYP2C19 Inducers (Strong): May increase the metabolism of CYP2C19 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP2C19 Inhibitors (Moderate): May decrease the metabolism of CYP2C19 Substrates (High risk with Inhibitors). Monitor therapy
CYP2C19 Inhibitors (Strong): May decrease the metabolism of CYP2C19 Substrates (High risk with Inhibitors). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C19 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Conversely, concentrations of active metabolites may be increased for those drugs activated by CYP2C19. Management: Concurrent use of enzalutamide with CYP2C19 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C19 substrate should be performed with caution and close monitoring. Consider therapy modification
Indium 111 Capromab Pendetide: Antiandrogens may diminish the diagnostic effect of Indium 111 Capromab Pendetide. Avoid combination
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
Adverse Reactions
Reactions reported from monotherapy and combination therapy.
>10%:
Endocrine & metabolic: Hot flash (28%)
Ophthalmic: Nocturnal amblyopia (13% to 57%)
1% to 10%:
Cardiovascular: Hypertension (5%), cardiac failure (3%), angina pectoris (2%), edema (2%), syncope (2%)
Central nervous system: Dizziness (7%), paresthesia (3%), malaise (2%), nervousness (2%)
Dermatologic: Pruritus (2%)
Endocrine & metabolic: Hyperglycemia (4%), increased haptoglobin (2%), weight loss (2%)
Gastrointestinal: Nausea (10%), constipation (7%), diarrhea (2%), gastrointestinal hemorrhage (2%), melena (2%), xerostomia (2%)
Hematologic & oncologic: Leukopenia (3%)
Hepatic: Increased serum ALT (8%), increased serum AST (8%), increased serum alkaline phosphatase (3%)
Neuromuscular & skeletal: Arthritis (2%)
Ophthalmic: Visual disturbance (7%), cataract (2%), photophobia (2%)
Renal: Increased blood urea nitrogen (2%), increased serum creatinine (2%)
Respiratory: Dyspnea (6%), cough (2%), interstitial pneumonitis (2%), rhinitis (2%)
Miscellaneous: Alcohol intolerance (5%)
<1%, postmarketing, and/or case reports: Anxiety, aplastic anemia, cold extremities, gynecomastia, headache, hepatic injury, hepatitis, maculopapular rash, palpitations, prolonged Q-T interval on ECG, urticaria, vomiting, weight gain
Warnings/Precautions
Concerns related to adverse effects:
- Hematologic: Anemia may occur with testosterone suppression; monitor CBC periodically as indicated. Aplastic anemia has been reported (postmarketing case reports).
- Hepatotoxicity: Hepatitis or marked increases in liver enzymes leading to drug discontinuation occurred in 1% of patients receiving nilutamide in controlled studies. Rare cases of hospitalization or deaths due to severe liver injury have been reported, with the onset of hepatotoxicity usually occurring within first 3 to 4 months of therapy. Monitor transaminases. Signs/symptoms of hepatic dysfunction (nausea/vomiting, abdominal pain, anorexia, fatigue, flu-like symptoms, dark urine, jaundice, and/or right upper quadrant pain) should prompt liver function testing. Discontinue treatment immediately for jaundice or ALT >2 times the upper limit of normal (ULN).
- Interstitial pneumonitis: [US Boxed Warning]: Interstitial pneumonitis has been reported in 2% of patients exposed to nilutamide in controlled studies. An increased incidence has been observed in one small study of Japanese patients. Symptoms typically include exertional dyspnea, cough, chest pain, and fever; interstitial changes (including pulmonary fibrosis) leading to hospitalization and fatalities have been reported (rarely). Most cases occurred within the first 3 months of treatment and most reversed after discontinuation. X-rays showed interstitial or alveolo-interstitial changes; pulmonary function tests revealed a restrictive pattern with decreased DLco. Perform chest x-ray prior to treatment initiation and consider baseline pulmonary function testing. Instruct patients to report new or worsening dyspnea. Discontinue nilutamide immediately if signs and/or symptoms of interstitial pneumonitis are observed until a causal effect can be ruled out.
- Vision effects: A delay in adaptation to dark has been reported; in clinical studies, this was reported by 13% to 57% of patients. The delay ranged from seconds to a few minutes after passing from a light to a dark area. This may not abate with continued treatment although may be alleviated by wearing tinted sunglasses. Caution patients who experience adaptation delay about driving at night or through tunnels.
Disease-related concerns:
- Cardiovascular disease: Androgen-deprivation therapy may increase the risk for cardiovascular disease (Levine, 2010). Androgen deprivation therapy with other antiandrogen agents has resulted in prolongation of the QT/QTc interval (Garnick, 2004); evaluate risk versus benefit in patients with congenital long QT syndrome, heart failure, frequent electrolyte abnormalities, and in patients taking medication known to prolong the QT interval. Correct electrolytes prior to initiation and consider periodic electrolyte and ECG monitoring in patients at risk for QT prolongation.
- Decreased bone mineral density: Prolonged use of antiandrogen therapy is associated with decreased bone mineral density and an increased risk of osteoporosis and fracture (Smith, 2003); alcohol abuse, familial history of osteoporosis, and/or chronic use of drugs capable of decreasing bone mass (eg, corticosteroids) may increase risk. Evaluate risk carefully before initiating therapy.
- Diabetes: Hyperglycemia has been observed; use with caution in diabetic patients and monitor for loss of glucose control.
Special populations:
- Females: Not indicated for use in women.
- Pediatrics: Not indicated for use in pediatric patients.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Antiandrogen withdrawal syndrome: Patients with disease progression while receiving antiandrogen therapy may experience clinical improvement with discontinuation of the antiandrogen.
- Ethanol use: Approximately 5% of patients experience intolerance (facial flushing, hypotension, malaise) when ethanol is combined with nilutamide. Instruct patients to avoid ethanol.
Monitoring Parameters
CBC (periodic), liver function tests (transaminases; at baseline, regularly during the first 4 months of treatment, and then periodically thereafter; more frequently if clinically indicated), electrolytes, serum testosterone, PSA, blood glucose and/or glycosylated hemoglobin (HbA1c) in patients with diabetes; chest x-ray (baseline); consider pulmonary function testing (baseline); bone-mineral density (as clinically indicated in patients at risk of osteoporosis); ECG; signs and symptoms of liver dysfunction; vision changes. If initiating nilutamide in patients who are on warfarin, closely monitor prothrombin time.
Pregnancy
Pregnancy Considerations
Animal reproduction studies have not been conducted. Nilutamide is not indicated for use in women.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience hot flashes, nausea, dizziness, alopecia, decreased sex drive, constipation, dyspepsia, flu-like symptoms, lack of appetite, osteodynia, trouble sleeping, hyperhydrosis, or xeroderma. Have patient report immediately to prescriber chest pain, severe headache, vision changes, considerable asthenia, depression, paresthesia, dyspnea, excessive weight gain, edema of extremities, hematemesis, melena, or signs of hepatic impairment (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for healthcare professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience and judgment in diagnosing, treating and advising patients.