Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
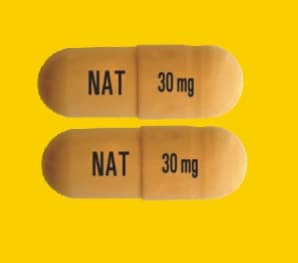
Capsule, Oral, as phosphate:
Tamiflu: 30 mg, 45 mg, 75 mg
Generic: 30 mg, 45 mg, 75 mg
Suspension Reconstituted, Oral, as base:
Tamiflu: 6 mg/mL (60 mL) [contains saccharin sodium, sodium benzoate, sorbitol; tutti-frutti flavor]
Generic: 6 mg/mL (60 mL)
Pharmacology
Mechanism of Action
Oseltamivir, a prodrug, is hydrolyzed to the active form, oseltamivir carboxylate (OC). OC inhibits influenza virus neuraminidase, an enzyme known to cleave the budding viral progeny from its cellular envelope attachment point (neuraminic acid) just prior to release.
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed
Distribution
Vd: Oseltamivir carboxylate:
Pediatric patients (Kimberlin 2013):
≤2 months: Median: 5.8 L/kg; Range: 2.97 to 44.91 L/kg.
3 to 5 months: Median: 10.4 L/kg; Range: 4.03 to 13.94 L/kg.
6 to 8 months: Median: 10.19 L/kg; Range: 1.39 to 107.59 L/kg.
9 to 11 months:
3 mg/kg: Median: 15.13 L/kg; Range: 5.46 to 95.3 L/kg.
3.5 mg/kg: Median: 10.41 L/kg; Range: 7.04 to 21.56 L/kg.
12 to 23 months:
3.5 mg/kg: Median: 24.36 L/kg; Range: 8.97 to 47.37 L/kg.
30 mg (fixed dose): Median: 13.92 L/kg; Range: 5.89 to 53.31 L/kg.
Adults: 23 to 26 L; may be significantly increased in patients receiving ECMO (Lemaitre 2012; Mulla 2013).
Metabolism
Hepatic (90%) to oseltamivir carboxylate; neither the parent drug nor active metabolite has any effect on the cytochrome P450 system
Excretion
Urine (>99% as oseltamivir carboxylate); feces (<20%)
Half-Life Elimination
Pediatric patients (Kimberlin 2013): Oseltamivir carboxylate:
≤2 months: Median: 6.64 hours; Range: 4.65 to 28.71 hours.
3 to 5 months: Median: 9.09 hours; Range: 6.25 to 19 hours.
6 to 8 months: Median:10.29 hours; Range: 1.02 to 78.26 hours.
9 to 11 months:
3 mg/kg: Median: 11.13 hours; Range: 5.4 to 51.86 hours.
3.5 mg/kg: Median: 14.56 hours; Range: 7.22 to 25.67 hours.
12 to 23 months:
3.5 mg/kg: Median: 14.82 hours; Range: 8.13 to 20.16 hours.
30 mg (fixed dose): Median: 7.98 hours; Range: 4.49 to 17.11 hours.
Adults: Oseltamivir: 1 to 3 hours; Oseltamivir carboxylate: 6 to 10 hours.
Protein Binding
Plasma: Oseltamivir carboxylate: 3%; Oseltamivir: 42%
Use in Specific Populations
Special Populations: Renal Function Impairment
Exposure to the active metabolite is inversely proportional to declining renal function. In continuous ambulatory peritoneal dialysis (CAPD) patients, the peak concentration of the active metabolite following a single 30 mg oseltamivir dose or once weekly oseltamivir was 3-fold higher than in patients with normal renal function receiving the approved adult dose. Administration of 30 mg once weekly to CAPD patients resulted in plasma concentrations of active metabolite comparable to patients with normal renal function receiving the approved adult doses.
Special Populations: Elderly
Exposure to the active metabolite at steady state was 25% to 35% higher in elderly patients.
Special Populations: Children
Preterm neonates have decreased clearance of oseltamivir due to immature renal function (AAP 2019). Exposure to active metabolite (oseltamivir carboxylate) is more variable in neonates and young infants (<9 months of age) due to maturation and greater variability of the carboxylesterase HCE-1; formation of active metabolite may be delayed, but overall exposure is similar. Clearance of the active metabolite increases throughout infancy. Exposures in these patients may be lower for similar mg/kg doses, particularly beginning at age 9 months (Kimberlin 2013). Children ≤12 years of age clear the prodrug and active metabolite faster than adults, resulting in a lower exposure with a given mg/kg dose. The pharmacokinetics of the prodrug in patients >12 years of age are similar to adult patients.
Use: Labeled Indications
Influenza, seasonal, prophylaxis: Prophylaxis of influenza (A or B) infection in patients ≥1 year of age.
Influenza, seasonal, treatment: Treatment of uncomplicated acute illness due to influenza (A or B) infection in patients ≥2 weeks of age who have been symptomatic for no more than 48 hours.
Note: The Advisory Committee on Immunization Practices (ACIP) recommends that treatment and prophylaxis be given to children <1 year of age when indicated (CDC 2018a).
Limitations of use: Not a substitute for annual influenza vaccination. Consider available information on influenza drug susceptibility patterns and treatment effects when deciding whether to use oseltamivir. Not recommended for patients with ESRD not undergoing dialysis.
Use: Off Label
Influenza A, avian (H7N9 or H5N1), prophylaxisc
Based on CDC interim guidance on influenza antiviral chemoprophylaxis of persons exposed to birds with avian influenza A viruses associated with severe human disease or with the potential to cause severe human disease, oseltamivir may be considered for postexposure prophylaxis in all persons exposed to avian influenza A viruses (H7N9 or H5N1) associated with severe human disease or with the potential to cause severe human disease CDC 2016a.
Influenza A, avian (H7N9 or H5N1), treatmentc
Based on CDC interim guidance on the use of antiviral medications for treatment of human infections with novel influenza A viruses associated with severe human disease, oseltamivir is recommended for treatment of influenza in hospitalized patients and outpatients with severe, complicated, or progressive illness due to avian influenza A virus (H7N9 or H5N1). Oseltamivir may also be considered in outpatients with uncomplicated illness due to avian influenza A virus (H7N9 or H5N1). Most human infections of avian influenza A H7N9 or H5N1 virus occur after exposure to infected poultry or contaminated environments. Rare instances of limited person-to-person spread have been identified outside of the US, but there is no evidence of sustained person-to-person spread CDC 2016b.
Contraindications
Hypersensitivity to oseltamivir or any component of the formulation
Dosage and Administration
Dosing: Adult
Influenza, seasonal, prophylaxis: Oral: 75 mg once daily
Postexposure prophylaxis: Note: Consider use in patients at very high risk for influenza complications (eg, severely immunocompromised patients) who have had close contact within the past 48 hours with a person with confirmed or suspected influenza during that person's infectious period (IDSA [Uyeki 2019]). Some experts also suggest use in patients at high risk (see Persons at increased risk for complications below) (Zachary 2019). Continue for 1 week after last exposure (if previously vaccinated) or 2 weeks (if unvaccinated). In unvaccinated patients, administer the influenza vaccine upon presentation (CDC 2018a).
Institutional outbreaks: Recommended for all residents regardless of vaccination status and continued for at least 2 weeks and 1 week after the last known case. Consider prophylaxis in employees, depending on vaccination status (CDC 2018a; IDSA [Uyeki 2019]).
Preexposure prophylaxis: Only during widespread outbreaks for persons at very high risk for influenza complications (eg, severely immunocompromised patients) not protected by vaccination. Continue for the duration of influenza activity or for 2 weeks following vaccination (IDSA [Uyeki 2019]).
Influenza, seasonal, treatment: Oral: 75 mg twice daily (CDC 2018a). Note: Higher doses (150 mg twice daily) are not currently recommended even in severely ill or immunocompromised patients (Ariano 2010; CDC 2018a; Lee 2013; SEAICRN 2013).
Timing of initiation/target population: In patients with severe, complicated, or progressive illness; hospitalized patients; or those at increased risk for complications (see Persons at increased risk for complications below), initiate treatment as soon as possible even if >48 hours have elapsed since illness onset and do not delay for laboratory confirmation. For symptomatic outpatients with mild illness not at increased risk for complications, treatment can be considered only if it can be initiated ≤48 hours following illness onset (CDC 2018a; IDSA [Uyeki 2019]).
Duration of therapy: Usual duration: 5 days; a longer duration can be considered in severely ill or immunocompromised patients (CDC 2018a).
Influenza A, avian (H7N9 or H5N1), prophylaxis (off-label use): Postexposure prophylaxis: Oral: 75 mg twice daily (CDC 2016a; CDC 2017)
Target population: Postexposure chemoprophylaxis can be considered for exposed persons; decisions to initiate chemoprophylaxis should be based on clinical judgment with consideration given to the type of exposure and to whether the person is at high risk for complications from influenza (see Persons at increased risk for complications below). Also refer to the CDC website for additional information (CDC 2016a; CDC 2017).
Duration of therapy: 5 days (from the last known exposure) if exposure was time-limited and not ongoing or 10 days if exposure is likely to be ongoing (eg, household setting) due to potential for prolonged infectiousness in the case-patient (CDC 2016a; CDC 2017).
Influenza A, avian (H7N9 or H5N1), treatment (off-label use): Oral: 75 mg twice daily (CDC 2016b). Note: Higher doses (150 mg twice daily) are not currently recommended even in severely ill or immunocompromised patients (Ariano 2010; CDC 2016b; Wang 2018). Initiate as soon as possible, even if >48 hours have elapsed since illness onset. Do not delay treatment while awaiting lab results. The usual duration is 5 days, but consider longer courses (eg, 10 days) for severely ill hospitalized patients (CDC 2016b).
Note: Persons at increased risk for complications: Adults ≥65 years of age, women who are pregnant or postpartum (within 2 weeks after delivery), residents of long-term care facilities, Native Americans and Alaska natives, persons with BMI ≥40 and individuals with certain chronic medical conditions (eg, pulmonary, cardiovascular, renal, hepatic, hematologic, metabolic, neurologic, HIV, malignancy) or those receiving immunosuppressive medications (CDC 2018b).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Influenza, treatment: Note: Treatment should ideally begin within 48 hours of illness onset; however, initiation after 48 hours is recommended for patients with severe, complicated, or progressive illness; hospitalized patients; or those at increased risk for complications (see Use for additional information). Initiate as early as possible in any hospitalized patient with suspected/confirmed influenza (CDC 2019).
The usual duration of therapy is 5 days; a longer duration may be necessary in severely ill or immunocompromised patients (CDC 2019).
Infants ≤8 months: Oral: 3 mg/kg/dose twice daily (AAP 2019; CDC 2019; IDSA [Uyeki 2019]; IDSA/PIDS [Bradley 2011]).
Infants ≥9 months: Oral: 3.5 mg/kg/dose twice daily (AAP 2019; IDSA [Uyeki 2019]); some experts still recommend 3 mg/kg/dose twice daily (CDC 2019; IDSA [Uyeki 2019]).
Children and Adolescents:
≤15 kg: Oral: 30 mg twice daily.
>15 to 23 kg: Oral: 45 mg twice daily.
>23 to 40 kg: Oral: 60 mg twice daily.
>40 kg: Oral: 75 mg twice daily.
Influenza, prophylaxis: Note: Recommendations for patient selection for prophylaxis are variable (see Use and/or guidelines for details). Duration of prophylaxis dependent upon type of exposure or outbreak (eg, household exposure vs hospital outbreak); see guidelines for details.
Infants 3 to 8 months: Limited data available: Oral: 3 mg/kg/dose once daily (AAP 2019; CDC 2019; IDSA [Uyeki 2019]).
Infants ≥9 months: Limited data available: Oral: 3.5 mg/kg/dose once daily (AAP 2019; IDSA [Uyeki 2019]); some experts still recommend 3 mg/kg/dose once daily (CDC 2019; IDSA [Uyeki 2019]).
Children and Adolescents:
≤15 kg: Oral: 30 mg once daily.
>15 kg to 23 kg: Oral: 45 mg once daily.
>23 kg to 40 kg: Oral: 60 mg once daily.
>40 kg: Oral: 75 mg once daily.
Dosing: Obesity
In adult morbidly obese patients (BMI >40 kg/m2), systemic exposure of oseltamivir carboxylate was not reduced; therefore, no dosage adjustment is necessary (Thorne-Humphrey 2011).
Reconstitution
Oral suspension: Reconstitute with 55 mL of water to a final concentration of 6 mg/mL (to make 60 mL total suspension).
Extemporaneously Prepared
Note: An oseltamivir oral suspension (6 mg/mL) is commercially available.
6 mg/mL Oral Suspension
If the commercially prepared oral suspension is not available, the manufacturer provides the following compounding information to prepare a 6 mg/mL suspension in emergency situations.
1. Place the specified amount of water into a polyethyleneterephthalate (PET) or glass bottle.
2. Carefully separate the capsule body and cap and pour the contents of the required number of 75 mg capsules into the PET or glass bottle.
3. Gently swirl the suspension to ensure adequate wetting of the powder for at least 2 minutes.
4. Slowly add the specified amount of vehicle to the bottle.
5. Close the bottle using a child-resistant cap and shake well for 30 seconds to completely dissolve the active drug.
6. Label “Shake Well Before Use.”
Stable for 35 days at 2°C to 8°C (36°F to 46°F) or 5 days at 25° C (77°F). Alternate recommendations suggest that preparations made with water containing preservative (ie, 0.05% sodium benzoate) are stable for 49 days at 2°C to 8°C (36°F to 46°F) and 10 days at 25°C (77°F) (Tamiflu Canadian product labeling 2017). Shake gently prior to use. Do not dispense with dosing device provided with commercially-available product.
|
Body Weight |
Total Volume per Patient1 |
# of 75 mg Capsules2 |
Required Volume of Water |
Required Volume of Vehicle2,3 |
Treatment Dose (wt based)4 |
Prophylactic Dose (wt based)4 |
|---|---|---|---|---|---|---|
|
1Entire course of therapy. |
||||||
|
2Based on total volume per patient. |
||||||
|
3Acceptable vehicles are cherry syrup (Humco®), Ora-Sweet® SF, or simple syrup. |
||||||
|
4Using 6 mg/mL suspension. |
||||||
|
≤15 kg |
75 mL |
6 |
5 mL |
69 mL |
5 mL (30 mg) twice daily for 5 days |
5 mL (30 mg) once daily for 10 days |
|
16 to 23 kg |
100 mL |
8 |
7 mL |
91 mL |
7.5 mL (45 mg) twice daily for 5 days |
7.5 mL (45 mg) once daily for 10 days |
|
24 to 40 kg |
125 mL |
10 |
8 mL |
115 mL |
10 mL (60 mg) twice daily for 5 days |
10 mL (60 mg) once daily for 10 days |
|
≥41 kg |
150 mL |
12 |
10 mL |
137 mL |
12.5 mL (75 mg) twice daily for 5 days |
12.5 mL (75 mg) once daily for 10 days |
Table has been converted to the following text.
Preparation of Oseltamivir 6 mg/mL Suspension
Weight-based details:
≤15 kg: To make a 6 mg/mL suspension, open six 75 mg capsules. Mix with 5 mL water and 69 mL vehicle to provide a total of 75 mL. Treatment dose is 5 mL (30 mg) twice daily for 5 days. Prophylactic dose is 5 mL (30 mg) once daily for 10 days.
16 to 23 kg: To make a 6 mg/mL suspension, open eight 75 mg capsules. Mix with 7 mL water and 91 mL vehicle to provide a total of 100 mL. Treatment dose is 7.5 mL (45 mg) twice daily for 5 days. Prophylactic dose is 7.5 mL (45 mg) once daily for 10 days.
24 to 40 kg: To make a 6 mg/mL suspension, open ten 75 mg capsules. Mix with 8 mL water and 115 mL vehicle to provide a total of 125 mL. Treatment dose is 10 mL (60 mg) twice daily for 5 days. Prophylactic dose is 10 mL (60 mg) once daily for 10 days.
≥41 kg: To make a 6 mg/mL suspension, open twelve 75 mg capsules. Mix with 10 mL water and 137 mL vehicle to provide a total of 150 mL. Treatment dose is 12.5 mL (75 mg) twice daily for 5 days. Prophylactic dose is 12.5 mL (75 mg) once daily for 10 days.
Alternate recommendations (Tamiflu Canadian product labeling 2017):
|
Body Weight |
Total Volume per Patient1 |
# of 75 mg Capsules2 |
Required Volume of Water (with preservative) |
Treatment Dose (wt based)2,3 |
Prophylactic Dose (wt based)2,3 |
|---|---|---|---|---|---|
|
1Entire course of therapy. |
|||||
|
2Using 6 mg/mL suspension. |
|||||
|
3Measured dose should be mixed with an equal amount of sweetened liquid (eg, chocolate syrup, cherry syrup) to mask bitter taste. |
|||||
|
≤15 kg |
75 mL |
6 |
74 mL |
5 mL (30 mg) twice daily for 5 days |
5 mL (30 mg) once daily for 10 days |
|
16 to 23 kg |
100 mL |
8 |
98 mL |
7.5 mL (45 mg) twice daily for 5 days |
7.5 mL (45 mg) once daily for 10 days |
|
24 to 40 kg |
125 mL |
10 |
123 mL |
10 mL (60 mg) twice daily for 5 days |
10 mL (60 mg) once daily for 10 days |
|
≥41 kg |
150 mL |
12 |
147 mL |
12.5 mL (75 mg) twice daily for 5 days |
12.5 mL (75 mg) once daily for 10 days |
Table has been converted to the following text.
Preparation of Oseltamivir 6 mg/mL Suspension
(using water with preservative [ie, 0.05% sodium benzoate]) (Tamiflu Canadian product labeling 2017)
Weight-based details:
≤15 kg: To make a 6 mg/mL suspension, open six 75 mg capsules. Mix with 74 mL water with preservative to provide a total of 75 mL. Treatment dose is 5 mL (30 mg) twice daily for 5 days. Prophylactic dose is 5 mL (30 mg) once daily for 10 days.
16 to 23 kg: To make a 6 mg/mL suspension, open eight 75 mg capsules. Mix with 98 mL water with preservative to provide a total of 100 mL. Treatment dose is 7.5 mL (45 mg) twice daily for 5 days. Prophylactic dose is 7.5 mL (45 mg) once daily for 10 days.
24 to 40 kg: To make a 6 mg/mL suspension, open ten 75 mg capsules. Mix with 123 mL water with preservative to provide a total of 125 mL. Treatment dose is 10 mL (60 mg) twice daily for 5 days. Prophylactic dose is 10 mL (60 mg) once daily for 10 days.
≥41 kg: To make a 6 mg/mL suspension, open twelve 75 mg capsules. Mix with 147 mL water with preservative to provide a total of 150 mL. Treatment dose is 12.5 mL (75 mg) twice daily for 5 days. Prophylactic dose is 12.5 mL (75 mg) once daily for 10 days.
Administration
May be administered without regard to meals; take with food to improve tolerance.
Capsules may be opened and mixed with sweetened liquid (eg, chocolate syrup, corn syrup, caramel topping, light brown sugar dissolved in water). Administer oral suspension using an oral dosing dispenser that measures the appropriate volume in milliliters; shake well before each use. When oral suspension is not available and/or age-appropriate strength of capsules are not available to mix with sweetened liquids, an extemporaneous preparation may be prepared (refer to “extemporaneously prepared” section of monograph for further details).
Mechanically ventilated critically ill patients: May administer via naso- or orogastric (NG/OG) tube. Dissolve powder from capsules in 20 mL of sterile water and inject down the NG/OG tube; follow with a 10 mL sterile water flush (Taylor 2008).
Dietary Considerations
Take without regard to meals; take with food to improve tolerance.
Storage
Capsules: Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Oral suspension: Store powder for suspension at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Once reconstituted, store oral suspension under refrigeration at 2°C to 8°C (36°F to 46°F) or at room temperature; do not freeze. Use within 10 days of preparation if stored at room temperature or within 17 days of preparation if stored under refrigeration.
Oseltamivir Images
Drug Interactions
Dichlorphenamide: May increase the serum concentration of Oseltamivir. Avoid combination
Influenza Virus Vaccine (Live/Attenuated): Antiviral Agents (Influenza A and B) may diminish the therapeutic effect of Influenza Virus Vaccine (Live/Attenuated). Management: Avoid anti-influenza antivirals during the period beginning 48 hours prior to and ending 2 weeks after live influenza virus vaccine administration. Consider therapy modification
Probenecid: May increase serum concentrations of the active metabolite(s) of Oseltamivir. Management: Consider a change in therapy when using oseltamivir together with probenecid; reduced oseltamivir dose may be necessary. Increase monitoring for adverse events, such as thrombocytopenia. Consider therapy modification
Adverse Reactions
>10%:
Central nervous system: Headache (adolescents and adults: 2% to 17%)
Gastrointestinal: Vomiting (2% to 16%)
1% to 10%:
Central nervous system: Pain (adolescents and adults: 4%)
Gastrointestinal: Nausea (adolescents and adults: 8% to 10%)
<1%, postmarketing, and/or case reports: Abnormal behavior, abnormal hepatic function tests, accidental injury, agitation, anaphylactoid reaction, anaphylaxis, anxiety, cardiac arrhythmia, confusion, delirium, delusions, dermatitis, eczema, erythema multiforme, exacerbation of diabetes mellitus, facial edema, gastrointestinal hemorrhage, hallucination, hemorrhagic colitis, hepatitis, hypersensitivity reaction, hypothermia, impaired consciousness, nightmares, seizure, skin rash, Stevens-Johnson syndrome, swollen tongue, toxic epidermal necrolysis, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Anaphylaxis/hypersensitivity: Rare but severe hypersensitivity reactions, including anaphylaxis and severe dermatologic reactions (eg, toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema multiforme), have been associated with use. Discontinue use immediately if hypersensitivity occurs or is suspected and treat appropriately.
- Neuropsychiatric events: Rare occurrences of neuropsychiatric events (including confusion, delirium, hallucinations, and/or self-injury) have been reported primarily in pediatric patients from postmarketing surveillance; direct causation is difficult to establish (influenza infection may also be associated with behavioral and neurologic changes, in some cases resulting in fatal outcomes). These events may occur in the setting of encephalitis or encephalopathy but can occur without obvious severe disease. Monitor closely for signs of any unusual behavior.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with chronic cardiac disease.
- Hepatic impairment: Use with caution in patients with severe hepatic impairment; safety and efficacy have not been established.
- Renal impairment: Use with caution; dosage adjustment is required for patients with renal impairment. Not recommended for patients with end stage renal disease (ESRD) not undergoing dialysis.
- Respiratory disease: Use with caution in patients with respiratory disease.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer's labeling.
- Sorbitol: Oral suspension contains sorbitol (delivers ~2 g sorbitol per 75 mg dose) which is greater than the maximum daily limit for patients with hereditary fructose intolerance; may cause diarrhea and dyspepsia; use with caution.
Other warnings/precautions:
- Appropriate use: Oseltamivir is not a substitute for the influenza virus vaccine. It has not been shown to prevent primary or concomitant bacterial infections that may occur with influenza virus. Antiviral treatment should begin within 48 hours of symptom onset. However, the CDC recommends that treatment may still be beneficial and should be started in hospitalized patients with severe, complicated or progressive illness if >48 hours. Treatment should not be delayed while awaiting results of laboratory tests for influenza. Nonhospitalized persons who are not at high risk for developing severe or complicated illness and who have a mild disease are not likely to benefit if treatment is started >48 hours after symptom onset. Nonhospitalized persons who are already beginning to recover do not need treatment.
Monitoring Parameters
Signs or symptoms of unusual behavior, including attempts at self-injury, confusion, and/or delirium
Critically-ill patients: Repeat rRT-PCR or viral culture may help to determine on-going viral replication
Pregnancy
Pregnancy Considerations
Oseltamivir phosphate and its active metabolite oseltamivir carboxylate cross the placenta (Meijer 2012).
An increased risk of adverse neonatal or maternal outcomes has generally not been observed following maternal use of oseltamivir during pregnancy (CDC 2011).
Untreated influenza infection is associated with an increased risk of adverse events to the fetus and an increased risk of complications or death to the mother. Oseltamivir is currently recommended for the treatment or prophylaxis of influenza in pregnant women and women up to 2 weeks' postpartum (ACOG 2018; CDC 2011).
Patient Education
What is this drug used for?
- It is used to treat or prevent the flu.
Frequently reported side effects of this drug
- Diarrhea
- Nausea
- Vomiting
- Headache
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Confusion
- Behavioral changes
- Difficulty speaking
- Tremors
- Seizures
- Sensing things that seem real but are not
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.