Boxed Warning
Peliosis hepatis:
Peliosis hepatis, a condition in which liver and, sometimes, splenic tissue is replaced with blood-filled cysts, has occurred in patients receiving androgenic anabolic steroids. These cysts are sometimes present with minimal hepatic dysfunction and have been associated with liver failure. Often, they are not recognized until life-threatening liver failure or intra-abdominal hemorrhage develops. Withdrawal of drug usually results in complete disappearance of lesions.
Liver cell tumors:
Most often these tumors are benign and androgen-dependent, but fatal malignant tumors have occurred. Withdrawal of drug often results in regression or cessation of tumor progression. However, hepatic tumors associated with androgens or anabolic steroids are much more vascular than other hepatic tumors and may be silent until life-threatening, intra-abdominal hemorrhage develops.
Blood lipid changes:
Blood lipid changes associated with increased risk of atherosclerosis are seen in patients treated with androgens and anabolic steroids. These changes include decreased high-density lipoprotein (HDL) and, sometimes, increased low-density lipoprotein (LDL). The changes may be very marked and could have a serious impact on the risk of atherosclerosis and coronary artery disease.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Tablet, Oral:
Oxandrin: 2.5 mg [DSC] [scored]
Oxandrin: 10 mg [DSC]
Generic: 2.5 mg, 10 mg
Pharmacology
Mechanism of Action
Synthetic testosterone derivative with similar androgenic and anabolic actions
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Well absorbed (Orr 2004)
Excretion
Urine (28% as unchanged drug) (Orr 2004)
Time to Peak
Concentration: ~1 hour (Orr 2004)
Half-Life Elimination
10 to 13 hours
Protein Binding
95% (Orr 2004)
Use: Labeled Indications
Weight gain (adjunctive therapy): Adjunctive therapy to promote weight gain after weight loss following extensive surgery, chronic infections, or severe trauma, and in some patients who, without definite pathophysiologic reasons, fail to gain or to maintain normal weight
Other indications included in manufacturer labeling: Adjunctive therapy to offset protein catabolism with prolonged corticosteroid administration; relief of bone pain associated with osteoporosis (current guidelines do not make recommendations regarding use of oxandrolone for osteoporosis related bone pain)
Use: Off Label
Burns, severe (adjunctive therapy)b
Data from a systematic review and meta-analysis support the use of oxandrolone as adjunctive therapy in the treatment of adult and geriatric patients with severe burns. Length of stay, donor-site healing time, time between surgical procedures, and decreased weight loss were improved in the catabolic phase. In the rehabilitative stage, length of stay and lean body mass were improved; lean body mass improvements continued into the long-term phase (after 12 months) of burn recovery Li 2016.
Contraindications
Nephrosis; breast cancer in females with hypercalcemia; known or suspected prostate or breast cancer in males; hypercalcemia; pregnancy
Dosage and Administration
Dosing: Adult
Burns, severe (off-label): Oral, Enteral feeding tube: 10 mg every 12 hours beginning ~5 days after injury (Li 2016; Wolf 2006)
Weight gain (adjunctive therapy): Oral: 2.5 to 20 mg in divided doses 2 to 4 times daily based on individual response; a course of therapy of 2 to 4 weeks is usually adequate. May repeat intermittently as needed.
Dosing: Geriatric
Burns, severe (adjunctive therapy) (off-label): Oral: 10 mg every 12 hours (Demling 2003; Li 2016) or 10 mg/day in patients with renal impairment (ie, CrCl <25% of normal for age) (Demling 2003)
Weight gain (adjunctive therapy): Oral: 5 mg twice daily
Dosing: Pediatric
Burn management, severe; to increase lean muscle mass and promote wound healing: Limited data available: Children and Adolescents: Oral: 0.1 mg/kg/dose twice daily for up to 12 months has been shown to increase lean body mass, bone mineral density, and muscle strength; shortened length of ICU stay and improved donor site wound healing were also observed (Hart 2001; Jeschke 2007; Murphy 2004; Porro 2012; Przkora 2005). Benefits have been shown to persist for up to 5 years post burn (Porro 2012; Przkora 2005).
Constitutional delay of growth and puberty (CDGP) (males): Limited data available: Children and Adolescents 9 to 16 years: Oral: 1.25 to 2.5 mg once daily in the evening; usual duration: 3 to 12 months although longer (~5 years) has been reported (Albanese 1994; Buyukgebiz 1990; Papadimitriou 1991; Schroor 1995; Stanhope 1985; Stanhope 1988; Tse 1990)
Turner Syndrome (females): Limited data available: Children and Adolescents ≥8 years: Oral: Reported range: 0.03 to 0.06 mg/kg/day at bedtime in combination with growth hormone and/or estrogen; maximum single dose: 2.5 mg/dose; due to risks of dose-related virilization, doses ≥0.05 mg/kg/day should generally be avoided. Typically, therapy initiated at 8 to 9 years of age and continued until goal height attained or further growth is unlikely (eg, bone age ≥14 years and growth velocity <2 cm/year) (Bareille 1997; NIH [Bondy 2007]; Freriks 2012; Gault 2011; Haeusler 1995; Menke 2010; Nilsson 1996).
Weight gain, adjunct: Children and Adolescents: Oral: Total daily dose: ≤0.1 mg/kg; may be repeated intermittently as needed; in adult patients, the daily dose is divided 2 to 4 times daily; typical duration of therapy: 2 to 4 weeks
Extemporaneously Prepared
A 1 mg/mL oral suspension may be made with tablets and either a 1:1 mixture of Ora-Sweet® and Ora-Plus®, or a 1:1 mixture of Ora-Sweet® SF and Ora-Plus®. Crush twenty-four 2.5 mg tablets in a mortar to a fine powder. Add small portions of chosen vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 60 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 60 mL. Thoroughly mix the suspension by shaking. Label “shake well” and “protect from light”. Stable for 90 days at room temperature (Johnson, 2011).
Johnson CE, Cober MP, Hawkins KA, et al, “Stability of Extemporaneously Prepared Oxandrolone Oral Suspensions,” Am J Health-Syst Pharm, 2011, 68(6):519-21.21378300
Administration
Enteral feeding tube (off-label): In severe burn patients unable to tolerate oral administration, may dissolve oxandrolone tablets in ethanol and administer through enteral feeding tube (Wolf 2006).
Storage
Store at 20°C to 25°C (68°F to 77°F).
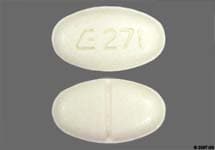
Oxandrolone Images
Drug Interactions
Ajmaline: Androgens may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Blood Glucose Lowering Agents: Androgens may enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
C1 inhibitors: Androgens may enhance the thrombogenic effect of C1 inhibitors. Monitor therapy
Corticosteroids (Systemic): May enhance the fluid-retaining effect of Androgens. Monitor therapy
CycloSPORINE (Systemic): Androgens may enhance the hepatotoxic effect of CycloSPORINE (Systemic). Androgens may increase the serum concentration of CycloSPORINE (Systemic). Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Androgens may enhance the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Test Interactions
May suppress factors II, V, VII, and X; may increase PT; may decrease thyroxine-binding globulin and radioactive iodine uptake
Adverse Reactions
Frequency not defined.
Cardiovascular: Edema
Central nervous system: Deepening of the voice (females), depression, excitement, habituation, insomnia
Dermatologic: Acne vulgaris (females and prepubertal males), androgenetic alopecia (females)
Endocrine & metabolic: Changes in libido, decreased glucose tolerance, decreased HDL cholesterol, electrolyte disturbance, gynecomastia, hirsutism (females), increased LDL cholesterol, inhibition of gonadotropin secretion, menstrual disease (females)
Genitourinary: Clitoromegaly (females), epididymitis (postpubertal males), erectile dysfunction (prepubertal males; increased or persistent erections), impotence (postpubertal males), inhibition of testicular function (postpubertal males), irritable bladder (postpubertal males), oligospermia (postpubertal males), phallic enlargement (prepubertal males), priapism (chronic; postpubertal males), testicular atrophy (postpubertal males)
Hematologic & oncologic: Clotting factors suppression, prolonged prothrombin time
Hepatic: Cholestatic jaundice, hepatocellular neoplasm, increased serum alkaline phosphatase, increased serum ALT, increased serum AST, increased serum bilirubin, peliosis hepatitis (long-term therapy)
Neuromuscular & skeletal: Increased creatine phosphokinase, premature epiphyseal closure (children)
Renal: Increased creatinine clearance
<1%, postmarketing, and/or case reports: Hepatic necrosis, hepatotoxicity (idiosyncratic; Chalasani 2014)
Warnings/Precautions
Concerns related to adverse effects:
- Blood lipid changes: [US Boxed Warning]: May cause blood lipid changes with increased risk of arteriosclerosis. Use caution in patients at risk for, or with a history of cardiovascular disease; monitor lipid profile and adjust therapy as indicated. Lipid changes are usually reversible upon discontinuation of therapy.
- Gynecomastia: May cause gynecomastia.
- Hepatic effects: [US Boxed Warning]: Anabolic steroids may cause peliosis hepatis or liver cell tumors which may not be apparent until liver failure or intra-abdominal hemorrhage develops. Discontinue in case of cholestatic hepatitis with jaundice or abnormal liver function tests; drug-induced jaundice is reversible upon discontinuation. Use with caution in patients with hepatic impairment.
- Oligospermia: May suppress spermatogenesis; oligospermia may occur.
- Polycythemia: Increased hemoglobin and hematocrit may occur with high doses of anabolic steroids; monitor.
- Priapism: Priapism or excessive sexual stimulation may occur.
Disease-related concerns:
- Breast cancer: Use with caution in females with breast cancer; may cause hypercalcemia by stimulating osteolysis; use is contraindicated in females with breast cancer and hypercalcemia. Discontinue use if hypercalcemia occurs. Use is contraindicated in males with known or suspected breast cancer.
- Carbohydrate intolerance: May have adverse effects on glucose tolerance; use caution in patients with diabetes.
- COPD: Use with caution in patients with COPD.
- Edematous conditions: Use with caution in patients with conditions influenced by edema (eg, cardiovascular disease, migraine, seizure disorder, hepatic impairment, renal impairment); may cause fluid retention.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution in elderly patients, elderly males may be at greater risk for prostatic hyperplasia and prostate cancer.
- Pediatric: May accelerate bone maturation without producing compensatory gain in linear growth in children; effect may continue for 6 months after the drug is stopped; in prepubertal children perform radiographic examination of the left hand and wrist every 6 months to determine the rate of bone maturation and to assess the effect of treatment on the epiphyseal centers.
- Females: May cause mild virilization in females; monitor for signs of virilization (deepening of the voice, hirsutism, acne, clitoromegaly). Discontinue with evidence of mild virilization in female patients; early discontinuation may prevent irreversible virilization.
Monitoring Parameters
Liver function tests, cholesterol profile, hemoglobin/hematocrit; INR/PT in patients on anticoagulant therapy
Children: Radiographs of left wrist and hand every 6 months (to assess bone maturation)
Adult females: Signs of virilization (deepening voice, hirsutism, acne, clitoromegaly); urine and serum calcium in women with breast cancer
Pregnancy
Pregnancy Risk Factor
X
Pregnancy Considerations
Use is contraindicated in pregnant women; masculinization of the fetus has been reported.
Patient Education
What is this drug used for?
- It is used to help you gain weight.
- It is used to ease bone pain.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Skin discoloration
- Trouble sleeping
- Decreased sex drive
- Sexual dysfunction
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- High calcium like weakness, confusion, fatigue, headache, nausea and vomiting, constipation, or bone pain.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Erection that lasts more than 4 hours
- Acne
- Severe anxiety
- Bruising
- Bleeding
- Testicular changes
- Virilization like in females a deep voice, facial hair, acne, or menstrual changes.
- Enlarged breasts
- Bladder irritation
- Depression
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.