Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution Reconstituted, Oral:
Generic: 125 mg/5 mL (100 mL, 200 mL); 250 mg/5 mL (100 mL, 200 mL)
Tablet, Oral:
Generic: 250 mg, 500 mg
Pharmacology
Mechanism of Action
Inhibits bacterial cell wall synthesis by binding to one or more of the penicillin-binding proteins (PBPs); which in turn inhibits the final transpeptidation step of peptidoglycan synthesis in bacterial cell walls, thus inhibiting cell wall biosynthesis. Bacteria eventually lyse due to ongoing activity of cell wall autolytic enzymes (autolysins and murein hydrolases) while cell wall assembly is arrested.
Pharmacokinetics/Pharmacodynamics
Excretion
Urine (as unchanged drug and metabolites)
Protein Binding
Plasma: 80%
Use in Specific Populations
Special Populations: Renal Function Impairment
Excretion is considerably delayed.
Special Populations: Children
In neonates and young infants, excretion is considerably delayed.
Use: Labeled Indications
Fusospirochetosis (Vincent gingivitis and pharyngitis): Treatment of fusospirochetosis (Vincent gingivitis and pharyngitis), in conjunction with dental care for infections involving gum tissue.
Pneumococcal infections: Treatment of mild to moderately severe pneumococcal respiratory tract infections, including otitis media.
Rheumatic fever and/or chorea prophylaxis: Prophylaxis (chronic, secondary) of rheumatic fever and/or chorea.
Staphylococcal infections (penicillin G-sensitive): Treatment of mild infections of the skin and soft tissues.
Streptococcal infections (without bacteremia): Treatment of mild to moderate streptococcal infections of the upper respiratory tract, scarlet fever, and mild erysipelas.
Use: Off Label
Actinomycosisc
Data from a limited number of clinical studies suggest that penicillin V potassium may be beneficial for the treatment of actinomycosis after initial surgical intervention and IV therapy with penicillin G (if clinically indicated) Hsieh 1993, Sudhakar 2004. Clinical experience also suggests the utility of penicillin V potassium in the treatment of actinomycosis Smego 1998. Duration is dependent upon disease location and patient-specific factors. Additional data may be necessary to further define the role of penicillin V potassium in this condition.
Bite wounds (animal)yes
Based on the Infectious Diseases Society of America (IDSA) guidelines for the diagnosis and management of skin and soft tissue infections (SSTI), penicillin V potassium, in combination with dicloxacillin, is an effective and recommended option for treatment of animal bites.
Chronic antimicrobial suppression of prosthetic joint infectionyes
Based on the Infectious Diseases Society of America (IDSA) Diagnosis and Management of Prosthetic Joint Infection: Clinical Practice Guideline, penicillin V potassium given for chronic antimicrobial suppression of prosthetic joint infection is effective and recommended in the management of this condition.
Cutaneous anthraxyes
Based on the Infectious Diseases Society of America (IDSA) Practice Guidelines for the Diagnosis and Management of Skin and Soft Tissue Infections (SSTI), penicillin V potassium given for cutaneous anthrax (community acquired) is effective and recommended in the management of this condition.
Cutaneous erysipeloidyes
Based on the Infectious Diseases Society of America (IDSA) Practice Guidelines for the Diagnosis and Management of Skin and Soft Tissue Infections (SSTI), penicillin V potassium given for cutaneous erysipeloid is effective and recommended in the management of this condition.
Pneumococcal prophylaxis in hematopoietic cell transplantyes
Based on the Guidelines for Preventing Infectious Complications among Hematopoietic Cell Transplant (HCT) Recipients, penicillin v potassium may be used in HCT recipients with chronic graft-versus host disease (GVHD) or low IgG levels to prevent invasive pneumococcal infection, in areas where the incidence of penicillin-resistant S. pneumoniae is not high Tomblyn 2009.
Streptococcus (group A) chronic carrieryes
Based on the Infectious Diseases Society of America (IDSA) Clinical Practice Guideline for the Diagnosis and Management of Group A Streptococcal Pharyngitis, penicillin V potassium given to chronic carriers of group A streptococcal is effective and recommended in the management of this condition.
Contraindications
Hypersensitivity to penicillin or any component of the formulation
Dosage and Administration
Dosing: Adult
Usual dosage range: Oral: 125 to 500 mg every 6 to 8 hours
Actinomycosis (off-label use): Oral: Note: Duration is dependent upon disease location and patient-specific factors; complicated infections requiring surgical intervention usually initiate IV therapy with penicillin G until disease subsidence followed by long term oral therapy (Hsieh 1993; Sudhakar 2004):
2 to 4 g/day in divided doses every 6 hours (Smego 1998)
Bite wounds (animal) (off-label use): Oral: 500 mg 4 times daily in combination with dicloxacillin (IDSA [Stevens 2014])
Cutaneous anthrax, community-acquired (off-label use): Oral: 500 mg 4 times daily for 7 to 10 days (IDSA [Stevens 2014])
Cutaneous erysipeloid (off-label use): Oral: 500 mg 4 times daily for 7 to 10 days (IDSA [Stevens 2014])
Erysipelas: Oral:
500 mg 4 times daily (IDSA [Stevens 2014])
Manufacturer's labeling: Dosing in the prescribing information may not reflect current clinical practice. 125 to 250 mg every 6 to 8 hours.
Fusospirochetosis (Vincent infection): Oral: 250 to 500 mg every 6 to 8 hours
Pneumococcal prophylaxis in hematopoietic cell transplant (off-label use): Oral: 250 to 500 mg twice daily. Note: Use only in areas where incidence of penicillin-resistant S. pneumoniae is low (Tomblyn 2009).
Prosthetic joint infection (off-label use): Chronic oral antimicrobial suppression (Enterococcus spp [penicillin-susceptible], streptococci [beta-hemolytic], Cutibacterium spp): Oral: 500 mg 2 to 4 times daily (Osmon 2013)
Streptococcal skin infection (off-label dose): Oral: 250 to 500 mg every 6 hours (IDSA [Stevens 2014])
Streptococcus (group A): Oral:
Pharyngitis, acute treatment: 500 mg 2 to 3 times daily for 10 days (AHA [Gerber 2009]); or 250 mg 4 times daily or 500 mg twice daily for 10 days (IDSA [Shulman 2012])
Secondary prophylaxis for rheumatic fever (prevention of recurrent attacks) (alternative agent): 250 mg twice daily. Duration depends on risk factors and presence of valvular disease (AHA [Gerber 2009]).
Chronic carriage (off-label use): 500 mg 4 times daily for 10 days in combination with oral rifampin. Note: Most individuals with chronic carriage do not require antibiotics (IDSA [Shulman 2012])
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
General dosing, susceptible infections: Oral:
Infants and Children <12 years: Mild to moderate infection: 25 to 75 mg/kg/day in divided doses every 6 to 8 hours; maximum daily dose: 2,000 mg/day (Red Book [AAP 2015])
Children ≥12 years and Adolescents:
Manufacturer's labeling (fixed dosing): 125 to 500 mg every 6 to 8 hours
Alternate dosing (weight-based): Mild to moderate infection: 25 to 75 mg/kg/day in divided doses every 6 to 8 hours; maximum daily dose: 2,000 mg/day (Red Book [AAP 2015])
Anthrax (cutaneous), community-acquired: Oral: Infants, Children, and Adolescents: 25 to 50 mg/kg/day in divided doses 2 or 4 times daily; maximum single dose: 500 mg (Stevens 2005)
Fusospirochetosis (Vincent infection), mild to moderately severe infections: Oral: Children ≥12 years and Adolescents: 250 to 500 mg every 6 to 8 hours
Tonsillopharyngitis; Group A streptococcal infection, treatment and primary prevention of rheumatic fever: Oral:
Acute treatment (Gerber 2009; Shulman 2012; WHO 2004):
Children ≤27 kg: 250 mg 2 to 3 times daily for 10 days
Children >27 kg and Adolescents: 500 mg 2 to 3 times daily for 10 days; in adolescents, 250 mg 4 times daily has also been suggested
Chronic carrier treatment (Group A streptococci): Children and Adolescents: 50 mg/kg/day in 4 divided doses for 10 days in combination with oral rifampin; maximum daily dose: 2,000 mg/day (Shulman 2012)
Recurrent rheumatic fever, prophylaxis: Children and Adolescents: 250 mg twice daily (Gerber 2009)
Pneumococcal infection prophylaxis for anatomic or functional asplenia [eg, sickle cell disease (SCD)] (AAP 2002; Kavanagh 2011; NHLBI 2014):
Infants (as soon as SCD diagnosed or asplenic) and Children <3 years: Oral: 125 mg twice daily
Children ≥3 years: Oral: 250 mg twice daily; the decision to discontinue penicillin prophylaxis after 5 years of age in children who have not experienced invasive pneumococcal infection and have received recommended pneumococcal immunizations is patient and clinician dependent
Pneumonia, community-acquired; Group A Streptococcus, mild infection or step-down therapy: Oral: Infants ≥3 months, Children, and Adolescents: 50 to 75 mg/kg/day in 3 to 4 divided doses (Bradley 2011); maximum daily dose: 2,000 mg/day
Reconstitution
Reconstitute powder for oral solution with appropriate amount of water as specified in the manufacturer’s labeling. Shake vigorously until dissolved.
Administration
Oral: Administer around-the-clock to promote less variation in peak and trough serum levels. Take on an empty stomach 1 hour before or 2 hours after meals, to enhance absorption.
Storage
Powder for oral solution: Store dry powder at 20°C to 25°C (68°F to 77°F). Reconstituted oral solution should be stored in refrigerator. Discard unused solution after 14 days (consult manufacturer labeling for specific recommendations).
Tablet: Store at 20°C to 25°C (68°F to 77°F).
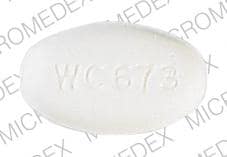
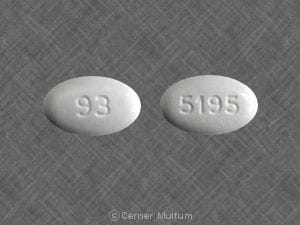
Penicillin V Potassium Images
Drug Interactions
Acemetacin: May increase the serum concentration of Penicillins. Monitor therapy
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Dichlorphenamide: Penicillins may enhance the hypokalemic effect of Dichlorphenamide. Monitor therapy
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Methotrexate: Penicillins may increase the serum concentration of Methotrexate. Monitor therapy
Mycophenolate: Penicillins may decrease serum concentrations of the active metabolite(s) of Mycophenolate. This effect appears to be the result of impaired enterohepatic recirculation. Monitor therapy
Nitisinone: May increase the serum concentration of OAT1/3 Substrates. Monitor therapy
Pretomanid: May increase the serum concentration of OAT1/3 Substrates. Monitor therapy
Probenecid: May increase the serum concentration of Penicillins. Monitor therapy
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Teriflunomide: May increase the serum concentration of OAT1/3 Substrates. Monitor therapy
Tetracyclines: May diminish the therapeutic effect of Penicillins. Monitor therapy
Tolvaptan: May increase the serum concentration of OAT1/3 Substrates. Management: Patients being treated with the Jynarque brand of tolvaptan should avoid concomitant use of OAT1/3 substrates. Concentrations and effects of the OAT1/3 substrate would be expected to increase with any combined use. Consider therapy modification
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Penicillins may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Test Interactions
False-positive or negative urinary glucose determination using Clinitest®; positive Coombs' [direct]; false-positive urinary and/or serum proteins
Adverse Reactions
>10%: Gastrointestinal: Melanoglossia, mild diarrhea, nausea, oral candidiasis, vomiting
<1%: Acute interstitial nephritis, anaphylaxis, convulsions, exfoliative dermatitis, fever, hemolytic anemia, hypersensitivity reaction, positive direct Coombs test, serum-sickness like reaction
Warnings/Precautions
Concerns related to adverse effects:
- Anaphylactic/hypersensitivity reactions: Serious and occasionally severe or fatal hypersensitivity (anaphylactic) reactions have been reported in patients on penicillin therapy, especially with a history of beta-lactam hypersensitivity or history of sensitivity to multiple allergens.). Use with caution in asthmatic patients. If a serious reaction occurs, treatment with supportive care measures and airway protection should be instituted immediately.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Renal impairment: Use with caution in patients with severe renal impairment.
- Seizure disorders: Use with caution in patients with a history of seizure disorder; high levels, particularly in the presence of renal impairment, may increase risk of seizures.
Concurrent drug therapy related issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC, 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
Other warnings/precautions:
- Prolonged use: Extended duration of therapy or use associated with high serum concentrations (eg, in renal insufficiency) may be associated with an increased risk for some adverse reactions (neutropenia, hemolytic anemia, serum sickness).
Monitoring Parameters
Periodic renal and hematologic function tests during prolonged therapy; monitor for signs of anaphylaxis during first dose
Pregnancy
Pregnancy Considerations
Penicillin crosses the placenta.
Maternal use of penicillins has generally not resulted in an increased risk of adverse fetal effects. Due to pregnancy-induced physiologic changes, some pharmacokinetic parameters of penicillin V may be altered in the second and third trimester (Heikkilä 1993). If treatment for the management of Bacillus anthracis is needed in pregnant women, other agents are preferred (Meaney-Delman 2014)
Patient Education
What is this drug used for?
- It is used to treat or prevent bacterial infections.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Abdominal pain
- Tongue discoloration
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Clostridioides (formerly Clostridium) difficile-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.