Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Intravenous [preservative free]:
Noxafil: 300 mg/16.7 mL (16.7 mL) [contains edetate disodium]
Suspension, Oral:
Noxafil: 40 mg/mL (105 mL) [contains polysorbate 80, sodium benzoate; cherry flavor]
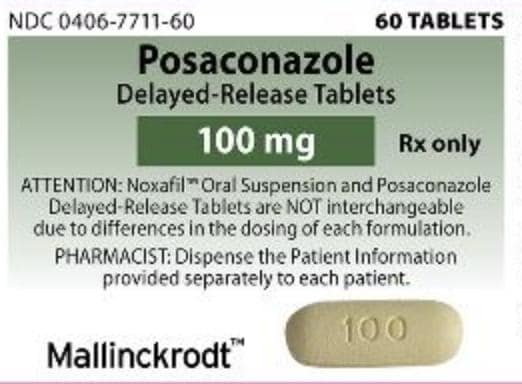
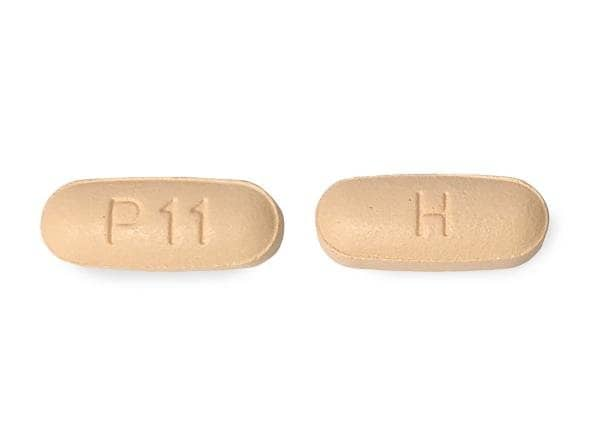
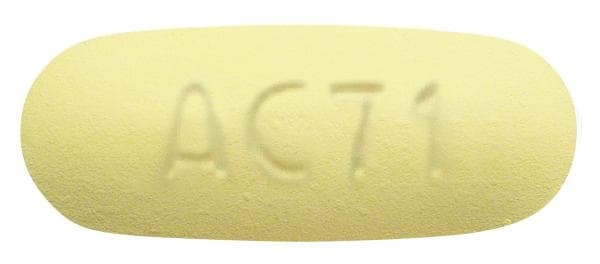
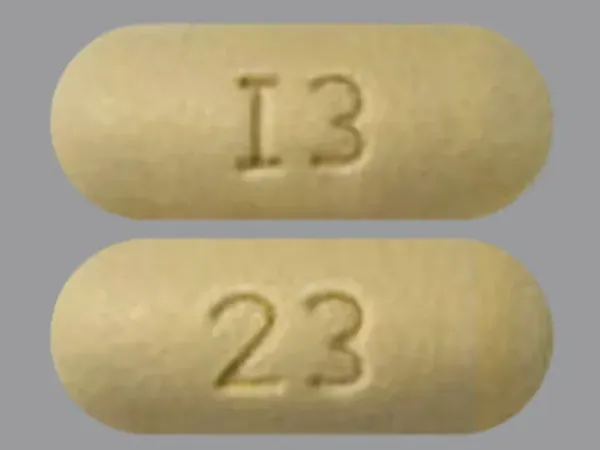
Tablet Delayed Release, Oral:
Noxafil: 100 mg
Generic: 100 mg
Pharmacology
Mechanism of Action
Interferes with fungal cytochrome P450 (lanosterol-14α-demethylase) activity, decreasing ergosterol synthesis (principal sterol in fungal cell membrane) and inhibiting fungal cell membrane formation.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral suspension: Unpredictable and variable (optimal absorption with a high-fat meal in 4 divided doses; absorption may be sufficient if taken with a nutritional supplement or acidic beverage [eg, ginger ale]).
Tablet (delayed-release): Predictable (preferably administered with food, but absorption is sufficient under fasting conditions).
Distribution
Vd: Oral: 287 L; Injection: ~261 L
Metabolism
Not significantly metabolized; 17% undergoes non-CYP-mediated metabolism, primarily via hepatic glucuronidation into metabolites
Excretion
Feces 71% (~66% of the total dose as unchanged drug); urine 13% (<0.2% of the total dose as unchanged drug)
Time to Peak
Plasma: Suspension: ~3 to 5 hours; Tablets: ~4 to 5 hours
Half-Life Elimination
Suspension: 35 hours (range: 20 to 66 hours); Tablets: 26 to 31 hours; Injection: ~27 hours
Protein Binding
>98%; predominantly bound to albumin
Use: Labeled Indications
Candidiasis, oropharyngeal: Suspension (≥13 years of age): Treatment of oropharyngeal candidiasis (including patients refractory to itraconazole and/or fluconazole)
Invasive fungal infections, prophylaxis: Suspension and delayed-release tablets (≥13 years of age) and injection (≥18 years of age): Prophylaxis of invasive Aspergillus and Candida infections in patients who are at high risk of developing these infections due to being severely immunocompromised (eg, hematopoietic stem cell transplant [HSCT] recipients with graft-versus-host disease [GVHD] or those with prolonged neutropenia secondary to chemotherapy for hematologic malignancies).
Use: Off Label
Aspergillosis, invasive treatment (refractory to or intolerant of conventional therapy)yes
Based on the Infectious Diseases Society of America (IDSA) practice guidelines for the diagnosis and management of aspergillosis, posaconazole is an effective and recommended therapeutic option for salvage therapy (alone or in combination with another antifungal) in the treatment of invasive aspergillosis.
Candidiasis, esophageal (refractory to conventional therapy)yes
Based on the Infectious Diseases Society of America (IDSA) clinical practice guidelines for the management of candidiasis and the US Department of Health and Human Services (HHS) guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents, posaconazole may be considered as an alternative for patients with esophageal candidiasis refractory to conventional therapy.
Coccidioidomycosis, treatment (refractory to conventional therapy)yes
Based on the IDSA clinical practice guideline for the treatment of coccidioidomycosis and the US Department of Health and Human Services (HHS) guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents, posaconazole is an effective and recommended alternative agent in the treatment of coccidioidomycosis in patients who are refractory to conventional therapy.
Cryptococcal infections (pulmonary, nonimmunosuppressed)yes
Based on the IDSA clinical practice guidelines for the management of cryptococcal disease, posaconazole is effective and recommended as an acceptable alternative for pulmonary cryptococcosis in nonimmunosuppressed patients if fluconazole is unavailable or contraindicated.
Mucormycosiscyes
Data from a limited number of patients suggest that posaconazole may be beneficial as salvage therapy for mucormycosis Greenberg 2006, van Burik 2006.
Based on the European Conference on Infections in Leukemia (ECIL) guidelines for the treatment of candidiasis, aspergillosis, and mucormycosis in leukemia and hematopoietic stem cell transplant patients and the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and European Confederation of Medical Mycology (ECMM) joint clinical guidelines for the diagnosis and management of mucormycosis, posaconazole, with or without a lipid formulation of amphotericin B, may be beneficial as salvage therapy for mucormycosis.
Contraindications
Coadministration with sirolimus, ergot alkaloids (eg, ergotamine, dihydroergotamine), HMG-CoA reductase inhibitors that are primarily metabolized through CYP3A4 (eg, atorvastatin, lovastatin, simvastatin), or CYP3A4 substrates that prolong the QT interval (eg, pimozide, quinidine); hypersensitivity to posaconazole, other azole antifungal agents, or any component of the formulation.
Dosage and Administration
Dosing: Adult
Note: The delayed-release tablet and oral suspension are not to be used interchangeably due to dosing differences for each formulation. Since the delayed-release tablet is easier to administer, better tolerated, and more reliably absorbed, the use of delayed-release tablets is preferred. The bioavailability of a once daily 300 mg dose given as the delayed-release tablet appears to be similar or greater than the bioavailability of 200 mg given 3 to 4 times daily, based upon available pharmacokinetic studies (Cumpston 2015; Durani 2015). The IV formulation is given at the same dose as the delayed-release tablet.
Aspergillosis, invasive:
Prophylaxis (immunocompromised host):
Oral:
Suspension: 200 mg 3 times daily; duration of therapy is based on recovery from neutropenia or immunosuppression. In patients with acute myelogenous leukemia (AML) or myelodysplastic syndromes (MDS), posaconazole was initiated at the time of chemotherapy initiation (or if receiving anthracyclines, 24 hours after the last anthracycline dose) and was continued until recovery from neutropenia, until complete remission, or for up to 12 weeks, whichever occurred first (Cornely 2007). In patients with graft-versus-host disease (GVHD) receiving immunosuppressive therapy, posaconazole was continued for 112 days (Ullmann 2007), although the optimal duration in GVHD has not been fully defined (Tomblyn 2009). It is recommended to continue throughout the duration of immunosuppression (ie, corticosteroid equivalent of >1 mg/kg/day of prednisone for >2 weeks and/or the use of other anti-GVHD therapies) (IDSA [Patterson 2016]).
Tablet (delayed release): Initial: 300 mg twice daily on day 1 followed by 300 mg once daily on day 2 and thereafter. Duration is based on recovery from neutropenia or immunosuppression.
Missed doses: Take as soon as remembered. If it is <12 hours until the next dose, skip the missed dose and return to the regular schedule. Do not double doses.
IV: Loading dose: 300 mg twice a day on day 1 followed by 300 mg once daily on day 2 and thereafter. Duration is based on recovery from neutropenia or immunosuppression.
Treatment (refractory to or intolerant of conventional therapy) (off-label use):
Oral:
Suspension: 200 mg 3 times daily (IDSA [Patterson 2016]) or 200 mg 4 times daily, then may switch to 400 mg twice daily for outpatients (IDSA [Tunkel 2017]; Pitisuttithum 2005; Walsh 2007).
Tablet (delayed release): Initial: 300 mg twice daily on day 1; Maintenance: 300 mg once daily (IDSA [Patterson 2016])
IV: Loading dose: 300 mg twice daily on day 1; Maintenance: 300 mg once daily (IDSA [Patterson 2016])
Duration of therapy: Minimum of 6 to 12 weeks, although duration is highly dependent on degree/duration of immunosuppression, disease site, and evidence of disease improvement (IDSA [Patterson 2016])
Candidiasis:
Prophylaxis (disseminated candidiasis, immunocompromised host):
Oral:
Suspension: 200 mg 3 times daily; duration of therapy is based on recovery from neutropenia or immunosuppression
Tablet (delayed release): Initial: 300 mg twice daily on day 1; Maintenance: 300 mg once daily on day 2 and thereafter; duration of therapy is based on recovery from neutropenia or immunosuppression
Missed doses: Take as soon as remembered. If it is <12 hours until the next dose, skip the missed dose and return to the regular schedule. Do not double doses.
IV: Initial: 300 mg twice daily on day 1; Maintenance: 300 mg once daily on day 2 and thereafter; duration of therapy is based on recovery from neutropenia or immunosuppression.
Treatment:
Oral:
Oropharyngeal infection: Suspension: Initial: 100 mg twice daily on day 1; Maintenance: 100 mg once daily on day 2 and thereafter for 13 days
Oropharyngeal infection (refractory to fluconazole):
Suspension: 400 mg twice daily (manufacturer's labeling) for 3 days, then 400 mg once daily for up to 28 days (IDSA [Pappas 2016])
HIV-infected patients (alternative to fluconazole or azole refractory): Suspension: 400 mg twice daily on day 1, then 400 mg once daily for 7 to 14 days for initial episodes (continue for 28 days in azole refractory patients) (HHS [OI adult] 2019)
Esophageal infections (off-label use):
Fluconazole-refractory (alternate therapy):
Tablet (delayed-release): 300 mg once daily (IDSA [Pappas 2016])
Suspension: 400 mg twice daily (IDSA [Pappas 2016])
HIV-infected patients (azole refractory): Suspension: 400 mg twice daily for 28 days. Note: If patient has frequent or severe recurrences, may continue for suppressive therapy; consider discontinuing when CD4 >200/mm3 (HHS [OI adult] 2019)
Coccidioidomycosis (refractory to conventional therapy) (off-label use):
Nonmeningeal infection: Oral:
Tablet (delayed-release): Initial: 300 mg twice daily on day 1; Maintenance: 300 mg once daily on day 2 and thereafter (HHS [OI adult] 2019).
Suspension: 400 mg twice daily (Anstead 2005; HHS [OI adult] 2019; Stevens 2007).
Duration of therapy: Varies by site and severity of infection, as well as host immunocompetence (HHS [OI adult] 2019; IDSA [Galgiani 2016]).
Meningeal infection: Oral:
Tablet (delayed-release): Initial: 300 mg twice daily on day 1; Maintenance: 300 mg once daily on day 2 and thereafter (HHS [OI adult] 2019). Some experts recommend a higher maintenance dose of 200 to 300 mg twice daily, with routine therapeutic drug monitoring (Kauffman 2019).
Suspension: 200 mg 4 times daily or 400 mg twice daily (Pitisuttithum 2005; Schein 2011).
Duration of therapy: Continue lifelong as there is a high relapse rate when the dose is decreased or treatment is discontinued (HHS [OI adult] 2019; IDSA [Galgiani 2016]).
Cryptococcal infections (off-label use):
Pulmonary, nonimmunosuppressed (alternative agent): Oral: Suspension: 400 mg twice daily (Perfect 2010; Raad 2006).
Salvage treatment of relapsed infection: Oral: Suspension: 400 mg twice daily (or 200 mg 4 times daily) for 10 to 12 weeks. Note: Salvage treatment should only be started after an appropriate course of an induction regimen (Perfect 2010; Pitisuttithum 2005).
Mucormycosis, salvage and step-down therapy (off-label use):
Oral:
Suspension: 800 mg/day in 2 or 4 divided doses (Danion 2015; ECIL [Tissot 2017]; ESCMID/ECMM [Cornely 2014]; Greenberg 2006; van Burik 2006).
Tablet (delayed release): Initial: 300 mg twice daily on day 1; Maintenance: 300 mg once daily on day 2 and thereafter (Cox 2019).
IV: Initial: 300 mg every 12 hours on day 1; Maintenance: 300 mg every 24 hours thereafter (Cox 2019).
Duration of therapy: Varies based on clinical and radiologic response and host immunocompetence (Cox 2019).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Verify correct dosage form; the delayed release tablet and oral suspension are not interchangeable.
Antifungal prophylaxis, HSCT recipients: Limited data available:
Infants ≥8 months and Children <12 years: Oral suspension: 4 mg/kg/dose 3 times daily; begin 2-4 days prior to discharge and continue until either day 100 post-HSCT or until CD3 T cells reach 200/mm3 and CD4 cells reach 100/mm3 whichever is longer. Dosing based on experience in 60 pediatric patients (median age: 6 years; age range: 0.7-11.5 years); pharmacokinetic analysis showed 12 mg/kg/day (4 mg/kg 3 times daily) produced morning serum trough concentration similar to effective adult values. The other evaluated regimen of 10 mg/kg/day (5 mg/kg twice daily) produced morning trough levels that were approximately 3 times lower than the thrice daily regimen and was subsequently removed from the protocol. Overall, no patients developed invasive mycosis (probable or proven), the median duration of therapy was 127 days (range: 12-188 days), and no severe adverse effects were observed (Döring, 2012).
Adolescents ≥13 years: Oral suspension: 200 mg 3 times daily beginning with GVHD diagnosis, continue until GVHD resolves (Science, 2014)
Antifungal prophylaxis, acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS): Limited data available: Adolescents ≥13 years: Oral suspension: 200 mg 3 times daily during chemotherapy associated neutropenia (Science, 2014). Note: Consider in centers with high incidence of mold infections or if fluconazole not available.
Aspergillosis, invasive; prophylaxis:
Oral: Adolescents ≥13 years:
Oral delayed release tablets (preferred): Initial: 300 mg twice daily for 1 day; maintenance dose: 300 mg once daily starting on Day 2; duration is based on recovery from neutropenia or immunosuppression. Missed doses: Take as soon as remembered. If it is <12 hours until the next dose, skip the missed dose and return to the regular schedule. Do not double doses.
Oral suspension: 200 mg 3 times daily; duration of therapy is based on recovery from neutropenia or immunosuppression. Missed doses: Take as soon as remembered. If it is <12 hours until the next dose, skip the missed dose and return to the regular schedule. Do not double doses.
IV: Adolescents ≥18 years: Loading dose: 300 mg twice a day on day 1; maintenance dose: 300 mg once daily on day 2 and thereafter. Duration is based on recovery from neutropenia or immunosuppression.
Candidiasis:
Esophageal infection; azole -refractory (HIV-exposed/-positive): Treatment: Adolescent: Oral suspension: 400 mg twice daily for 28 days; Note: If patient has frequent or severe recurrences may continue for suppressive therapy; consider discontinuing when CD4 >200/mm3 (DHHS [adult], 2014)
Invasive infections:
Prophylaxis: Adolescents ≥13 years:
Oral delayed release tablets (preferred): Initial: 300 mg twice daily for 1 day; maintenance dose: 300 mg once daily. Duration is based on recovery from neutropenia or immunosuppression. Missed doses: Take as soon as remembered. If it is <12 hours until the next dose, skip the missed dose and return to the regular schedule. Do not double doses.
Oral suspension: 200 mg 3 times daily; duration of therapy is based on recovery from neutropenia or immunosuppression. Missed doses: Take as soon as remembered. If it is <12 hours until the next dose, skip the missed dose and return to the regular schedule. Do not double doses.
Treatment (refractory infection): Limited data available: Children ≥8 years and Adolescents: Oral suspension: 800 mg/day administered as either 200 mg 4 times daily or 400 mg twice daily; this regimen produced similar plasma concentrations in both children (n=12; age range: 8-17 years; weight: 24-76 kg) and adults (Krishna, 2007)
Oropharyngeal infection:
Non-HIV-exposed/-positive: Adolescents ≥13 years:
Treatment: Oral suspension: Initial: 100 mg twice daily on day 1; maintenance: 100 mg once daily for 13 days
Treatment (refractory infection): Oral suspension: 400 mg twice daily; duration of therapy is based on underlying disease and clinical response
HIV-exposed/-positive: Treatment: Adolescents: Oral suspension: Initial: 400 mg twice daily on day 1; maintenance: 400 mg once daily for 28 days (DHHS [adult], 2014)
Reconstitution
IV: Equilibrate the refrigerated vial to room temperature. Contents of vial should be withdrawn and admixed with D5W, D5W with KCl 20 mEq, D5NS, D51/2NS, 1/2NS, or NS to achieve a concentration of 1 to 2 mg/mL. The admixed solution may be colorless to yellow. Color variations in this range do not affect potency. Admixture should be used immediately; may be stored for up to 24 hours between 2°C and 8°C (36°F and 46°F).
Administration
Oral:
Suspension: Shake well before use. Administer with provided measured dosing spoon during or within 20 minutes following a full meal; patients who are unable to eat a full meal may take each dose with an oral liquid nutritional supplement or acidic carbonated beverage (eg, ginger ale). Consider an alternative antifungal in patients unable to eat a full meal or tolerate a liquid nutritional supplement or acidic carbonated beverage and who do not have the option of taking the delayed-release tablet or injection.
Tablets (delayed release): Swallow tablets whole; do not divide, crush, dissolve, or chew. Administer with food.
Closely monitor patients with severe diarrhea or vomiting for breakthrough fungal infections.
IV: Infuse over 90 minutes via a central venous line. Do not administer IV push or bolus. Must be infused through an in-line filter (0.22-micron polyethersulfone [PES] or polyvinylidene difluoride [PVDF]). Infusion through a peripheral line should only be used as a one-time infusion over 30 minutes in a patient who will be receiving a central venous line for subsequent doses, or to bridge a period during which a central venous line is to be replaced or is in use for another infusion. May be an irritant. Note: In clinical trials, multiple peripheral infusions given through the same vein resulted in infusion-site reactions.
Dietary Considerations
Tablets (delayed release): Take with food.
Suspension: Give during or within 20 minutes following a full meal, liquid nutritional supplement, or an acidic carbonated beverage (eg, ginger ale).
Consider alternative antifungal therapy in patients with inadequate oral intake or severe diarrhea/vomiting; if alternative therapy is not an option, closely monitoring for breakthrough fungal infections.
Adequate posaconazole absorption from GI tract and subsequent plasma concentrations are dependent on food for efficacy. Lower average plasma concentrations have been associated with an increased risk of treatment failure.
Storage
Suspension: Store at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Do not freeze.
Tablets: Store between 20°C and 25°C (68°F and 77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F).
Injection: Store at 2°C to 8°C (36°F to 46°F).
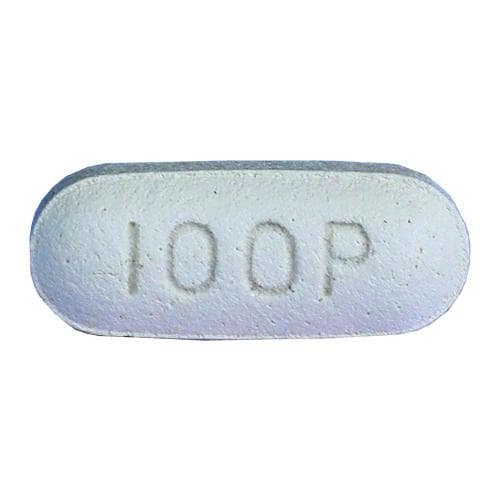
Posaconazole Images
Drug Interactions
Abemaciclib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Abemaciclib. Management: In patients taking abemaciclib at a dose of 200 mg or 150 mg twice daily, reduce the dose to 100 mg twice daily when combined with strong CYP3A4 inhibitors. In patients taking abemaciclib 100 mg twice daily, decrease the dose to 50 mg twice daily. Consider therapy modification
Acalabrutinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Acalabrutinib. Avoid combination
Ado-Trastuzumab Emtansine: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Ado-Trastuzumab Emtansine. Specifically, strong CYP3A4 inhibitors may increase concentrations of the cytotoxic DM1 component. Avoid combination
Alfuzosin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Alfuzosin. Avoid combination
Alitretinoin (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Alitretinoin (Systemic). Management: Consider reducing the alitretinoin dose to 10 mg when used together with strong CYP3A4 inhibitors. Monitor for increased alitretinoin effects/toxicities if combined with a strong CYP3A4 inhibitor. Consider therapy modification
Almotriptan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Almotriptan. Management: Limit initial almotriptan adult dose to 6.25 mg and maximum adult dose to 12.5 mg/24-hrs when used with a strong CYP3A4 inhibitor. Avoid concurrent use in patients with impaired hepatic or renal function. Consider therapy modification
Alosetron: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Alosetron. Monitor therapy
ALPRAZolam: CYP3A4 Inhibitors (Strong) may increase the serum concentration of ALPRAZolam. Management: Consider using an alternative agent that is less likely to interact. If combined, monitor for increased therapeutic/toxic effects of alprazolam if combined with a strong CYP3A4 inhibitor. Consider therapy modification
Amphotericin B: Antifungal Agents (Azole Derivatives, Systemic) may diminish the therapeutic effect of Amphotericin B. Monitor therapy
Antineoplastic Agents (Vinca Alkaloids): Posaconazole may enhance the adverse/toxic effect of Antineoplastic Agents (Vinca Alkaloids). Posaconazole may increase the serum concentration of Antineoplastic Agents (Vinca Alkaloids). Management: Avoid the concomitant use of posaconazole and vinca alkaloids when possible. If combined, monitor for increased vinca alkaloid toxicities (eg, neurotoxicity, gastrointestinal toxicity). Consider therapy modification
Apalutamide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Apalutamide. Monitor therapy
Apixaban: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Apixaban. Monitor therapy
Aprepitant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Aprepitant. Avoid combination
ARIPiprazole: CYP3A4 Inhibitors (Strong) may increase the serum concentration of ARIPiprazole. Management: See full interaction monograph for details. Consider therapy modification
ARIPiprazole Lauroxil: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of ARIPiprazole Lauroxil. Management: Please refer to the full interaction monograph for details concerning the recommended dose adjustments. Consider therapy modification
Astemizole: Posaconazole may increase the serum concentration of Astemizole. Avoid combination
Asunaprevir: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Asunaprevir. Avoid combination
Atazanavir: Posaconazole may increase the serum concentration of Atazanavir. Monitor therapy
AtorvaSTATin: Posaconazole may increase the serum concentration of AtorvaSTATin. Avoid combination
Avanafil: Posaconazole may increase the serum concentration of Avanafil. Avoid combination
Avapritinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Avapritinib. Avoid combination
Axitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Axitinib. Management: Avoid concurrent use of axitinib with any strong CYP3A inhibitor whenever possible. If a strong CYP3A inhibitor must be used with axitinib, a 50% axitinib dose reduction is recommended. Consider therapy modification
Barnidipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Barnidipine. Avoid combination
Benperidol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Benperidol. Monitor therapy
Benzhydrocodone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Benzhydrocodone. Specifically, the concentration of hydrocodone may be increased. Monitor therapy
Betamethasone (Ophthalmic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Betamethasone (Ophthalmic). Monitor therapy
Bictegravir: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bictegravir. Monitor therapy
Blonanserin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Blonanserin. Avoid combination
Bortezomib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bortezomib. Monitor therapy
Bosentan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bosentan. Management: Concomitant use of both a CYP2C9 inhibitor and a CYP3A inhibitor or a single agent that inhibits both enzymes with bosentan is likely to cause a large increase in serum concentrations of bosentan and is not recommended. See monograph for details. Monitor therapy
Bosutinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bosutinib. Avoid combination
Brentuximab Vedotin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be increased. Monitor therapy
Brexpiprazole: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Brexpiprazole. Management: Reduce brexpiprazole dose 50% with strong CYP3A4 inhibitors; reduce to 25% of usual if used with both a moderate CYP3A4 inhibitor and a CYP2D6 inhibitor in patients not being treated for MDD, or strong CYP3A4 inhibitor used in a CYP2D6 poor metabolizer. Consider therapy modification
Brigatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Brigatinib. Management: Avoid concurrent use of brigatinib with strong CYP3A4 inhibitors when possible. If combination cannot be avoided, reduce the brigatinib dose by approximately 50%, rounding to the nearest tablet strength (ie, from 180 mg to 90 mg, or from 90 mg to 60 mg). Consider therapy modification
Brinzolamide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Brinzolamide. Monitor therapy
Bromocriptine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bromocriptine. Avoid combination
Budesonide (Nasal): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Budesonide (Nasal). Monitor therapy
Budesonide (Oral Inhalation): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Budesonide (Oral Inhalation). Monitor therapy
Budesonide (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Budesonide (Systemic). Avoid combination
Budesonide (Topical): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Budesonide (Topical). Management: Per US prescribing information, avoid this combination. Canadian product labeling does not recommend strict avoidance. If combined, monitor for excessive glucocorticoid effects as budesonide exposure may be increased. Consider therapy modification
Buprenorphine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Buprenorphine. Monitor therapy
BusPIRone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of BusPIRone. Management: Limit the buspirone dose to 2.5 mg daily and monitor patients for increased buspirone effects/toxicities if combined with strong CYP3A4 inhibitors. Consider therapy modification
Busulfan: Antifungal Agents (Azole Derivatives, Systemic) may increase the serum concentration of Busulfan. Isavuconazonium considerations are addressed in separate monographs. Monitor therapy
Cabazitaxel: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cabazitaxel. Management: Concurrent use of cabazitaxel with strong inhibitors of CYP3A4 should be avoided when possible. If such a combination must be used, consider a 25% reduction in the cabazitaxel dose. Consider therapy modification
Cabozantinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cabozantinib. Management: Avoid use of a strong CYP3A4 inhibitor with cabozantinib if possible. If combined, cabozantinib dose adjustments are recommended and vary based on the cabozantinib product used and the indication for use. See monograph for details. Consider therapy modification
Calcifediol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Calcifediol. Monitor therapy
Calcium Channel Blockers: Antifungal Agents (Azole Derivatives, Systemic) may enhance the adverse/toxic effect of Calcium Channel Blockers. Specifically, itraconazole may enhance the negative inotropic effects of verapamil or diltiazem. Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of Calcium Channel Blockers. Fluconazole and isavuconazonium likely exert weaker effects than other azoles and are addressed in separate monographs. Management: Concurrent use of felodipine or nisoldipine with itraconazole is specifically contraindicated. Frequent monitoring is warranted with any such combination; calcium channel blocker dose reductions may be required. Exceptions: Clevidipine. Consider therapy modification
Cannabidiol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cannabidiol. Monitor therapy
Cannabis: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cannabis. More specifically, tetrahydrocannabinol and cannabidiol serum concentrations may be increased. Monitor therapy
Cariprazine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cariprazine. Management: Cariprazine dose reductions of 50% are required; specific recommended management varies slightly for those stable on cariprazine versus those just starting cariprazine. See prescribing information or full interaction monograph for details. Consider therapy modification
Cilostazol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cilostazol. Management: Consider reducing the cilostazol dose to 50 mg twice daily in adult patients who are also receiving strong inhibitors of CYP3A4. Consider therapy modification
Cinacalcet: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cinacalcet. Monitor therapy
Cisapride: Posaconazole may increase the serum concentration of Cisapride. Avoid combination
CloZAPine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of CloZAPine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Cobimetinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cobimetinib. Avoid combination
Codeine: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Codeine. Monitor therapy
Colchicine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Colchicine. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a strong CYP3A4 inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. See full monograph for details. Consider therapy modification
Conivaptan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Conivaptan. Avoid combination
Copanlisib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Copanlisib. Management: If concomitant use of copanlisib and strong CYP3A4 inhibitors cannot be avoided, reduce the copanlisib dose to 45 mg. Monitor patients for increased copanlisib effects/toxicities. Consider therapy modification
Corticosteroids (Orally Inhaled): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Corticosteroids (Orally Inhaled). Management: Orally inhaled fluticasone propionate with a strong CYP3A4 inhibitor is not recommended. Exceptions: Beclomethasone (Oral Inhalation); Triamcinolone (Systemic). Monitor therapy
Corticosteroids (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Corticosteroids (Systemic). Exceptions: MethylPREDNISolone; PrednisoLONE (Systemic); PredniSONE. Monitor therapy
CycloSPORINE (Systemic): Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of CycloSPORINE (Systemic). Fluconazole and isavuconazonium considerations are addressed in separate monographs. Consider therapy modification
CycloSPORINE (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of CycloSPORINE (Systemic). Consider therapy modification
CYP3A4 Substrates (High risk with Inhibitors): CYP3A4 Inhibitors (Strong) may decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Exceptions: Alitretinoin (Systemic); AmLODIPine; Benzhydrocodone; Buprenorphine; Gefitinib; HYDROcodone; Mirtazapine; Praziquantel; Telithromycin; Vinorelbine. Consider therapy modification
Dabrafenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dabrafenib. Avoid combination
Daclatasvir: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Daclatasvir. Management: Decrease the daclatasvir dose to 30 mg once daily if combined with a strong CYP3A4 inhibitor. No dose adjustment is needed when daclatasvir is used with darunavir/cobicistat. Consider therapy modification
Dapoxetine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dapoxetine. Avoid combination
Deflazacort: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Deflazacort. Management: Administer one third of the recommended deflazacort dose when used together with a strong or moderate CYP3A4 inhibitor. Consider therapy modification
DexAMETHasone (Ophthalmic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of DexAMETHasone (Ophthalmic). Monitor therapy
Dichlorphenamide: Antifungal Agents (Azole Derivatives, Systemic) may enhance the hypokalemic effect of Dichlorphenamide. Monitor therapy
Didanosine: May decrease the absorption of Antifungal Agents (Azole Derivatives, Systemic). Enteric coated didanosine capsules are not expected to affect these antifungals. Consider therapy modification
Dienogest: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dienogest. Monitor therapy
Digoxin: Posaconazole may increase the serum concentration of Digoxin. Monitor therapy
Dihydroergotamine: Posaconazole may increase the serum concentration of Dihydroergotamine. Avoid combination
DOCEtaxel: CYP3A4 Inhibitors (Strong) may increase the serum concentration of DOCEtaxel. Management: Avoid the concomitant use of docetaxel and strong CYP3A4 inhibitors when possible. If combined use is unavoidable, consider a 50% docetaxel dose reduction and monitor for increased docetaxel toxicities. Consider therapy modification
Dofetilide: Posaconazole may increase the serum concentration of Dofetilide. Avoid combination
Domperidone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Domperidone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
Doxercalciferol: CYP3A4 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Doxercalciferol. Monitor therapy
DOXOrubicin (Conventional): CYP3A4 Inhibitors (Strong) may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to strong CYP3A4 inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Dronabinol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dronabinol. Monitor therapy
Dronedarone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dronedarone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
Drospirenone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Drospirenone. Management: Drospirenone use is contraindicated specifically when the strong CYP3A4 inhibitors atazanavir and cobicistat are administered concurrently. Caution should be used when drospirenone is coadministered with other strong CYP3A4 inhibitors. Consider therapy modification
Dutasteride: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dutasteride. Monitor therapy
Duvelisib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Duvelisib. Management: Reduce the dose of duvelisib to 15 mg twice a day when used together with a strong CYP3A4 inhibitor. Consider therapy modification
Efavirenz: May decrease the serum concentration of Posaconazole. Avoid combination
Elagolix: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Elagolix. Management: Use of the elagolix 200 mg twice daily dose with a strong CYP3A4 inhibitor for longer than 1 month is not recommended. Limit combined use of the elagolix 150 mg once daily dose with a strong CYP3A4 inhibitor to a maximum of 6 months. Consider therapy modification
Eletriptan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Eletriptan. Avoid combination
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Management: When combined with strong CYP3A4 inhibitors, administer two elexacaftor/tezacaftor/ivacaftor tablets (100 mg/50 mg/75 mg) in the morning, twice a week, approximately 3 to 4 days apart. No evening doses of ivacaftor (150 mg) alone should be administered. Consider therapy modification
Eliglustat: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Eliglustat. Management: Use should be avoided under some circumstances. See full drug interaction monograph for details. Consider therapy modification
Enfortumab Vedotin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Enfortumab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be increased. Monitor therapy
Enzalutamide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Enzalutamide. Monitor therapy
Eplerenone: Posaconazole may increase the serum concentration of Eplerenone. Avoid combination
Erdafitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Erdafitinib. Management: Avoid concomitant use of erdafitinib and strong CYP3A4 inhibitors when possible. If combined, monitor closely for erdafitinib adverse reactions and consider dose modifications accordingly. Consider therapy modification
Ergoloid Mesylates: Posaconazole may increase the serum concentration of Ergoloid Mesylates. Avoid combination
Ergonovine: Posaconazole may increase the serum concentration of Ergonovine. Avoid combination
Ergotamine: Posaconazole may increase the serum concentration of Ergotamine. Avoid combination
Erlotinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Erlotinib. Management: Avoid use of this combination when possible. When the combination must be used, monitor the patient closely for the development of severe adverse reactions, and if such severe reactions occur, reduce the erlotinib dose (in 50 mg decrements). Consider therapy modification
Estrogen Derivatives: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Estrogen Derivatives. Monitor therapy
Eszopiclone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Eszopiclone. Management: Limit the eszopiclone dose to 2 mg daily when combined with strong CYP3A4 inhibitors and monitor for increased eszopiclone effects and toxicities (eg, somnolence, drowsiness, CNS depression). Consider therapy modification
Etizolam: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Etizolam. Management: Consider use of lower etizolam doses when using this combination; specific recommendations concerning dose adjustment are not available. Monitor clinical response to the combination closely. Consider therapy modification
Etravirine: Antifungal Agents (Azole Derivatives, Systemic) may increase the serum concentration of Etravirine. Applicable Isavuconazonium considerations are addressed in separate monographs. Etravirine may decrease the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). This would be anticipated with itraconazole or ketoconazole. Etravirine may increase the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). This would be anticipated with voriconazole. Management: Monitor for increased effects/toxicity of etravirine. Antifungal dose adjustment may be needed for ketoconazole, itraconazole, or posaconazole but specific dosing guidelines are lacking. Consider therapy modification
Everolimus: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Everolimus. Avoid combination
Evogliptin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Evogliptin. Monitor therapy
Fedratinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Fedratinib. Management: Consider alternatives when possible. If used together, decrease fedratinib dose to 200 mg/day. After the inhibitor is stopped, increase fedratinib to 300 mg/day for the first 2 weeks and then to 400 mg/day as tolerated. Consider therapy modification
FentaNYL: CYP3A4 Inhibitors (Strong) may increase the serum concentration of FentaNYL. Management: Monitor patients closely for several days following initiation of this combination, and adjust fentanyl dose as necessary. Consider therapy modification
Fesoterodine: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Fesoterodine. Management: Avoid fesoterodine doses greater than 4 mg daily in adult patients who are also receiving strong CYP3A4 inhibitors. Consider therapy modification
Flibanserin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Flibanserin. Avoid combination
Fluticasone (Nasal): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Fluticasone (Nasal). Avoid combination
Fluticasone (Oral Inhalation): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Fluticasone (Oral Inhalation). Management: Use of orally inhaled fluticasone propionate with strong CYP3A4 inhibitors is not recommended. Use of orally inhaled fluticasone furoate with strong CYP3A4 inhibitors should be done with caution. Monitor patients using such a combination more closely. Consider therapy modification
Fosamprenavir: Posaconazole may increase serum concentrations of the active metabolite(s) of Fosamprenavir. Fosamprenavir may decrease the serum concentration of Posaconazole. Monitor therapy
Fosaprepitant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Fosaprepitant. Avoid combination
Fosphenytoin: May decrease the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). Antifungal Agents (Azole Derivatives, Systemic) may increase the serum concentration of Fosphenytoin. Applicable Isavuconazonium considerations are addressed in separate monographs. Consider therapy modification
Fostamatinib: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Fostamatinib. Monitor therapy
Galantamine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Galantamine. Monitor therapy
Gefitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Gefitinib. Monitor therapy
Glasdegib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Glasdegib. Management: Consider alternatives to this combination when possible. If the combination must be used, monitor closely for evidence of QT interval prolongation and other adverse reactions to glasdegib. Consider therapy modification
GlipiZIDE: Posaconazole may enhance the hypoglycemic effect of GlipiZIDE. Posaconazole may increase the serum concentration of GlipiZIDE. Monitor therapy
GuanFACINE: CYP3A4 Inhibitors (Strong) may increase the serum concentration of GuanFACINE. Management: Reduce the guanfacine dose by 50% when initiating this combination. Consider therapy modification
Halofantrine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Halofantrine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
Histamine H2 Receptor Antagonists: May decrease the serum concentration of Posaconazole. Management: Avoid concurrent use of oral suspension with H2-antagonists whenever possible. Monitor patients closely for decreased antifungal effects if this combination is used. Delayed-release posaconazole tablets may be less likely to interact. Consider therapy modification
HYDROcodone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of HYDROcodone. Monitor therapy
Ibrutinib: Posaconazole may increase the serum concentration of Ibrutinib. Management: Ibrutinib dose reductions are required when combined with posaconazole. Dose recommendations depend on the indication for ibrutinib and the posaconazole dose. See full monograph for details. Consider therapy modification
Idelalisib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Idelalisib. Monitor therapy
Ifosfamide: CYP3A4 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Iloperidone: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Iloperidone. Specifically, concentrations of the metabolites P88 and P95 may be increased. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Iloperidone. Management: Reduce iloperidone dose by half when administered with a strong CYP3A4 inhibitor. Consider therapy modification
Imatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Imatinib. Monitor therapy
Imidafenacin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Imidafenacin. Monitor therapy
Irinotecan Products: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Irinotecan Products. Specifically, serum concentrations of SN-38 may be increased. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Irinotecan Products. Avoid combination
Isavuconazonium Sulfate: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Isavuconazonium Sulfate. Specifically, CYP3A4 Inhibitors (Strong) may increase isavuconazole serum concentrations. Management: Combined use is considered contraindicated per US labeling. Lopinavir/ritonavir (and possibly other uses of ritonavir doses less than 400 mg every 12 hours) is treated as a possible exception to this contraindication despite strongly inhibiting CYP3A4. Avoid combination
Istradefylline: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Istradefylline. Management: Limit the maximum istradefylline dose to 20 mg daily when combined with strong CYP3A4 inhibitors and monitor for increased istradefylline effects/toxicities. Consider therapy modification
Ivabradine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ivabradine. Avoid combination
Ivacaftor: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ivacaftor. Management: Ivacaftor dose reductions are required; consult full monograph content for age- and weight-specific recommendations. Consider therapy modification
Ixabepilone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ixabepilone. Consider therapy modification
Lacosamide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lacosamide. Monitor therapy
Lapatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lapatinib. Management: If an overlap in therapy cannot be avoided, consider reducing lapatinib adult dose to 500 mg/day during, and within 1 week of completing, treatment with the strong CYP3A4 inhibitor. Avoid combination
Larotrectinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Larotrectinib. Management: Avoid use of strong CYP3A4 inhibitors with larotrectinib. If this combination cannot be avoided, reduce the larotrectinib dose by 50%. Increase to previous dose after stopping the inhibitor after a period of 3 to 5 times the inhibitor half-life. Consider therapy modification
Lefamulin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin tablets and strong inhibitors of CYP3A4. Avoid combination
Lemborexant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lemborexant. Avoid combination
Lercanidipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lercanidipine. Avoid combination
Levobupivacaine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Levobupivacaine. Monitor therapy
Levomilnacipran: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Levomilnacipran. Management: Do not exceed a maximum adult levomilnacipran dose of 80 mg/day in patients also receiving strong CYP3A4 inhibitors. Consider therapy modification
Lomitapide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lomitapide. Avoid combination
Lorlatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lorlatinib. Management: Avoid use of lorlatinib with strong CYP3A4 inhibitors. If the combination cannot be avoided, reduce the lorlatinib dose from 100 mg once daily to 75 mg once daily, or from 75 mg once daily to 50 mg once daily. Consider therapy modification
Losartan: Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of Losartan. Applicable Isavuconazonium considerations are addressed in separate monographs. Monitor therapy
Lovastatin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lovastatin. Avoid combination
Lumacaftor and Ivacaftor: May decrease the serum concentration of Posaconazole. Management: Concurrent use of lumacaftor/ivacaftor and posaconazole is not recommended. Consider an alternative antifungal such as fluconazole if appropriate. If this combination cannot be avoided, monitor patients for decreased posaconazole efficacy. Consider therapy modification
Lumateperone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lumateperone. Avoid combination
Lumefantrine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lumefantrine. Monitor therapy
Lurasidone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lurasidone. Avoid combination
Macitentan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Macitentan. Avoid combination
Manidipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Manidipine. Management: Consider avoiding concomitant use of manidipine and strong CYP3A4 inhibitors. If combined, monitor closely for increased manidipine effects and toxicities. Manidipine dose reductions may be required. Consider therapy modification
Maraviroc: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Maraviroc. Management: Reduce the adult dose of maraviroc to 150 mg twice daily when used with a strong CYP3A4 inhibitor. Do not use maraviroc with strong CYP3A4 inhibitors in patients with Clcr less than 30 mL/min. Consider therapy modification
MedroxyPROGESTERone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of MedroxyPROGESTERone. Monitor therapy
Meperidine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Meperidine. Monitor therapy
Methadone: Posaconazole may enhance the QTc-prolonging effect of Methadone. Posaconazole may increase the serum concentration of Methadone. Avoid combination
Methylergonovine: Posaconazole may increase the serum concentration of Methylergonovine. Avoid combination
MethylPREDNISolone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of MethylPREDNISolone. Management: Consider methylprednisolone dose reduction in patients receiving strong CYP3A4 inhibitors and monitor for increased steroid related adverse effects. Consider therapy modification
Metoclopramide: May decrease the serum concentration of Posaconazole. Monitor therapy
MiFEPRIStone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of MiFEPRIStone. Management: Limit mifepristone adult dose, when used for treatment of hyperglycemia in Cushing's syndrome, to a maximum of 900 mg/day when combined with a strong CYP3A4 inhibitor. Monitor for increased mifepristone toxicity regardless of dose or indication. Consider therapy modification
Mirodenafil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Mirodenafil. Management: Consider using a lower dose of mirodenafil when used with strong CYP3A4 inhibitors. Monitor for increased mirodenafil effects/toxicities with the use of this combination. Consider therapy modification
Mirtazapine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Mirtazapine. Monitor therapy
Mizolastine: Antifungal Agents (Azole Derivatives, Systemic) may increase the serum concentration of Mizolastine. Avoid combination
Naldemedine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Naldemedine. Monitor therapy
Nalfurafine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Nalfurafine. Monitor therapy
Naloxegol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Naloxegol. Avoid combination
Neratinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Neratinib. Avoid combination
NiMODipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of NiMODipine. Avoid combination
Nisoldipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Nisoldipine. Avoid combination
Olaparib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Olaparib. Management: Avoid use of strong CYP3A4 inhibitors in patients being treated with olaparib, if possible. If such concurrent use cannot be avoided, the dose of olaparib should be reduced to 100 mg twice daily. Consider therapy modification
Ospemifene: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ospemifene. Monitor therapy
Oxybutynin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Oxybutynin. Monitor therapy
OxyCODONE: CYP3A4 Inhibitors (Strong) may enhance the adverse/toxic effect of OxyCODONE. CYP3A4 Inhibitors (Strong) may increase the serum concentration of OxyCODONE. Serum concentrations of the active metabolite oxymorphone may also be increased. Consider therapy modification
Palbociclib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Palbociclib. Avoid combination
Panobinostat: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Panobinostat. Management: Reduce the panobinostat dose to 10 mg when it must be used with a strong CYP3A4 inhibitor. Consider therapy modification
Parecoxib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Parecoxib. Monitor therapy
Paricalcitol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Paricalcitol. Monitor therapy
PAZOPanib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of PAZOPanib. Management: Avoid concurrent use of pazopanib with strong inhibitors of CYP3A4 whenever possible. If it is not possible to avoid such a combination, reduce pazopanib adult dose to 400 mg. Further dose reductions may also be required. Consider therapy modification
Pexidartinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Pexidartinib. Management: Avoid use of pexidartinib with strong CYP3A4 inhibitors if possible. If combined use cannot be avoided, the pexidartinib dose should be reduced. Decrease 800 mg or 600 mg daily doses to 200 mg twice daily. Decrease doses of 400 mg/day to 200 mg/day. Consider therapy modification
Phenytoin: Antifungal Agents (Azole Derivatives, Systemic) may increase the serum concentration of Phenytoin. Applicable Isavuconazonium considerations are addressed in separate monographs. Phenytoin may decrease the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). Management: Concomitant therapy with itraconazole, voriconazole, or ketoconazole and phenytoin should probably be avoided, as antifungal failure is likely. Consider selecting alternative antifungal therapy. Consider therapy modification
Pimavanserin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Pimavanserin. Management: Decrease the pimavanserin dose to 10 mg daily when combined with strong CYP3A4 inhibitors. Consider therapy modification
Pimecrolimus: CYP3A4 Inhibitors (Strong) may decrease the metabolism of Pimecrolimus. Monitor therapy
Pimozide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Pimozide. Avoid combination
Piperaquine: CYP3A4 Inhibitors (Strong) may enhance the QTc-prolonging effect of Piperaquine. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Piperaquine. Management: Avoid concomitant use of piperaquine and strong CYP3A4 inhibitors when possible. If the combination cannot be avoided, frequent ECG monitoring is recommended due to the risk for QTc prolongation. Exceptions are discussed separately. Consider therapy modification
Polatuzumab Vedotin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Polatuzumab Vedotin. Exposure to unconjugated MMAE, the cytotoxic small molecule component of polatuzumab vedotin, may be increased. Monitor therapy
PONATinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of PONATinib. Management: Per ponatinib U.S. prescribing information, the adult starting dose of ponatinib should be reduced to 30 mg daily during treatment with any strong CYP3A4 inhibitor. Consider therapy modification
Pranlukast: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Pranlukast. Monitor therapy
Praziquantel: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Praziquantel. Monitor therapy
PrednisoLONE (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of PrednisoLONE (Systemic). Monitor therapy
PredniSONE: CYP3A4 Inhibitors (Strong) may increase the serum concentration of PredniSONE. Monitor therapy
Propafenone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Propafenone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Proton Pump Inhibitors: May decrease the serum concentration of Posaconazole. Consider therapy modification
QT-prolonging CYP3A4 Substrates: Posaconazole may increase the serum concentration of QT-prolonging CYP3A4 Substrates. Such increases may lead to a greater risk for proarrhythmic effects and other similar toxicities. Avoid combination
QuiNIDine: Posaconazole may increase the serum concentration of QuiNIDine. Avoid combination
Radotinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Radotinib. Avoid combination
Ramelteon: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ramelteon. Monitor therapy
Ranolazine: Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of Ranolazine. Fluconazole and isavuconazonium considerations are addressed in separate monographs. Avoid combination
Ranolazine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ranolazine. Avoid combination
Reboxetine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Reboxetine. Consider therapy modification
Red Yeast Rice: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Red Yeast Rice. Specifically, concentrations of lovastatin and related compounds found in Red Yeast Rice may be increased. Avoid combination
Regorafenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Regorafenib. Avoid combination
Repaglinide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Repaglinide. Management: The addition of a CYP2C8 inhibitor to this drug combination may substantially increase the magnitude of increase in repaglinide exposure. Monitor therapy
Retapamulin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Retapamulin. Management: Avoid this combination in patients less than 2 years old. No action is required in other populations. Monitor therapy
Rifamycin Derivatives: Antifungal Agents (Azole Derivatives, Systemic) may increase the serum concentration of Rifamycin Derivatives. Only rifabutin appears to be affected. Rifamycin Derivatives may decrease the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). Management: Avoid these combinations when possible. Voriconazole and isavuconazonium are considered contraindicated. Consider therapy modification
Rilpivirine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Rilpivirine. Monitor therapy
Ritonavir: Posaconazole may increase the serum concentration of Ritonavir. Monitor therapy
RomiDEPsin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of RomiDEPsin. Monitor therapy
Rupatadine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Rupatadine. Avoid combination
Ruxolitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ruxolitinib. Management: This combination should be avoided under some circumstances. See monograph for details. Consider therapy modification
Saccharomyces boulardii: Antifungal Agents (Systemic, Oral) may diminish the therapeutic effect of Saccharomyces boulardii. Avoid combination
Salmeterol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Salmeterol. Avoid combination
SAXagliptin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of SAXagliptin. Management: Limit the saxagliptin dose to 2.5 mg daily when combined with strong CYP3A4 inhibitors. When using the saxagliptin combination products saxagliptin/dapagliflozin or saxagliptin/dapagliflozin/metformin, avoid use with strong CYP3A4 inhibitors. Consider therapy modification
Sibutramine: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Sibutramine. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Sibutramine. Monitor therapy
Sildenafil: Posaconazole may increase the serum concentration of Sildenafil. Management: Concurrent posaconazole is not recommended when sildenafil is used for treatment of pulmonary arterial hypertension. If sildenafil is used to treat erectile dysfunction, an initial dose of 25 mg is recommended with concurrent posaconazole. Consider therapy modification
Silodosin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Silodosin. Avoid combination
Simeprevir: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Simeprevir. Avoid combination
Simvastatin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Simvastatin. Avoid combination
Sirolimus: Posaconazole may increase the serum concentration of Sirolimus. Avoid combination
Solifenacin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Solifenacin. Management: Limit solifenacin doses to 5 mg daily when combined with strong CYP3A4 inhibitors. Consider therapy modification
Sonidegib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Sonidegib. Avoid combination
SORAfenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of SORAfenib. Monitor therapy
SUFentanil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of SUFentanil. Management: If a strong CYP3A4 inhibitor is initiated in a patient on sufentanil, consider a sufentanil dose reduction and monitor for increased sufentanil effects and toxicities (eg, respiratory depression). Consider therapy modification
SUNItinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of SUNItinib. Management: Avoid when possible. If such a combination cannot be avoided, sunitinib dose decreases are recommended, and vary by indication. See full monograph for details. Consider therapy modification
Suvorexant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Suvorexant. Avoid combination
Tacrolimus (Systemic): Posaconazole may increase the serum concentration of Tacrolimus (Systemic). Management: Reduce tacrolimus dose to approximately one-third of original dose when starting posaconazole. Tacrolimus blood concentrations should be monitored closely during and at discontinuation of posaconazole. Consider therapy modification
Tacrolimus (Topical): Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of Tacrolimus (Topical). Applicable Isavuconazonium considerations are addressed in separate monographs. Monitor therapy
Tadalafil: Posaconazole may increase the serum concentration of Tadalafil. Consider therapy modification
Tamsulosin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tamsulosin. Avoid combination
Tasimelteon: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tasimelteon. Monitor therapy
Tazemetostat: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tazemetostat. Avoid combination
Telithromycin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Telithromycin. Monitor therapy
Temsirolimus: Posaconazole may increase serum concentrations of the active metabolite(s) of Temsirolimus. Management: Consider temsirolimus dose reductions or alternatives to posaconazole. Monitor sirolimus concentrations in all patients receiving posaconazole or any systemic azole antifungal. Consider therapy modification
Terfenadine: Posaconazole may increase the serum concentration of Terfenadine. Avoid combination
Tetrahydrocannabinol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tetrahydrocannabinol. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tetrahydrocannabinol and Cannabidiol. Monitor therapy
Tezacaftor and Ivacaftor: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tezacaftor and Ivacaftor. Management: When combined with strong CYP3A4 inhibitors, tezacaftor/ivacaftor should be administered in the morning, twice a week, approximately 3 to 4 days apart. No evening doses of ivacaftor alone should be administered. Consider therapy modification
Thiotepa: CYP3A4 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Thiotepa. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Thiotepa. Management: Thiotepa prescribing information recommends avoiding concomitant use of thiotepa and strong CYP3A4 inhibitors. If concomitant use is unavoidable, monitor for adverse effects and decreased efficacy. Consider therapy modification
Ticagrelor: CYP3A4 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Ticagrelor. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ticagrelor. Avoid combination
Tofacitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tofacitinib. Management: Tofacitinib dose reductions are recommended when combined with strong CYP3A4 inhibitors. Recommended dose adjustments vary by tofacitinib formulation and therapeutic indication. See full monograph for details. Consider therapy modification
Tolterodine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tolterodine. Management: The maximum recommended adult dose of tolterodine is 2 mg/day when used together with a strong CYP3A4 inhibitor. Consider therapy modification
Tolvaptan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tolvaptan. Avoid combination
Toremifene: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Toremifene. Management: Use of toremifene with strong CYP3A4 inhibitors should be avoided if possible. If coadministration is necessary, monitor for increased toremifene toxicities, including QTc interval prolongation. Exceptions are discussed in separate monograph. Consider therapy modification
Trabectedin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Trabectedin. Avoid combination
TraMADol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of TraMADol. Monitor therapy
TraZODone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of TraZODone. Management: Consider the use of a lower trazodone dose and monitor for increased trazodone effects (eg, sedation, QTc prolongation) if combined with strong CYP3A4 inhibitors. Consider therapy modification
Triazolam: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Triazolam. Avoid combination
Ubrogepant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ubrogepant. Avoid combination
Udenafil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Udenafil. Avoid combination
Ulipristal: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ulipristal. Management: This is specific for when ulipristal is being used for signs/symptoms of uterine fibroids (Canadian indication). When ulipristal is used as an emergency contraceptive, patients receiving this combo should be monitored for ulipristal toxicity. Avoid combination
Upadacitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Upadacitinib. Monitor therapy
Valbenazine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Valbenazine. Management: Reduce the valbenazine dose to 40 mg daily when combined with strong CYP3A4 inhibitors. Consider therapy modification
Vardenafil: Posaconazole may increase the serum concentration of Vardenafil. Management: Limit vardenafil dosing to a maximum of 2.5 mg per 24 hours in patients receiving concurrent therapy with strong CYP3A4 inhibitors, such as posaconazole. Consider therapy modification
Vemurafenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vemurafenib. Management: Avoid concurrent use of vemurafenib with strong CYP3A4 inhibitors when possible. Consider use of an alternative that is not a strong inhibitor of CYP3A4 as clinically appropriate. Consider therapy modification
Venetoclax: Posaconazole may increase the serum concentration of Venetoclax. Management: This combination is contraindicated during venetoclax initiation and ramp-up in patients with CLL/SLL. Reduced venetoclax doses are required during ramp-up for patients with AML, and reduced doses are required for all patients during maintenance therapy. Consider therapy modification
Vilanterol: May increase the serum concentration of CYP3A4 Inhibitors (Strong). Monitor therapy
Vilazodone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vilazodone. Management: Limit maximum adult vilazodone dose to 20 mg daily in patients receiving strong CYP3A4 inhibitors. The original vilazodone dose can be resumed following discontinuation of the strong CYP3A4 inhibitor. Consider therapy modification
VinCRIStine (Liposomal): CYP3A4 Inhibitors (Strong) may increase the serum concentration of VinCRIStine (Liposomal). Avoid combination
Vinflunine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vinflunine. Avoid combination
Vitamin K Antagonists (eg, warfarin): Posaconazole may increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Vorapaxar: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vorapaxar. Avoid combination
Voxelotor: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Voxelotor. Management: Avoid concomitant use of voxelotor and strong CYP3A4 inhibitors. If concomitant use is unavoidable, reduce the voxelotor dose to 1,000 mg once daily. Consider therapy modification
Zanubrutinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Zanubrutinib. Management: Decrease the zanubrutinib dose to 80 mg once daily during coadministration with a strong CYP3A4 inhibitor. Further dose adjustments may be required for zanubrutinib toxicities, refer to prescribing information for details. Consider therapy modification
Zolpidem: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Zolpidem. Monitor therapy
Zopiclone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Zopiclone. Management: The initial starting adult dose of zopiclone should not exceed 3.75 mg if combined with a strong CYP3A4 inhibitor. Monitor patients for signs and symptoms of zopiclone toxicity if these agents are combined. Consider therapy modification
Zuclopenthixol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Zuclopenthixol. Management: Consider zuclopenthixol dosage reduction with concomitant use of a strong CYP3A4 inhibitor (eg, ketoconazole) in poor CYP2D6 metabolizers or with strong CYP2D6 inhibitors (eg, paroxetine). Monitor for increased zuclopenthixol levels/toxicity. Consider therapy modification
Adverse Reactions
>10%:
Cardiovascular: Thrombophlebitis (intravenous via peripheral venous catheter: 60%), hypertension (8% to 18%), peripheral edema (12% to 16%), lower extremity edema (oral: 15%), hypotension (oral: 14%), tachycardia (oral: 12%)
Central nervous system: Headache (8% to 28%), rigors (oral: ≤20%), fatigue (3% to 17%), insomnia (oral: 1% to 17%), chills (10% to 16%), dizziness (oral: 11%)
Dermatologic: Skin rash (3% to 24%), pruritus (oral: 11%)
Endocrine & metabolic: Hypokalemia (oral: ≤30%), hypomagnesemia (10% to 18%), hyperglycemia (oral: 11%)
Gastrointestinal: Diarrhea (10% to 42%), nausea (9% to 38%), vomiting (7% to 29%), abdominal pain (5% to 27%), constipation (8% to 21%), anorexia (oral: 2% to 15%), stomatitis (oral: 14%), decreased appetite (10% to 12%), upper abdominal pain (6% to 11%)
Hematologic & oncologic: Thrombocytopenia (≤29%), anemia (2% to 25%), neutropenia (oral: 4% to 23%), petechia (8% to 11%)
Hepatic: Increased serum alanine aminotransferase (oral: ≤17%)
Neuromuscular & skeletal: Musculoskeletal pain (oral: 16%), arthralgia (oral: 11%)
Respiratory: Cough (3% to 24%), dyspnea (1% to 20%), epistaxis (14% to 17%), pharyngitis (oral: 12%)
Miscellaneous: Fever (21% to 45%)
1% to 10%:
Cardiovascular: Edema (oral: 9%), pulmonary embolism (<5%), torsades de pointes (<5%)
Central nervous system: Paresthesia (<5%), pain (oral: 1%)
Dermatologic: Diaphoresis (oral: 2%)
Endocrine & metabolic: Hypocalcemia (9%), adrenocortical insufficiency (<5%), dehydration (oral: 1%), weight loss (oral: 1%)
Gastrointestinal: Dyspepsia (10%), pancreatitis (<5%), oral candidiasis (oral: 1%)
Genitourinary: Vaginal hemorrhage (oral: 10%)
Hematologic & oncologic: Hemolytic-uremic syndrome (<5%), thrombotic thrombocytopenic purpura (<5%)
Hepatic: Hyperbilirubinemia (≤10%), hepatic insufficiency (<5%), hepatitis (<5%), hepatomegaly (<5%), increased liver enzymes (<5%), jaundice (<5%), increased serum aspartate aminotransferase (≤4%), increased serum alkaline phosphatase (oral: ≤3%)
Hypersensitivity: Hypersensitivity reaction (<5%)
Infection: Herpes simplex infection (oral: 3%)
Neuromuscular & skeletal: Back pain (oral: 10%), asthenia (oral: 2% to 10%)
Renal: Acute renal failure (<5%)
Respiratory: Pneumonia (oral: 3%)
<1%, postmarketing, and/or case reports: Cholestasis, prolonged QT interval on ECG, pseudoaldosteronism
Warnings/Precautions
Concerns related to adverse effects:
- Hepatic effects: Hepatic dysfunction has occurred, ranging from mild/moderate increases of ALT, AST, alkaline phosphatase, total bilirubin, and/or clinical hepatitis to severe reactions (cholestasis, hepatic failure including death). Elevations in liver function tests have been generally reversible after posaconazole has been discontinued; some cases resolved without drug interruption. More severe reactions have been observed in patients with underlying serious medical conditions (eg, hematologic malignancy) and primarily with suspension total daily doses of 800 mg. Monitor liver function tests at baseline and periodically during therapy. If increases occur, monitor for severe hepatic injury development. Consider discontinuation of therapy in patients who develop clinical evidence of liver disease that may be secondary to posaconazole.
Disease-related concerns:
- Arrhythmias: Use caution in patients with an increased risk of arrhythmia (long QT syndrome, concurrent QTc-prolonging drugs metabolized through CYP3A4, hypokalemia). Development of QTc prolongation, including torsades de pointes, has been reported.
- Electrolyte abnormalities: Correct electrolyte abnormalities (eg, hypokalemia, hypomagnesemia, hypocalcemia) prior to initiating and during therapy.
- Renal impairment: Do not use injection in patients with eGFR <50 mL/minute/1.73 m2, unless risk/benefit has been assessed. See "Dosage forms specific issues: Injection formulation." Evaluate renal function (particularly serum creatinine) at baseline and periodically during therapy. If increases occur, consider oral therapy. Monitor closely for breakthrough fungal infections in patients with severe renal impairment taking delayed-release tablets or oral suspension due to variability in posaconazole exposure.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer's labeling.
- Injection formulation: Do not give as an intravenous bolus injection. Avoid/limit use of IV formulation in patients with eGFR <50 mL/minute/1.73 m2; injection contains excipient cyclodextrin (sulfobutyl ether beta-cyclodextrin [SBECD]), which may accumulate although the clinical significance of this finding is uncertain (Luke 2010); consider using oral posaconazole in these patients unless benefit of injection outweighs the risk. If injection is used in patients with eGFR <50 mL/minute, monitor serum creatinine closely; if increases occur, consider changing therapy to oral posaconazole. In critically patients undergoing concurrent continuous venovenous hemofiltration (CVVH), the use of standard doses of intravenous posaconazole has been used without SBECD accumulation (Morris 2015).
- Oral formulations: The delayed-release tablet and oral suspension are not to be used interchangeably due to dosing differences for each formulation.
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer's labeling.
Special populations:
- Obesity: Patients weighing >120 kg may have lower plasma drug exposure; monitor closely for breakthrough fungal infections.
Other warnings/precautions:
- Appropriate use: For patients prescribed posaconazole suspension who are unable to eat, take with a high-fat meal, or tolerate nutritional supplements or acidic carbonated beverages (eg, ginger ale), and do not have the option of taking the delayed-release tablet or injection, consider alternative antifungal therapy or closely monitor for breakthrough fungal infections.
Monitoring Parameters
Hepatic function (eg, AST/ALT, alkaline phosphatase and bilirubin) prior to initiation and during treatment; renal function, especially in patients on IV therapy if eGFR <50 mL/minute/1.73 m2; serum electrolytes (eg, calcium, magnesium, potassium) prior to initiation and during therapy; CBC; breakthrough fungal infections; adequate oral intake
For invasive aspergillosis (treatment or prolonged prophylaxis), IDSA recommends monitoring serum trough concentrations in patients receiving posaconazole oral suspension; further studies are needed to address whether therapeutic drug monitoring is helpful or necessary with delayed-release tablets or IV formulations of posaconazole (IDSA [Patterson 2016]). In general, evidence to support therapeutic drug monitoring for posaconazole is limited; however, due to the large interindividual and intraindividual variation in bioavailability and drug-drug interactions with posaconazole, therapeutic drug monitoring is advised (Dekkers 2016).
Pregnancy
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies.
Patient Education
What is this drug used for?
- It is used to treat fungal infections.
- It is used to prevent fungal infections
Frequently reported side effects of this drug
- Abdominal pain
- Constipation
- Cough
- Lack of appetite
- Joint pain
- Back pain
- Trouble sleeping
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, seizures, lack of appetite, or severe nausea or vomiting
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
- Abnormal heartbeat
- Chest pain
- Fast heartbeat
- Severe dizziness
- Passing out
- Vision changes
- Severe diarrhea
- Severe nausea
- Severe vomiting
- Shortness of breath
- Swelling of arms or legs
- Chills
- Sore throat
- Severe headache
- Nosebleed
- Bruising
- Bleeding
- Abnormal vaginal bleeding
- Severe loss of strength and energy
- Mouth irritation
- Mouth sores
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.