Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule Extended Release, Oral:
Klor-Con Sprinkle: 8 mEq [contains brilliant blue fcf (fd&c blue #1)]
Klor-Con Sprinkle: 10 mEq [contains fd&c red #40, fd&c yellow #10 (quinoline yellow)]
Micro-K: 8 mEq [DSC], 10 mEq [DSC]
Generic: 8 mEq, 10 mEq
Packet, Oral:
Klor-Con: 20 mEq (1 ea, 30 ea, 100 ea) [contains fd&c yellow #6 (sunset yellow); orange flavor]
Klor-Con: 20 mEq (1 ea [DSC], 30 ea [DSC], 100 ea [DSC]); 25 mEq (30 ea [DSC], 100 ea [DSC]) [sugar free; contains fd&c yellow #6 (sunset yellow); fruit flavor]
Generic: 20 mEq (1 ea, 30 ea, 100 ea)
Solution, Intravenous:
Potassium Chloride PROAMP: 2 mEq/mL (10 mL [DSC])
Generic: 20 mEq (1000 mL); 40 mEq (1000 mL); 0.4 mEq/mL (50 mL [DSC]); 10 mEq/100 mL (100 mL); 10 mEq/50 mL (50 mL); 20 mEq/100 mL (100 mL); 20 mEq/50 mL (50 mL); 40 mEq/100 mL (100 mL); 2 mEq/mL (5 mL, 10 mL, 20 mL, 30 mL, 250 mL); 20 mEq/L (1000 mL); 40 mEq/L (1000 mL [DSC]); Potassium 10 mEq/L, dextrose 5%, and sodium chloride 0.45% (1000 mL); Potassium 20 mEq/L and sodium chloride 0.45% (1000 mL); Potassium 20 mEq/L and sodium chloride 0.9% (1000 mL); Potassium 20 mEq/L, dextrose 5%, and sodium chloride 0.2% (500 mL, 1000 mL); Potassium 20 mEq/L, dextrose 5%, and sodium chloride 0.225% (500 mL, 1000 mL); Potassium 20 mEq/L, dextrose 5%, and sodium chloride 0.33% (500 mL [DSC], 1000 mL); Potassium 20 mEq/L, dextrose 5%, and sodium chloride 0.45% (500 mL, 1000 mL); Potassium 20 mEq/L, dextrose 5%, and sodium chloride 0.9% (1000 mL); Potassium 30 mEq/L, dextrose 5%, and sodium chloride 0.45% (1000 mL); Potassium 40 mEq/L and sodium chloride 0.9% (1000 mL); Potassium 40 mEq/L, dextrose 5%, and sodium chloride 0.45% (1000 mL); Potassium 40 mEq/L, dextrose 5%, and sodium chloride 0.9% (1000 mL)
Solution, Intravenous [preservative free]:
Generic: 10 mEq/100 mL (100 mL); 10 mEq/50 mL (50 mL); 20 mEq/50 mL (50 mL); 20 mEq/L (1000 mL)
Solution, Oral:
Generic: 20 mEq/15 mL (10%) (15 mL, 30 mL, 473 mL, 3800 mL); 40 MEQ/15ML (20%) (473 mL); 40 mEq/15 mL (20%) (473 mL)
Tablet Extended Release, Oral:
K-Tab: 8 mEq, 10 mEq [contains fd&c yellow #10 (quinoline yellow)]
K-Tab: 20 mEq
Klor-Con: 8 mEq [contains fd&c blue #1 aluminum lake, fd&c blue #2 aluminum lake]
Klor-Con 10: 10 mEq [contains fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Klor-Con M10: 10 mEq
Klor-Con M15: 15 mEq
Klor-Con M15: 15 mEq [scored]
Klor-Con M20: 20 mEq
Klor-Con M20: 20 mEq [scored]
Generic: 8 mEq, 10 mEq, 20 mEq
Pharmacology
Mechanism of Action
Potassium is the major cation of intracellular fluid and is essential for the conduction of nerve impulses in heart, brain, and skeletal muscle; contraction of cardiac, skeletal and smooth muscles; maintenance of normal renal function, acid-base balance, carbohydrate metabolism, and gastric secretion
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed from upper GI tract
Distribution
Enters cells via active transport from extracellular fluid
Excretion
Primarily urine; skin and feces (small amounts); most intestinal potassium reabsorbed
Use: Labeled Indications
Hypokalemia: Treatment or prevention of hypokalemia.
Contraindications
Hypersensitivity to potassium chloride or any component of the formulation; hyperkalemia, renal failure, and conditions in which potassium retention is present; structural, pathological, and/or pharmacologic cause for delay or arrest in passage through the GI tract (solid oral dosage forms only).
Canadian labeling: Additional contraindications (not in US labeling): Injection: Renal impairment with oliguria, anuria, or azotemia; Addison disease (untreated); ventricular fibrillation; salt-losing adrenal hyperplasia; extensive tissue breakdown as in severe burns, acute dehydration, and heat cramps; increased sensitivity to potassium administration (eg, congenital paramyotonia, adynamia episodica hereditaria); hyperadrenalism associated with adrenogenital syndrome; digitalis-induced, second- or third-degree heart block.
Dosage and Administration
Dosing: Adult
Note: When maintaining normal daily requirements, IV doses should be incorporated into the patient's maintenance IV fluids. Intermittent IV potassium administration should be reserved for more severe depletion situations in patients undergoing ECG monitoring. Doses expressed as mEq of potassium.
Normal daily requirements: Oral, IV: 40 to 80 mEq/day
Prevention of hypokalemia: Oral: 20 to 40 mEq/day in 1 to 2 divided doses
Treatment of hypokalemia:
Oral:
Mild to moderate hypokalemia: Note: If deficits are severe or ongoing losses are great, IV route should be considered.
Capsules, tablets, oral solution: Usual dose: 40 to 100 mEq daily in divided doses; limit single doses to 20 to 25 mEq/dose to avoid GI discomfort.
Powder for oral solution (Klor-Con): Usual dose: 40 to 100 mEq daily in 2 to 5 divided doses; limit single doses to 40 mEq/dose; maximum: 200 mEq/24 hours.
Note: Some clinicians initiate treatment with 10 to 20 mEq given 2 to 4 times per day (20 to 80 mEq/day), depending upon the severity of the hypokalemia. Total daily doses up to 120 mEq may be necessary as determined by laboratory assessment, patient symptoms and/or ongoing losses (Brophy 2014).
Severe hypokalemia: Some clinicians initiate treatment with 40 mEq given 3 to 4 times per day; may also administer 20 mEq every 2 to 3 hours in conjunction with IV potassium administration with careful monitoring. Administration of dose >40 mEq orally per dose are typically not well tolerated, resulting in GI irritation and nausea.
IV intermittent infusion: Peripheral or central line: ≤10 mEq/hour; repeat as needed based on frequently obtained lab values; central line infusion and continuous ECG monitoring highly recommended for infusions >10 mEq/hour.
Potassium dosage/rate of infusion general guidelines (per product labeling): Note: High variability exists in dosing/infusion rate recommendations; therapy guided by patient condition and specific institutional guidelines. As an estimate, 10 mEq of potassium chloride will roughly increase serum levels by 0.1 mEq/L. Patients with more severe forms of hypokalemia (eg, serum potassium levels <3.5 mEq/L) may require increased amounts due to total body potassium deficit (Flurie 2017).
Serum potassium >2.5 to 3.5 mEq/L: Maximum infusion rate: 10 mEq/hour; maximum concentration: 40 mEq/L; maximum 24-hour dose: 200 mEq
Serum potassium <2.5 mEq/L or symptomatic hypokalemia (excluding emergency treatment of cardiac arrest): Maximum infusion rate (central line only): 40 mEq/hour in presence of continuous ECG monitoring and frequent lab monitoring; in selected situations, patients may require up to 400 mEq/24 hours.
Dosing: Geriatric
Refer to adult dosing. Use with caution, starting at the low end of the dosage range.
Dosing: Pediatric
Note: Maintenance potassium IV doses should be incorporated into the patient's maintenance IV fluids; intermittent IV potassium administration should be reserved for severe depletion situations; continuous ECG monitoring should be used for intermittent IV doses >0.5 mEq/kg/hour. Oral solutions are available in two concentrations: 20 mEq/15 mL (1.33 mEq/mL) and 40 mEq/15 mL (2.67 mEq/mL); use extra precaution; verify product formulation for dosage calculation.
Hypokalemia, prevention for ongoing drug losses (eg, concurrent diuretic therapy): Limited data available: Infants, Children, and Adolescents: Oral: 1 to 2 mEq/kg/day in 1 to 2 divided doses; usual single dose should not exceed usual adult single dose: 20 mEq/dose; although some patients may require a single dose up to 40 mEq/dose (Moffett 2011); some patients may require higher individual daily doses based on lab values and ongoing losses.
Hypokalemia, treatment; mild to moderate: Limited data available: Infants, Children, and Adolescents: Oral: 2 to 5 mEq/kg/day in divided doses; not to exceed 1 to 2 mEq/kg as a single dose or 20 mEq (whichever is less) (ASPEN [Corkins 2015]; Moffett 2011); if deficits are severe or ongoing losses are great, IV potassium route should be considered as preferred route of administration.
Hypokalemia, treatment; severe: Infants, Children, and Adolescents: Intermittent IV infusion: 0.5 to 1 mEq/kg/dose; maximum dose: 40 mEq/dose; infuse at a rate ≤0.5 mEq/kg/hour (see Administration for more detail on rate) (ASPEN [Corkins 2015]; Fuhrman 2017; Kliegman 2016); serum concentrations should be evaluated 1 to 2 hours after completion of infusion; may repeat as needed based on lab values; severe depletion or ongoing losses may require >200% of normal daily maintenance (Knudson 2013).
Parenteral nutrition, maintenance potassium requirement (ASPEN [Mirtallo 2004]):
Infants and Children weighing ≤50 kg: IV: 2 to 4 mEq/kg/day of potassium as an additive to parenteral nutrition solution.
Children weighing >50 kg and Adolescents: IV: 1 to 2 mEq/kg/day of potassium as an additive to parenteral nutrition solution.
Reconstitution
Parenteral: Potassium must be diluted prior to parenteral administration. The concentration of infusion may be dependent on patient condition and specific institution policy. Some clinicians recommend that the maximum concentration for peripheral infusion is 10 mEq/100 mL and 20-40 mEq/100 mL for central infusions.
Administration
Parenteral: Potassium must be diluted prior to parenteral administration. For IV infusion; do not administer IV push. In general, the rate of administration may be dependent on patient condition and specific institution policy.
Some clinicians recommend that the maximum concentration for peripheral infusion is 10 mEq/100 mL and maximum rate of administration for peripheral infusion is 10 mEq/hour (Kraft 2005). ECG monitoring is recommended for peripheral or central infusions >10 mEq/hour in adults (Kraft 2005). With central line administration, higher concentrations and more rapid rates of infusion may be used; concentrations of 20 to 40 mEq/100 mL at a maximum rate of 40 mEq/hour via central line have been safely administered (Hamill 1991; Kruse 1990).
Vesicant/irritant (at concentrations >0.1 mEq/mL); ensure proper needle or catheter placement prior to and during IV infusion. Avoid extravasation.
Extravasation management: If extravasation occurs, stop infusion immediately and disconnect (leave needle/cannula in place); gently aspirate extravasated solution (do NOT flush the line); initiate hyaluronidase antidote; remove needle/cannula; apply dry cold compresses (Hurst 2004; Reynolds 2014); elevate extremity.
Hyaluronidase: Intradermal or SubQ: Inject a total of 1 to 1.7 mL (15 units/mL) as five separate 0.2 to 0.3 mL injections (using a 25-gauge needle) into area of extravasation at the leading edge in a clockwise manner (MacCara 1983; Reynolds 2014; Zenk 1981).
Oral: Oral dosage forms should be taken with meals (or immediately after eating) and a full glass of water or other liquid to minimize the risk of GI irritation. Prescribing information for the various oral preparations recommend that no more than 20 mEq to 40 mEq should be given as single dose.
Capsule: MicroK: Swallow whole, do not chew. Capsules may also be opened and contents sprinkled on a spoonful of applesauce or pudding and should be swallowed immediately without chewing.
Powder for oral solution: Klor-Con: Dissolve one packet in at least 120 mL of cold water or other beverage prior to administration. If GI irritation occurs, increase dilution.
Tablet:
K-Tab, Kaon-Cl, Klor-Con: Swallow tablets whole; do not crush, chew, or suck on tablet.
Klor-Con M: Swallow tablets whole; do not crush, chew, or suck on tablet. Tablet may also be broken in half and each half swallowed separately; the whole tablet may be dissolved in ~4 ounces of water (allow ~2 minutes to dissolve, stir well and drink immediately)
Dietary Considerations
Administer with plenty of fluid to decrease stomach irritation and discomfort. Some dietary sources of potassium include leafy green vegetables (eg, spinach, cabbage), tomatoes, cucumbers, zucchini, fruits (eg, apples, oranges, and bananas), root vegetables (eg, carrots, radishes), beans, and peas.
Storage
Capsule, tablet: Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light and moisture.
Powder for oral solution: Store at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C to 30°C (59°F to 86°F). Protect from light.
Solution for injection: Store at 25°C (77°F); do not freeze; avoid excessive heat. Use only clear solutions. Potassium chloride is compatible when admixed in most common infusion solutions. Refer to institution-specific policies and procedures for stability information.
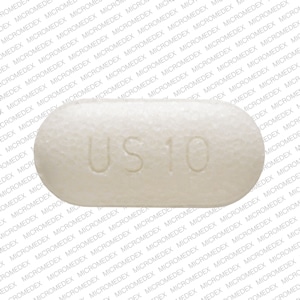
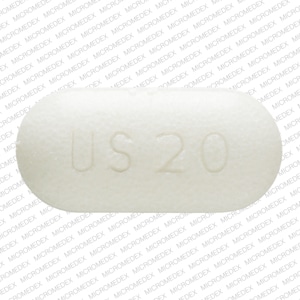
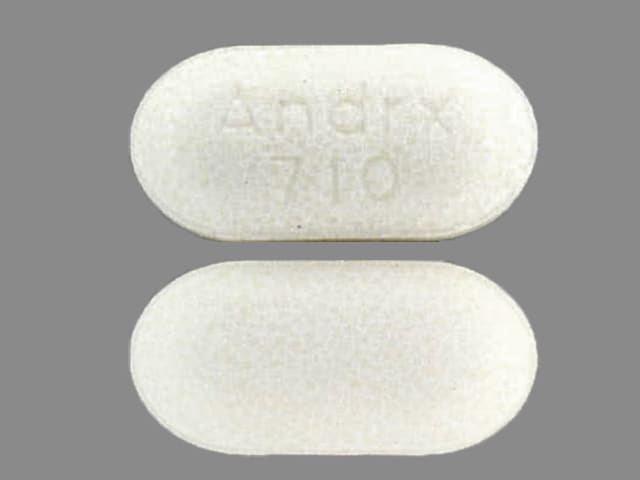
Potassium Chloride Images
Drug Interactions
Aliskiren: Potassium Salts may enhance the hyperkalemic effect of Aliskiren. Monitor therapy
Angiotensin II Receptor Blockers: Potassium Salts may enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Potassium Salts may enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Anticholinergic Agents: May enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Drospirenone: Potassium Salts may enhance the hyperkalemic effect of Drospirenone. Monitor therapy
Eplerenone: May enhance the hyperkalemic effect of Potassium Salts. Management: This combination is contraindicated in patients receiving eplerenone for treatment of hypertension. Consider therapy modification
Glycopyrrolate (Systemic): May enhance the adverse/toxic effect of Potassium Chloride. This is specific to solid oral dosage forms of potassium chloride. Avoid combination
Heparin: May enhance the hyperkalemic effect of Potassium Salts. Monitor therapy
Heparins (Low Molecular Weight): May enhance the hyperkalemic effect of Potassium Salts. Monitor therapy
Nicorandil: May enhance the hyperkalemic effect of Potassium Salts. Monitor therapy
Potassium-Sparing Diuretics: Potassium Salts may enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Consider therapy modification
Adverse Reactions
Frequency not defined:
Cardiovascular: Cardiac arrhythmia, cardiac conduction disturbance, edema, peripheral edema
Endocrine & metabolic: Fluid and electrolyte disturbance, hypervolemia
Gastrointestinal: Abdominal cramps, abdominal distress, abdominal pain, diarrhea, flatulence, gastrointestinal hemorrhage, gastrointestinal irritation, gastrointestinal obstruction, gastrointestinal perforation, gastrointestinal ulcer, nausea, vomiting
Respiratory: Pulmonary edema
Postmarketing: Angioedema, asystole (with rapid administration or hyperkalemia), bradycardia, burning sensation at injection site, chest pain, dyspnea, encephalopathy (hyponatremic), erythema at injection site, hyperkalemia, hypersensitivity reaction, hyponatremia, infusion-site pain, injection site phlebitis, irritation at injection site, skin rash, swelling at injection site, venous thrombosis at injection site, ventricular fibrillation (with rapid administration or hyperkalemia)
Warnings/Precautions
Concerns related to adverse effects:
- Extravasation: Vesicant/irritant (at concentrations >0.1 mEq/mL); ensure proper catheter or needle position prior to and during infusion. Avoid extravasation.
- Hyperkalemia: May occur with IV or oral use. Potentially fatal hyperkalemia can develop rapidly and be asymptomatic. Use with caution or avoid use in patients with predisposing conditions for hyperkalemia (eg, chronic or severe renal impairment, extensive burns or tissue injury, heart failure, acute dehydration, systemic acidosis, adrenal insufficiency, or the administration of potassium-sparing diuretics). Monitor serum potassium closely.
- Hypersensitivity/infusion reactions: Hypersensitivity/infusion reactions, including anaphylaxis and chills, may occur with parenteral administration of potassium containing solutions. Discontinue immediately if signs/symptoms of hypersensitivity/infusion reactions develop.
- Hyponatremia: Parenteral administration may cause hyponatremia; risk may be increased in children, elderly patients, postoperatively, in patients with psychogenic polydipsia, and with concurrent use of medications that may decrease sodium (eg, diuretics). Monitor serum sodium as clinically indicated.
Disease-related concerns:
- Acid/base disorders: Use with caution in patients with acid/base alterations or acid/base correction; hyperosmolality or acidosis (or correction of alkalosis) is associated with hyperkalemia (shift of intracellular potassium to extracellular space); monitor serum potassium closely.
- Cardiovascular disease: Use with caution in patients with cardiovascular disease (eg, heart failure, cardiac arrhythmias, atrioventricular [AV] block); patients may be more susceptible to life-threatening cardiac effects associated with hyper/hypokalemia.
- Hepatic impairment: Use with caution in patients with cirrhosis; monitor serum potassium more frequently.
- Renal impairment: Use with caution in patients with renal impairment; monitor serum potassium closely. Contraindicated in patients with renal failure.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Oral formulations: May cause GI upset and irritation (eg, nausea, vomiting, diarrhea, abdominal pain, discomfort) and lead to GI ulceration, bleeding, perforation, and/or obstruction. Oral liquid preparations (not solid) should be used in patients with esophageal compression or delayed gastric emptying. Extended-release formulations of potassium chloride may result in a “ghost tablet” in the stool.
Other warnings/precautions:
- Parenteral administration: Use extreme caution with parenteral administration and monitor serum potassium concentrations closely. Evaluate renal function, cardiac and fluid status, and any factors contributing to altered potassium concentrations (eg, acidosis, alkalosis) prior to therapy. Do NOT administer undiluted or IV push; inappropriate parenteral administration may be fatal. Always administer potassium further diluted; refer to appropriate dilution and administration rate recommendations. Pain and phlebitis may occur during parenteral infusion requiring a decrease in infusion rate or potassium concentration.
Monitoring Parameters
Electrolytes (including serum potassium, calcium, chloride, magnesium, phosphate, sodium), acid/base balance; renal function; cardiac monitor (if intermittent infusion or potassium infusion rates 0.5 mEq/kg/hour in children or >10 mEq/hour in adults); to assess adequate replacement, repeat serum potassium level 2 to 4 hours after dose; monitor potassium levels daily for treatment and monthly to biannually for prophylaxis. Monitor IV infusion site.
Pregnancy
Pregnancy Considerations
Potassium requirements are the same in pregnant and nonpregnant women. Adverse events have not been observed following use of potassium supplements in healthy women with normal pregnancies. Use caution in pregnant women with other medical conditions (eg, preeclampsia; may be more likely to develop hyperkalemia) (IOM 2004). Potassium supplementation (that does not cause maternal hyperkalemia) would not be expected to cause adverse fetal events.
Patient Education
What is this drug used for?
- It is used to treat or prevent low potassium levels.
Frequently reported side effects of this drug
- Abdominal pain
- Nausea
- Vomiting
- Diarrhea
- Passing gas
- Tablet wax in stool
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- High potassium like abnormal heartbeat, confusion, dizziness, passing out, weakness, shortness of breath, or numbness or tingling feeling
- Slow heartbeat
- Chest pain
- Low sodium like headache, difficulty focusing, trouble with memory, confusion, weakness, seizures, or change in balance
- Bowel problems like black, tarry, or bloody stools; fever; mucus in stools; vomiting; vomiting blood; severe abdominal pain; constipation; or diarrhea
- Abdominal swelling
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Severe injection site pain, edema, or irritation
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.