Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
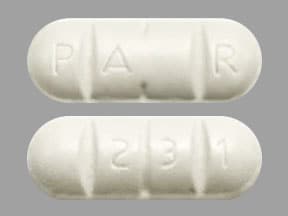
Tablet, Oral:
Biltricide: 600 mg [scored]
Generic: 600 mg
Pharmacology
Mechanism of Action
Increases the cell permeability to calcium in schistosomes, causing strong contractions and paralysis of worm musculature leading to detachment of suckers from the blood vessel walls and to dislodgment
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: 80%
Distribution
CSF concentration is 14% to 20% of plasma concentration
Metabolism
Extensive first-pass effect; metabolized by the liver to hydroxylated and conjugated metabolites
Excretion
Urine ~80% (>99% as metabolites)
Time to Peak
Serum: 1 to 3 hours
Half-Life Elimination
Parent drug: 0.8 to 1.5 hours; Metabolites: 4.5 hours
Protein Binding
~80%
Use in Specific Populations
Special Populations: Renal Function Impairment
Excretion may be delayed in patients with renal impairment, but accumulation of unchanged drug would not be expected.
Special Populations: Hepatic Function Impairment
Cmax, AUC, and half-life were significantly elevated in patients with moderate to severe liver impairment.
Use: Labeled Indications
Helminths: Treatment of infections in patients ≥1 year caused by the following: All species of Schistosoma (eg, Schistosoma mekongi, S. japonicum, S. mansoni, S. hematobium) and the liver flukes Clonorchis sinensis/Opisthorchis viverrini
Use: Off Label
Neurocysticercosis, parenchymalbyes
Data from the phase II and phase III portions of a randomized, double blind, placebo-controlled study supports the use of praziquantel (in combination with albendazole) in the treatment of parenchymal neurocysticercosis Garcia 2014, Garcia 2016.
Based on the IDSA/ASTMH guidelines for the diagnosis and treatment of neurocysticercosis, praziquantel, in combination with albendazole, is an effective and recommended agent in the management of parenchymal neurocysticercosis with >2 viable cysts.
Tapewormsc
Clinical experience suggests the utility of praziquantel in the treatment of a broad range of trematode and cestode infections Liu 1996.
Contraindications
Hypersensitivity to praziquantel or any component of the formulation; ocular cysticercosis; concomitant administration with strong cytochrome P450 (CYP450) inducers, such as rifampin
Dosage and Administration
Dosing: Adult
Schistosomiasis: Oral: 20 mg/kg/dose 3 times daily at 4- to 6-hour intervals for 1 day
Clonorchiasis/opisthorchiasis: Oral: 25 mg/kg/dose 3 times daily for 1 to 2 days (Drugs for Parasitic Infections 2013; manufacturer's labeling)
Neurocysticercosis, parenchymal (>2 viable cysts) (off-label use): Oral: 50 mg/kg/day in 3 divided doses (in combination with albendazole) for 10 to 14 days; may be repeated if persistent viable lesions on 6-month follow-up imaging (Garcia 2014; IDSA/ASTMH [White 2018]). Note: Initiate adjunctive corticosteroid therapy prior to initiation of antiparasitic therapy. Antiparasitic therapy should not be initiated in patients with untreated hydrocephalus, calcified lesions, or cysticercal encephalitis; consult an infectious diseases specialist for specific treatment recommendations (IDSA/ASTMH [White 2018]).
Tapeworms (off-label use): Oral: 5 to 10 mg/kg as a single dose (25 mg/kg for Hymenolepis nana) (Drugs for Parasitic Infections 2013; Liu 1996)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dosing interval and duration highly variable dependent on condition; for 3 times daily doses, intervals of 4 to 6 hours are suggested.
Flukes:
Clonorchiasis (Clonorchis sinensis [Chinese liver fluke]); Opisthorchiasis (Opisthorchis viverrini [Southeast Asian liver fluke]): Children and Adolescents: Oral: 25 mg/kg/dose 3 times daily at 4- to 6-hour intervals for 1 to 2 days (CDC 2018a; CDC 2018b; Red Book [AAP 2018])
Fasciolopsiasis (Fasciolopsis buski [intestinal fluke]):Limited data available: Children and Adolescents: Oral: 25 mg/kg/dose 3 times daily for 1 day (CDC 2012b; Red Book [AAP 2018])
Paragonimiasis (Paragonimus spp. [lung fluke]): Limited data available: Children and Adolescents: Oral: 25 mg/kg/dose 3 times daily for 2 to 3 days (CDC 2013a; Red Book [AAP 2018])
Schistosomiasis (Bilharziasis):
Treatment (CDC 2018c; Red Book [AAP 2018]): Note: Repeat treatment may be needed in 2 to 4 weeks to increase effectiveness
Schistosoma japonicum, Schistosoma mekongi: Children and Adolescents: Oral: 20 mg/kg/dose 3 times daily for 1 day
Schistosoma mansoni, Schistosoma haematobium, Schistosoma intercalatum: Children and Adolescents: Oral: 20 mg/kg/dose twice daily for 1 day
Control programs for endemic areas: Limited data available: Infants, Children, and Adolescents: Oral: 40 mg/kg as a single dose (WHO 2006; WHO 2010); a single dose of 40 mg/kg has been successfully used to treat urogenital S. haematobium in children 1 to 10 years of age (Wami 2016) and S. mansoni in population that included infants (age range: 5 months to 7 years) (Sousa-Figueiredo 2012); however, pharmacokinetic data suggests a lower cure rate in infants and preschool children; one possible explanation is that higher doses may be necessary in younger patients due to pharmacokinetic/dynamic differences; in preschool children, a single dose of 60 mg/kg was successfully used in children 3 to 8 years of age in a hyperendemic area to treat S. mansoni (Bustinduy 2016).
Tapeworms: Limited data available:
Diphyllobothrium latum (fish), Taenia saginata (beef), Taenia solium (pork); intestinal (adult) stage: Children and Adolescents: Oral: 5 to 10 mg/kg as a single dose (CDC 2012a; CDC 2013b; Red Book [AAP 2018])
Dipylidium caninum (dog); intestinal (adult) stage: Infants ≥6 months, Children, and Adolescents: Oral: 5 to 10 mg/kg as a single dose (CDC 2016; Red Book [AAP 2018])
Hymenolepis nana (dwarf tapeworm): Children and Adolescents: Oral: 25 mg/kg as a single dose (CDC 2012c)
Neurocysticercosis (Taenia solium [pork tapeworm]); tissue (larvae) stage: Children and Adolescents: Oral: 50 mg/kg/day for 15 days (CDC 2017); Note: May be used in conjunction with antiseizure medication and/or corticosteroids.
Administration
Administer tablets with water during meals. Tablets should be promptly swallowed to avoid bitter taste that may cause gagging or vomiting. Tablets may be halved or quartered; do not chew. Tablets may be crushed or disintegrated and mixed with semi-solid food or liquid; use within 1 hour of mixing. Tablets are scored and may be split into four 150 mg segments.
Storage
Store below 30°C (86°F).
Praziquantel Images
Drug Interactions
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Chloroquine: May decrease the serum concentration of Praziquantel. Monitor therapy
Cimetidine: May increase the serum concentration of Praziquantel. Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Praziquantel. Management: Use of praziquantel with strong CYP3A4 inducers is contraindicated. Discontinue rifampin 4 weeks prior to initiation of praziquantel therapy. Rifampin may be resumed the day following praziquantel completion. Avoid combination
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Praziquantel. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Grapefruit Juice: May increase the serum concentration of Praziquantel. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Adverse Reactions
Frequency not defined. May be more frequent and/or serious in patients with a heavy worm burden.
Central nervous system: Dizziness, headache, malaise
Dermatologic: Urticaria
Gastrointestinal: Abdominal distress, nausea
Miscellaneous: Fever
<1%, postmarketing and/or case reports: Abdominal pain, anorexia, atrioventricular block, bloody diarrhea, bradycardia, cardiac arrhythmia, drowsiness, ectopic beats, eosinophilia, fatigue, hypersensitivity, hypersensitivity reaction, increased liver enzymes (minimal), myalgia, paradoxical reaction (in schistosomiasis), polyserositis, pruritus, seizure, serum sickness (in schistosomiasis; Jarisch-Herxheimer-like reaction), skin rash, ventricular fibrillation, vertigo, vomiting, weakness
Warnings/Precautions
Disease-related concerns:
- Cardiac arrhythmias: Monitor patients with cardiac arrhythmias during treatment; bradycardia, ectopic rhythms, ventricular fibrillation, and AV blocks have been observed with praziquantel administration.
- Central nervous system effects: Praziquantel may exacerbate central nervous system pathology due to schistosomiasis, paragonimiasis, or Taenia solium cysticercosis. Assess whether the potential benefit justifies the potential risk in patients with a history of seizures and/or other signs of potential central nervous system involvement such as subcutaneous nodules suggestive of cysticercosis.
- Hepatic impairment: Use with caution in patients with moderate to severe hepatic impairment; reduced liver drug metabolism may result in higher and longer lasting plasma concentrations of unmetabolized praziquantel.
- Neurocysticercosis: Appropriate use: Antiparasitic therapy may worsen symptoms of neurocysticercosis by inducing an inflammatory response; adjunctive corticosteroid therapy should be started before initiation of antiparasitic therapy. Antiparasitic therapy should not be initiated in patients with untreated hydrocephalus, calcified lesions, or cysticercal encephalitis. Perform funduscopic exam prior to initiation of antiparasitic therapy to exclude intraocular cysticerci; antiparasitic therapy may lead to blindness in some cases with unsuspected intraocular parasites (IDSA/ASTMH [White 2018]).
- Schistosomiasis: Praziquantel may not be effective against migrating schistosomulae; observational data indicate that praziquantel treatment in the acute phase of the infection may not prevent progression from asymptomatic to acute schistosomiasis, or from asymptomatic/acute disease to chronic disease. In addition, use in patients with schistosomiasis may be associated with clinical deterioration such as paradoxical reactions or serum sickness Jarisch-Herxheimer-like reactions, which is a sudden inflammatory immune response likely caused by the release of schistosomal antigens. Such reactions typically occur during the acute disease phase, and may lead to life-threatening events such as respiratory failure, encephalopathy, papilledema, and/or cerebral vasculitis.
Concurrent drug therapy issues:
- Drug/drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information. Therapeutic levels of praziquantel may not be achieved with concurrent administration of strong inducers of cytochrome P450 (eg, rifampin); concurrent use is contraindicated.
Other warnings/precautions:
- Patient information: Patients should be instructed to not drive or operate machinery on the day of treatment and the day after treatment.
Monitoring Parameters
Liver function tests; monitor patients with cardiac irregularities during treatment; monitor for seizures; culture urine or feces for ova prior to instituting therapy
Pregnancy
Pregnancy Considerations
Based on available data, an increased risk of adverse fetal or maternal outcomes has not been observed following use of praziquantel for the treatment of Schistosoma infection during pregnancy (Friedman 2018).
In areas where schistosomiasis and soil-transmitted helminthiasis is endemic, the World Health Organization recommends treatment with praziquantel during any trimester of pregnancy (WHO 2006). Non-emergent treatment of neurocysticercosis can be delayed until after pregnancy (IDSA/ASTMH [White 2018]).
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience loss of strength and energy, dizziness, headache, abdominal pain, or nausea. Have patient report immediately to prescriber seizures, fast heartbeat, slow heartbeat, or abnormal heartbeat (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.