Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral, as phosphate:
Generic: 26.3 mg
Pharmacology
Mechanism of Action
Primaquine is an antiprotozoal agent active against exoerythrocytic stages of Plasmodium ovale and P. vivax, also active against the primary exoerythrocytic stages of P. falciparum and gametocytes of Plasmodia; disrupts mitochondria and binds to DNA
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed
Metabolism
Hepatic to carboxyprimaquine (active) via CYP1A2
Excretion
Urine (small amounts as unchanged drug)
Time to Peak
Serum: 1 to 3 hours
Half-Life Elimination
7 hours; reported range: 3.7 to 9.6 hours
Use: Labeled Indications
Malaria: Radical cure (prevention of relapse) of vivax malaria
Use: Off Label
Malaria chemoprophylaxisyes
Based on the Centers for Disease Control and Prevention Health Information for National Travel, primaquine is effective and recommended for prophylaxis of malaria when the travel is of short-duration to areas with principally Plasmodium vivax malaria and last-minute travelers. Must rule out G6PD deficiency prior to use.
Pneumocystis pneumonia (PCP) in HIV-infected patientsyes
Based on the US Department of Health and Human Services (HHS) Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents, primaquine in combination with clindamycin is an effective and recommended alternative agent in the treatment of Pneumocystis pneumonia (PCP) in HIV-infected patients.
Presumptive antirelapse therapy for Plasmodium vivax and Plasmodium ovale malariayes
Based on the Centers for Disease Control and Prevention Health Information for National Travel, primaquine is effective and recommended for presumptive antirelapse therapy (terminal prophylaxis) to decrease the risk for relapses of P. vivax and Plasmodium ovale malaria. Must rule out G6PD deficiency prior to use.
Uncomplicated Plasmodium vivax and Plasmodium ovale malariayes
Based on the Centers for Disease Control and Prevention guidelines for treatment of malaria, primaquine is effective and recommended for the treatment of uncomplicated Plasmodium vivax or Plasmodium ovale malaria. Must rule out G6PD deficiency prior to use.
Contraindications
Severe G6PD deficiency; pregnancy; use in acutely ill patients who have a tendency to develop granulocytopenia (eg, rheumatoid arthritis, systemic lupus erythematosus); concurrent use with other medications causing hemolytic anemia or myeloid bone marrow suppression; concurrent use with or recent use of quinacrine
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to primaquine or any component of the formulation
Documentation of allergenic cross-reactivity for aminoquinolines is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Note: Screen for G6PD deficiency prior to initiating treatment. Dosage expressed as mg of base (15 mg base = 26.3 mg primaquine phosphate).
Malaria: Oral:
Treatment or prevention of relapse of P. vivax malaria: 15 mg once daily in combination with chloroquine for 14 days (maximum dose: 15 mg/day)
Treatment of uncomplicated P. vivax and P. ovale malaria (off-label use): 30 mg once daily for 14 days with chloroquine or hydroxychloroquine; alternative regimen (for mild G6PD deficiency or as an alternative to daily regimen): 45 mg once weekly for 8 weeks (use only after consultation with an infectious disease/tropical medicine expert) (CDC 2013)
Chemoprophylaxis (off-label use): 30 mg once daily; start 1 to 2 days prior to travel and continue for 7 days after departure from malaria-endemic area (CDC Yellow Book 2014)
Presumptive antirelapse therapy for P. vivax and P. ovale malaria (off-label use): 30 mg once daily for 14 days after departure from malaria-endemic area (CDC Yellow Book 2014)
Pneumocystis pneumonia (PCP) treatment in HIV-infected patients (alternative to preferred therapy) (off-label use): Oral: 30 mg once daily for 21 days (in combination with clindamycin) (HHS [OI adult 2015])
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dosage expressed as mg of base (15 mg base = 26.3 mg primaquine phosphate):
Malaria: Oral:
Treatment or relapse prevention of P. vivax malaria: Infants, Children, and Adolescents: 0.5 mg base/kg once daily for 14 days; maximum single dose: 30 mg base (CDC, 2013)
Treatment of uncomplicated malaria (P. vivax and P. ovale): Infants, Children, and Adolescents: 0.5 mg base/kg once daily for 14 days with chloroquine or hydroxychloroquine; maximum single dose: 30 mg base (CDC, 2013)
Prevention of malaria (primarily P. vivax):
Non-HIV-exposed/-positive: Infants, Children and Adolescents: 0.5 mg base/kg once daily; maximum single dose: 30 mg base; initiate 1 to 2 days prior to travel and continue once daily while in the area with malaria risk, and for 7 days after departure from malaria-endemic area (CDC, 2014)
HIV-exposed/-positive:
Primary prophylaxis: Infants and Children: 0.6 mg base/kg once daily; maximum single dose: 30 mg base; initiate 1 day prior to travel and continue once daily while in the area with malaria risk, and for 3 to 7 days after departure from malaria-endemic area (DHHS [pediatric], 2013)
Secondary prophylaxis and antirelapse therapy: Infants, Children, and Adolescents: 0.5 mg base/kg once daily for 14 days after departure from malaria-endemic area; maximum single dose: 30 mg base (CDC, 2014)
Pneumocystis jirovecii pneumonia (PCP) (HIV-exposed/-positive) treatment: Oral:
Infants and Children: 0.3 mg base/kg once daily for 21 days in combination with clindamycin; maximum single dose: 30 mg base (DHHS [pediatric], 2013)
Adolescents: 30 mg base once daily for 21 days in combination with clindamycin (DHHS [adult], 2013)
Extemporaneously Prepared
A 6 mg base/5 mL oral suspension may be made using tablets. Crush ten 15 mg base tablets and reduce to a fine powder. In small amounts, add a total of 10 mL Carboxymethylcellulose 1.5% and mix to a uniform paste; mix while adding Simple Syrup, NF to almost 125 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 125 mL. Label "shake well" and "refrigerate". Stable 7 days.
Nahata MC, Pai VB, and Hipple TF, Pediatric Drug Formulations, 5th ed, Cincinnati, OH: Harvey Whitney Books Co, 2004.
Administration
Administer with meals to decrease adverse GI effects. If patient vomits within 30 minutes of taking a dose, then they should repeat the dose (CDC 2013).
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light.
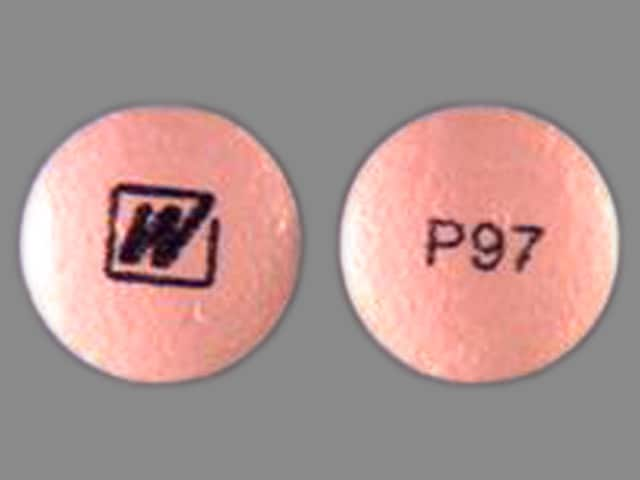
Primaquine Images
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Ajmaline: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Antipsychotic Agents (Phenothiazines): Antimalarial Agents may increase the serum concentration of Antipsychotic Agents (Phenothiazines). Monitor therapy
Artemether: May enhance the QTc-prolonging effect of Primaquine. Artemether may increase the serum concentration of Primaquine. Monitor therapy
Artesunate: May enhance the QTc-prolonging effect of Primaquine. Artesunate may increase the serum concentration of Primaquine. Monitor therapy
Asunaprevir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Beta-Blockers: Aminoquinolines (Antimalarial) may decrease the metabolism of Beta-Blockers. Exceptions: Atenolol; Carteolol (Ophthalmic); Levobunolol; Metipranolol; Nadolol; Sotalol. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Cardiac Glycosides: Aminoquinolines (Antimalarial) may increase the serum concentration of Cardiac Glycosides. Monitor therapy
Chloroquine: May increase the serum concentration of Primaquine. Monitor therapy
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Cobicistat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Moderate): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Strong): May diminish the therapeutic effect of Primaquine. Management: Monitor for signs and symptoms of possible treatment failure with primaquine in patients who are taking strong CYP2D6 inhibitors. If efficacy of primaquine is compromised, may consider adjusting therapies. Consider therapy modification
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dacomitinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of dacomitinib with CYP2D6 subtrates that have a narrow therapeutic index. Consider therapy modification
Dapsone (Systemic): Antimalarial Agents may enhance the adverse/toxic effect of Dapsone (Systemic). Specifically, concomitant use of antimalarial agents with dapsone may increase the risk of hemolytic reactions. Dapsone (Systemic) may enhance the adverse/toxic effect of Antimalarial Agents. Specifically, concomitant use of dapsone with antimalarial agents may increase the risk for hemolytic reactions. Management: Closely monitor patients for signs/symptoms of hemolytic reactions with concomitant use of dapsone and antimalarial agents, particularly in patients deficient in glucose-6-phosphate dehydrogenase (G6PD), methemoglobin reductase, or with hemoglobin M. Consider therapy modification
Dapsone (Topical): Antimalarial Agents may enhance the adverse/toxic effect of Dapsone (Topical). Specifically, the risk of hemolytic reactions may be increased. Management: Closely monitor for signs/symptoms of hemolytic reactions with concomitant use of topical dapsone and antimalarial agents. Patients with glucose-6-phosphate dehydrogenase deficiency may be at particularly high risk for adverse hematologic effects. Consider therapy modification
Darunavir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lumefantrine: Antimalarial Agents may enhance the adverse/toxic effect of Lumefantrine. Management: Artemether/Lumefantrine (combination product) should not be used with other antimalarials unless there is no other treatment option. Avoid combination
Mefloquine: Aminoquinolines (Antimalarial) may enhance the adverse/toxic effect of Mefloquine. Specifically, the risk for QTc-prolongation and the risk for convulsions may be increased. Mefloquine may increase the serum concentration of Aminoquinolines (Antimalarial). Management: Avoid concurrent use, and delay administration of mefloquine until at least 12 hours after the last dose of an aminoquinoline antimalarial when possible. Avoid combination
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Perhexiline: CYP2D6 Substrates (High risk with Inhibitors) may increase the serum concentration of Perhexiline. Perhexiline may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QuiNINE: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Adverse Reactions
Frequency not defined.
Cardiovascular: Cardiac arrhythmia, dizziness, prolonged Q-T interval on ECG
Dermatologic: Pruritus, skin rash
Gastrointestinal: Abdominal cramps, epigastric distress, nausea, vomiting
Hematologic & oncologic: Anemia, hemolytic anemia (in patients with G6PD deficiency), leukopenia, methemoglobinemia (in NADH-methemoglobin reductase-deficient individuals)
Warnings/Precautions
Concerns related to adverse effects:
- Cardiovascular effects: May cause QT prolongation; monitor ECG in patients with cardiac disease, long QT syndrome, a history of ventricular arrhythmias, uncorrected hypokalemia and/or hypomagnesemia, or bradycardia (<50 beats per minute), and during concomitant administration with QT interval prolonging agents.
- Hematologic effects: Anemia, methemoglobinemia, and leukopenia have been associated with primaquine use; monitor during treatment; do not exceed recommended dosage and duration. Closely monitor patients who have a family or personal history of hemolytic anemia or who have had a prior hematologic adverse reaction attributed to primaquine. Immediately discontinue if marked darkening of the urine or sudden decrease in hemoglobin concentration or leukocyte count occurs.
- Hemolytic anemia: Promptly discontinue with signs of hemolytic anemia (darkening of urine, marked fall in hemoglobin or erythrocyte count). Moderate to severe hemolytic reactions may occur in individuals with glucose-6-phosphate dehydrogenase (G6PD) deficiency and personal or familial history of favism. Geographic regions with a high prevalence of G6PD deficiency (eg, Africa, southern Europe, Mediterranean region, Middle East, southeast Asia, Oceania) are associated with a higher incidence of hemolytic anemia.
Disease-related concerns:
- G6PD deficiency: Screen for G6PD deficiency prior to therapy initiation. Use is contraindicated in patients with severe G6PD deficiency. Assess benefits/risks of treatment when considering use in patients with mild to moderate G6PD deficiency or those patients whose G6PD status is unknown and testing is not available. Also assess risk factors for G6PD deficiency or favism in patients with unknown G6PD status. If a decision is made to administer primaquine to a patient with mild to moderate G6PD deficiency or unknown G6PD status (when testing is not available), perform baseline hematocrit and hemoglobin testing and closely monitor hematological parameters (eg, at day 3 and 8). Immediately discontinue treatment if signs of hemolytic anemia occur.
- NADH methemoglobin reductase deficiency: Use with caution in patients with a personal or family history of NADH methemoglobin reductase deficiency; methemoglobinemia may occur.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer’s labeling.
Monitoring Parameters
Periodic CBC (in G6PD normal patients), visual color check of urine, glucose, electrolytes; if hemolysis suspected, monitor CBC, haptoglobin, peripheral smear, urinalysis dipstick for occult blood, G6PD deficiency screening (prior to initiating treatment); baseline hematocrit and hemoglobin testing and periodic CBC (eg, at day 3 and 8) in patients with mild to moderate G6PD deficiency or unknown G6PD status (when testing is not available); ECG (in patients at risk for QT prolongation). Pregnancy test prior to therapy in sexually active females.
Pregnancy
Pregnancy Considerations
Primaquine is contraindicated in pregnant women.
Malaria infection in pregnant women may be more severe than in nonpregnant women and has a high risk of maternal and perinatal morbidity and mortality. Therefore, pregnant women and women who are likely to become pregnant are advised to avoid travel to malaria-risk areas. When treatment is needed, other agents are preferred (CDC Yellow Book 2016). Consult current CDC guidelines for the treatment of malaria during pregnancy.
Sexually active females should have a pregnancy test prior to treatment with primaquine. Females of reproductive potential should use effective contraception during therapy and until the next menses following discontinuation of treatment. Males with female partners of reproductive potential should use condoms during therapy and for 3 months after treatment is discontinued.
Patient Education
What is this drug used for?
- It is used to treat or prevent malaria.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Abdominal cramps
- Abdominal pain
- Vomiting
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Methemoglobinemia like blue or gray color of the lips, nails, or skin; arrhythmia; seizures; severe dizziness or passing out; severe headache; fatigue; loss of strength and energy; or shortness of breath
- Dark urine
- Chills
- Yellow skin
- Dizziness
- Fast heartbeat
- Abnormal heartbeat
- Severe loss of strength and energy
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.