Boxed Warning
Drug-induced lupus erythematosus-like syndrome:
The prolonged administration of procainamide often leads to the development of a positive antinuclear antibody (ANA) test, with or without symptoms of a lupus erythematosus-like syndrome. If a positive ANA titer develops, the benefits versus risks of continued procainamide therapy should be assessed.
Mortality:
In the National Heart, Lung and Blood Institute's Cardiac Arrhythmia Suppression Trial (CAST), a long-term, multicenter, randomized, double-blind study in patients with asymptomatic non-life-threatening ventricular arrhythmias who had myocardial infarction more than 6 days but less than 2 years previously, an excessive mortality or nonfatal cardiac arrest rate (7.7%) was seen in patients treated with encainide or flecainide compared with that seen in patients assigned to matched placebo-treated group (3%). The average duration of treatment with encainide or flecainide in this study was 10 months.
The applicability of the CAST results to other populations (eg, those without recent myocardial infarctions) is uncertain. Considering the known proarrhythmic properties of procainamide and the lack of evidence of improved survival for any antiarrhythmic drug in patients without life-threatening arrhythmias, the use of procainamide as well as other antiarrhythmic agents should be reserved for patients with life-threatening ventricular arrhythmias.
Blood dyscrasias:
Agranulocytosis, bone marrow depression, neutropenia, hypoplastic anemia and thrombocytopenia in patients receiving procainamide HCl have been reported at a rate of approximately 0.5%. Most of these patients received procainamide within the recommended dosage range. Fatalities have occurred (with approximately 20 to 25% mortality in reported cases of agranulocytosis). Since most of these events have been noted during the first 12 weeks of therapy, it is recommended that complete blood counts including white cell, differential and platelet counts be performed at weekly intervals for the first 3 months of therapy, and periodically thereafter. Complete blood counts should be performed promptly if the patient develops any signs of infection (such as fever, chills, sore throat or stomatitis), bruising or bleeding. If any of those hematologic disorders are identified, procainamide therapy should be discontinued. Blood counts usually return to normal within 1 month of discontinuation. Caution should be used in patients with preexisting marrow failure or cytopenia of any type.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Injection, as hydrochloride:
Generic: 100 mg/mL (10 mL); 500 mg/mL (2 mL)
Pharmacology
Mechanism of Action
Decreases myocardial excitability and conduction velocity and may depress myocardial contractility, by increasing the electrical stimulation threshold of ventricle, His-Purkinje system and through direct cardiac effects
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: Children: 2.2 L/kg; Adults: 2 L/kg; decreased with congestive heart failure or shock
Metabolism
Hepatic via acetylation to produce N-acetyl procainamide (NAPA) (active metabolite)
Excretion
Urine (30% to 60% unchanged procainamide; 6% to 52% as NAPA); feces (<5% unchanged procainamide. Note: >80% of formed NAPA is renally eliminated in contrast to procainamide which is ~50% renally eliminated (Gibson, 1977).
Onset of Action
IM 10 to 30 minutes
Time to Peak
Serum: IM: 15 to 60 minutes
Half-Life Elimination
Procainamide (hepatic acetylator, phenotype, cardiac and renal function dependent): Children: 1.7 hours; Adults: 2.5 to 4.7 hours; Anephric: 11 hours
NAPA (renal function dependent): Children: 6 hours; Adults: 6 to 8 hours; Anephric: 42 hours
Protein Binding
15% to 20%
Use in Specific Populations
Special Populations: Renal Function Impairment
Elimination half-life is prolonged.
Special Populations: Elderly
Elimination half-life is prolonged.
Use: Labeled Indications
Ventricular arrhythmias: Intravenous: Treatment of life-threatening ventricular arrhythmias
Supraventricular arrhythmias: Oral [Canadian product]: Treatment of supraventricular arrhythmias. Note: In the treatment of atrial fibrillation, use only when preferred treatment is ineffective or cannot be used. Use in paroxysmal atrial tachycardia when reflex stimulation or other measures are ineffective.
Use: Off Label
Atrial fibrillation (preexcited)yes
Based on the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science and the 2014 American Heart Association/American College of Cardiology/Heart Rhythm Society Guideline (AHA/ACC/HRS) for the Management of Patients With Atrial Fibrillation (AF), procainamide may be considered for the treatment of hemodynamically stable preexcited AF with rapid ventricular response in adults with preserved left ventricular function.
Junctional tachycardiayes
Based on the American Heart Association, American College of Clinical Cardiology and Heart Rhythm Society Guideline for the Management of Patients with Supraventricular Tachycardia, procainamide may be considered for the treatment of hemodynamically, acute junctional tachycardia when beta-blocker therapy is ineffective. Dosing not specified.
Stable monomorphic ventricular tachycardiayes
Based on the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science, procainamide is an effective and recommended treatment alternative for hemodynamically stable monomorphic ventricular tachycardia in adults with preserved left ventricular function. Use should be avoided in those with a prolonged QT interval.
Contraindications
Hypersensitivity to procainamide, procaine, other ester-type local anesthetics, or any component of the formulation; complete heart block; second-degree AV block or various types of hemiblock (without a functional artificial pacemaker); SLE; torsade de pointes
Canadian labeling: Additional contraindications (not in US labeling):Myasthenia gravis; severe heart failure (IV); renal failure (IV); shock (IV)
Dosage and Administration
Dosing: Adult
Note: Dose must be individualized and titrated to patient response. Use ideal body weight for weight-based doses (Christoff 1983).
Ventricular arrhythmias: Hemodynamically stable, sustained monomorphic ventricular tachycardia (off label): IV:
Loading dose: 10 to 17 mg/kg at a rate of 20 to 50 mg/minute or 100 mg every 5 minutes; administer until arrhythmia is controlled, hypotension occurs, or QRS complex widens by 50% of its original width. Although manufacturer's labeling suggests a maximum total loading dose of 1 g, clinical evidence suggests higher weight based loading doses of up to 17 mg/kg may be needed (ACLS [Neumar 2010]; AHA/ACC/HRS [Al-Khatib 2017]). Note: Not recommended for use in ongoing ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT) due to prolonged administration time and lack of efficacy (AHA 2005; AHA/ACC/HRS [Al-Khatib 2017]).
Maintenance infusion: 1 to 4 mg/minute (ACLS [Neumar 2010]; AHA/ACC/HRS [Al-Khatib 2017]). Manufacturer labeling suggests a maintenance infusion of 2 to 6 mg/minute.
Supraventricular arrhythmias:
Oral [Canadian product]: Sustained release formulation (Procan SR): Maintenance: 50 mg/kg/24 hours given in divided doses every 6 hours.
Suggested Procan SR maintenance dose:
<55 kg: 500 mg every 6 hours
55 to 91 kg: 750 mg every 6 hours
>91 kg: 1 g every 6 hours
Atrial fibrillation (preexcited) (off-label use): IV:
Loading dose: Up to 17 mg/kg at a rate of 20 to 50 mg/minute or 100 mg every 5 minutes; administer until arrhythmia is controlled, hypotension occurs, or QRS complex widens by 50% of its original width. Although manufacturer's labeling suggests a maximum total loading dose of 1 g, clinical evidence suggests higher weight-based loading doses of up to 17 mg/kg may be needed (ACLS [Neumar 2010]).
Maintenance infusion: 1 to 4 mg/minute (ACLS [Neumar 2010]; Hazinski 2015).
Dosing: Geriatric
Refer to adult dosing. Initiate doses at lower end of dosage range.
Dosing: Pediatric
Note: Dose must be individualized and titrated to patient's response; monitor serum concentrations.
Antiarrhythmic: Limited data available:
IM: Children and Adolescents: 20 to 30 mg/kg/day divided every 4 to 6 hours; maximum daily dose: 4000 mg/day (Nelson, 1996)
IV, I.O.: Infants, Children, and Adolescents:
Loading dose: 10 to 15 mg/kg over 30 to 60 minutes; in adults, maximum dose range: 1000 to 1500 mg (Hegenbarth, 2008; Kliegman, 2011)
Maintenance: Continuous IV infusion: 20 to 80 mcg/kg/minute; maximum daily dose: 2000 mg/24 hours (Kliegman, 2011)
Stable wide-complex tachycardia of unknown origin (atrial or ventricular) or SVT (PALS [Kleinman, 2010]): Infants, Children, and Adolescents: Note: Avoid or use extreme caution when administering procainamide with other drugs that prolong QT interval (eg, amiodarone); consider consulting with cardiology expert
IV, I.O.: Loading dose: 15 mg/kg infused over 30-60 minutes; monitor ECG and blood pressure; stop the infusion if hypotension occurs or QRS complex widens by >50% of baseline
Reconstitution
IV: Dilute loading dose to a maximum concentration of 20 mg/mL.
Administration
Oral: Canadian product: Do not crush or chew sustained release drug products
IV: Must dilute prior to IV administration. Dilute loading dose to a maximum concentration of 20 mg/mL; administer loading dose at a maximum rate of 50 mg/minute
Storage
Store intact vials at 20°C to 25°C (68°F to 77°F). The solution is initially colorless but may turn slightly yellow on standing. Discard solutions darker than light amber.
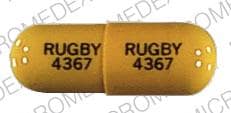
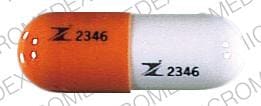
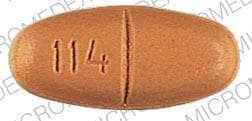
Procainamide Images
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Ajmaline: May enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). QT-prolonging Class IA Antiarrhythmics (Highest Risk) may increase the serum concentration of Ajmaline. Avoid combination
Amiodarone: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Amiodarone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Amisulpride: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Amisulpride. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Asunaprevir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Azithromycin (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Azithromycin (Systemic). Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Ceritinib: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Ceritinib. Ceritinib may enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Chloroquine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Chloroquine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Cimetidine: May increase the serum concentration of Procainamide. Management: Consider an alternative H2-receptor antagonist in patients taking procainamide. If combined, monitor for increased therapeutic effects/toxicity of procainamide. Consider therapy modification
Citalopram: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Citalopram. Avoid combination
Clarithromycin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Clarithromycin. Avoid combination
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Clofazimine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Clofazimine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
CloZAPine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of CloZAPine. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Cobicistat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Crizotinib: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Crizotinib. Crizotinib may enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Crizotinib may increase the serum concentration of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
CYP2D6 Inhibitors (Moderate): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Strong): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Dacomitinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of dacomitinib with CYP2D6 subtrates that have a narrow therapeutic index. Consider therapy modification
Darunavir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Dasatinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Dasatinib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Domperidone: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Domperidone. Avoid combination
Doxepin-Containing Products: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Doxepin-Containing Products. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Droperidol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Droperidol. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Encorafenib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Entrectinib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Avoid combination
Erdafitinib: May increase the serum concentration of OCT2 Substrates. Monitor therapy
Erythromycin (Systemic): QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Erythromycin (Systemic). Erythromycin (Systemic) may enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Erythromycin (Systemic) may increase the serum concentration of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Escitalopram: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Escitalopram. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Avoid combination
Fingolimod: May enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Avoid combination
Flecainide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Flecainide. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Fluconazole: May enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Flupentixol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Flupentixol. Avoid combination
Gadobenate Dimeglumine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Gadobenate Dimeglumine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Gemifloxacin: May enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Avoid combination
Gilteritinib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Consider alternatives to this combination. If use is necessary, monitor for QTc interval prolongation and arrhythmias. Consider therapy modification
Halofantrine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Halofantrine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Haloperidol: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Inotuzumab Ozogamicin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Inotuzumab Ozogamicin. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Lacosamide: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
LamoTRIgine: May increase the serum concentration of Procainamide. Management: Consider monitoring for increased procainamide concentrations and/or systemic effects in patients receiving procainamide with lamotrigine. The lamotrigine Canadian product monograph states that coadministration of these agents is not recommended. Monitor therapy
Levofloxacin-Containing Products (Systemic): May enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Avoid combination
Lofexidine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Lofexidine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Lumefantrine: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Lurasidone: May enhance the QTc-prolonging effect of Procainamide. Management: Consider alternatives to procainamide in patients with acute lurasidone overdose. If procainamide treatment cannot be avoided, monitor for excessive QTc interval prolongation. Consider therapy modification
Methadone: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Methadone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Midostaurin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Midostaurin. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Moxifloxacin (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Moxifloxacin (Systemic). Avoid combination
Neuromuscular-Blocking Agents: Procainamide may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents. Monitor therapy
Nilotinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Nilotinib. Avoid combination
OLANZapine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of OLANZapine. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Ondansetron: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Ondansetron. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Osimertinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Osimertinib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Pentamidine (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pentamidine (Systemic). Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Perhexiline: CYP2D6 Substrates (High risk with Inhibitors) may increase the serum concentration of Perhexiline. Perhexiline may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Pilsicainide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pilsicainide. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Pimozide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pimozide. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Avoid combination
Piperaquine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Piperaquine. Avoid combination
Probucol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Probucol. Avoid combination
Propafenone: May enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Agents (Indeterminate Risk - Avoid): May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Agents (Indeterminate Risk - Caution): May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Class IA Antiarrhythmics (Highest Risk): May enhance the QTc-prolonging effect of other QT-prolonging Class IA Antiarrhythmics (Highest Risk). Exceptions: Ajmaline. Avoid combination
QT-prolonging Class III Antiarrhythmics (Highest Risk): QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Avoid combination
QT-prolonging Kinase Inhibitors (Highest Risk): May enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Miscellaneous Agents (Highest Risk): QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QUEtiapine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of QUEtiapine. Avoid combination
RaNITIdine: May increase the serum concentration of Procainamide. Ranitidine may also increase the concentration of the active N-acetyl-procainamide (NAPA) metabolite. Monitor therapy
Ribociclib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Ribociclib. Avoid combination
RisperiDONE: QT-prolonging Agents (Highest Risk) may enhance the CNS depressant effect of RisperiDONE. QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of RisperiDONE. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Saquinavir: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Saquinavir. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Sodium Stibogluconate: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Sodium Stibogluconate. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Sparfloxacin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Sparfloxacin. Avoid combination
Tafenoquine: May increase the serum concentration of MATE1 Substrates. Management: Avoid use of MATE substrates with tafenoquine, and if the combination cannot be avoided, monitor closely for evidence of toxicity of the MATE substrate and consider a reduced dose of the MATE substrate according to that substrate's labeling. Consider therapy modification
Tafenoquine: May increase the serum concentration of OCT2 Substrates. Management: Avoid use of OCT2 substrates with tafenoquine, and if the combination cannot be avoided, monitor closely for evidence of toxicity of the OCT2 substrate and consider a reduced dose of the OCT2 substrate according to that substrate's labeling. Consider therapy modification
Thioridazine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Thioridazine. Avoid combination
Trimethoprim: May increase serum concentrations of the active metabolite(s) of Procainamide. Trimethoprim may increase the serum concentration of Procainamide. Consider therapy modification
Vemurafenib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Vemurafenib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Voriconazole: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Voriconazole. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Test Interactions
In the presence of propranolol or suprapharmacologic concentrations of lidocaine or meprobamate, tests which depend on fluorescence to measure procainamide/NAPA concentrations may be affected.
Adverse Reactions
>10%:
Hematologic & oncologic: Positive ANA titer (≤50%)
Neuromuscular & skeletal: Lupus-like syndrome (≤30%, increased incidence with long-term therapy or slow acetylators; syndrome may include abdominal pain, arthralgia, arthritis, chills, fever, hepatomegaly, myalgia, pericarditis, pleural effusion, pulmonary infiltrates, skin rash)
1% to 10%:
Cardiovascular: Hypotension (intravenous: ≤5%)
Dermatologic: Skin rash
Gastrointestinal: Diarrhea (oral: 3% to 4%), dysgeusia (oral: 3% to 4%), nausea (oral: 3% to 4%), vomiting (oral: 3% to 4%)
<1%, postmarketing, and/or case reports: Agranulocytosis, angioedema, anorexia, aplastic anemia, arthralgia, asystole, bone marrow depression, cerebellar ataxia, confusion, demyelinating disease (demyelinating polyradiculoneuropathy), depression, depression of myocardial contractility, disorientation, dizziness, drug fever, exacerbation of cardiac arrhythmia, exacerbation of myasthenia gravis, fever, first degree atrioventricular block, flushing, gastrointestinal pseudo-obstruction, granulomatous hepatitis, hallucination, hemolytic anemia, hepatic failure, hyperbilirubinemia, hypoplastic anemia, increased serum alkaline phosphatase, increased serum transaminases, intrahepatic cholestasis, leukopenia, maculopapular rash, mania, myocarditis, myopathy, neuromuscular blockade, neutropenia, pancreatitis, pancytopenia, peripheral neuropathy, pleural effusion, polyneuropathy, positive direct Coombs test, prolonged Q-T interval on ECG, psychosis, pruritus, pulmonary embolism, second degree atrioventricular block, tachycardia, thrombocytopenia, torsades de pointes, urticaria, vasculitis, ventricular fibrillation, ventricular tachycardia (paradoxical; in atrial fibrillation/flutter), weakness
Warnings/Precautions
Concerns related to adverse effects:
- Blood dyscrasias: [US Boxed Warning]: Potentially fatal blood dyscrasias (eg, agranulocytosis) have occurred with therapeutic doses; weekly monitoring is recommended during the first 3 months of therapy and periodically thereafter. Discontinue procainamide if this occurs.
- Conduction disturbances: Reduce dose if first-degree heart block occurs.
- Drug-induced lupus erythematosus-like syndrome: [US Boxed Warning]: Long-term administration leads to the development of a positive antinuclear antibody (ANA) test in 50% of patients which may result in a drug-induced lupus erythematosus-like syndrome (in 20% to 30% of patients); discontinue procainamide with rising ANA titers or with SLE symptoms and choose an alternative agent.
- Proarrhythmic effects: Watch for proarrhythmic effects; monitor and adjust dose to prevent QTc prolongation. Avoid use in patients with QT prolongation (ACLS, 2010).
Disease-related concerns:
- Atrial fibrillation/flutter: May increase ventricular response rate in patients with atrial fibrillation or flutter; control AV conduction before initiating.
- Electrolyte imbalance: Correct electrolyte disturbances, especially hypokalemia or hypomagnesemia, prior to use and throughout therapy.
- Heart failure (HF): Use with caution or avoid (ACLS, 2010) in patients with HF; may precipitate or exacerbate condition due to negative inotropic actions.
- Myasthenia gravis: Avoid use in myasthenia gravis; may worsen condition.
- Renal impairment: Use with caution in patients with renal impairment; dosage reduction recommended.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Sodium metabisulfite: The injectable product may contain sodium metabisulfite which can cause allergic-type reactions, including anaphylactic symptoms and life-threatening asthmatic episodes in susceptible people; this is seen more frequently in asthmatics.
Special populations:
- Elderly: Use caution and dose cautiously; renal clearance of procainamide/NAPA declines in patients ≥50 years of age (independent of creatinine clearance reductions) and in the presence of concomitant renal impairment.
Other warnings/precautions:
- CAST trial: [US Boxed Warning] In the Cardiac Arrhythmia Suppression Trial (CAST), recent (>6 days but <2 years ago) myocardial infarction patients with asymptomatic, non-life-threatening ventricular arrhythmias did not benefit and may have been harmed by attempts to suppress the arrhythmia with flecainide or encainide. An increased mortality or nonfatal cardiac arrest rate (7.7%) was seen in the active treatment group compared with patients in the placebo group (3%). The applicability of the CAST results to other populations is unknown. Procainamide should be reserved for patients with life-threatening ventricular arrhythmias.
Monitoring Parameters
ECG (with attention to the QRS duration and QT interval), blood pressure, renal function; with prolonged use monitor CBC with differential, platelet count; procainamide and NAPA blood concentrations in patients with hepatic impairment, renal impairment, or receiving constant infusion >3 mg/minute for longer than 24 hours; ANA titers with chronic oral use
Consult individual institutional policies and procedures.
Pregnancy
Pregnancy Considerations
Procainamide crosses the placenta (Dumesic 1982; Oudijk 2002); procainamide and its active metabolite (N-acetyl procainamide) can be detected in the cord blood and neonatal serum (Pittard 1983). Intravenous procainamide may be considered for the acute treatment of SVT in pregnant women. Due to adverse events (lupus-like syndrome), long-term therapy should be avoided unless other options are not available (Page [ACC/AHA/HRS 2015]).
Patient Education
What is this drug used for?
- It is used to treat certain types of abnormal heartbeats.
- This drug will be started in a hospital where you will be closely watched. Talk with your doctor.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Lupus like rash on the cheeks or other body parts, sunburn easy, muscle or joint pain, chest pain or shortness of breath, or swelling in the arms or legs.
- Infection
- Bruising
- Bleeding
- Severe loss of strength and energy
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Chest pain
- Depression
- Mood changes
- Sensing things that seem real but are not
- Severe nausea
- Vomiting
- Joint pain
- Joint swelling
- Diarrhea
- Severe dizziness
- Passing out
- Fast heartbeat
- Slow heartbeat
- Abnormal heartbeat
- Mouth sores
- Mouth irritation
- Muscle pain
- Muscle weakness
- Excessive weight gain
- Swelling of arms or legs
- Shortness of breath
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.