Boxed Warning
Hepatotoxicity:
Severe liver injury and acute liver failure, in some cases fatal, have been reported in patients treated with propylthiouracil. These reports of hepatic reactions include cases requiring liver transplantation in adults and pediatric patients.
Reserve propylthiouracil for patients who cannot tolerate methimazole and in whom radioactive iodine therapy or surgery are not appropriate treatments for the management of hyperthyroidism.
Pregnancy:
Because of the risk of fetal abnormalities associated with methimazole, propylthiouracil may be the treatment of choice when an antithyroid drug is indicated during or just prior to the first trimester of pregnancy.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Generic: 50 mg
Pharmacology
Mechanism of Action
Inhibits the synthesis of thyroid hormones by interfering with thyroid peroxidase (TPO) which oxidizes iodide, subsequently catalyzes formation of mono- and di-iodotyrosines (MIT and DIT) on thyroglobulin, and catalyzes coupling reactions between MIT and DIT to form thyroxine (T4) and triiodothyronine (T3) (Burch 2015); also blocks conversion of T4 to T3 in peripheral tissues (does not inactivate existing T4 and T3 stores in circulating blood and the thyroid and does not interfere with replacement thyroid hormones).
Pharmacokinetics/Pharmacodynamics
Distribution
Concentrated in the thyroid gland (Clark 2006)
Metabolism
Hepatic
Excretion
Urine (35%; primarily as metabolites)
Onset of Action
For significant therapeutic effects 24 to 36 hours are required; remission of hyperthyroidism usually does not occur before 4 months of continued therapy
Time to Peak
1 to 2 hours (Clark 2006)
Duration of Action
12 to 24 hours (Clark 2006)
Half-Life Elimination
~1 hour (Clark 2006)
Protein Binding
80% to 85% (Clark 2006)
Use: Labeled Indications
Hyperthyroidism: Treatment of hyperthyroidism in patients with Graves' disease or toxic multinodular goiter who are intolerant of methimazole and for whom surgery or radioactive iodine therapy is not an appropriate treatment regimen; amelioration of hyperthyroid symptoms in preparation for thyroidectomy or radioactive iodine therapy (in patients who are intolerant of methimazole).
Use: Off Label
Thyroid storm or thyrotoxicosisyes
Based on the American Thyroid Association guidelines for the management of Hyperthyroidism and Other Causes of Thyrotoxicosis, treatment with propylthiouracil is recommended in thyroid storm or thyrotoxicosis to reduce thyroid hormone production and to block T4 to T3 conversion. Propylthiouracil is preferred over methimazole in thyroid storm due to inhibition of peripheral conversion of T4 to T3 as well as thyroid hormone synthesis Ross 2016.
Contraindications
Hypersensitivity to propylthiouracil or any component of the formulation
Canadian labeling: Additional contraindications (not in US labeling): Breastfeeding
Dosage and Administration
Dosing: Adult
Hyperthyroidism: Oral: Initial: 300 mg daily in 3 equally divided doses (~8-hour intervals); 400 mg daily in patients with severe hyperthyroidism and/or very large goiters; an occasional patient will require 600 to 900 mg daily; usual maintenance: 100 to 150 mg daily in 3 equally divided doses
Adjust dosage as required to achieve and maintain serum T3, T4, and TSH levels in the normal range. An elevated T3 may be the sole indicator of inadequate treatment. An elevated TSH indicates excessive antithyroid treatment.
Hyperthyroidism associated with Graves’ disease (off-label) (Ross 2016): Oral: Initial: 50 to 150 mg (depending on severity) 3 times daily to restore euthyroidism; as clinical condition improves, may reduce dosage to usual maintenance dose of 50 mg 2 to 3 times daily for a total of ~12 to 18 months then discontinue if thyroid function tests (eg, TSH, thyrotropin receptor antibody [TRAb]) are normal at that time.
Thyrotoxic crisis/thyroid storm (off-label use): Oral: Note: Recommendations vary widely and have not been evaluated in comparative trials. The American Thyroid Association recommends a loading dose of 500 to 1,000 mg followed by 250 mg every 4 hours (Ross 2016). As thyrotoxicosis improves, a gradual dose reduction to a dose within the standard maintenance ranges is recommended (Goldberg 2003).
Dosing: Geriatric
Refer to adult dosing; use with caution.
Dosing: Pediatric
Note: Due to reports of severe liver toxicity, propylthiouracil is not recommended for use in pediatric patients and dosing is no longer FDA-approved for pediatric patients; use should be limited to patients who have developed minor toxic reactions to methimazole and who are not candidates for surgery or radioactive iodine treatment. If used, limit duration to short course of therapy. Discontinue therapy if transaminases reach 2 to 3 times ULN and fail to resolve within a week of repeat testing (Bahn [ATA/AACE 2011]).
Hyperthyroidism: Note: Adjust dosage to maintain T3, T4, and TSH in normal range; elevated T3 may be sole indicator of inadequate treatment. Elevated TSH indicates excessive antithyroid treatment. Oral:
Children: ≥6 years and Adolescents: Limited data available [Propyl-Thyracil Prescribing Information (Canada)]:
Initial: 150 mg/m2/day
6 to 10 years: 50 to 150 mg/day divided every 8 hours
≥10 years: 150 to 300 mg/day divided every 8 hours
Maintenance (once euthyroid): Dose should be individualized based on patient response: Usual dose: 50 mg twice daily
Extemporaneously Prepared
A 5 mg/mL oral suspension may be made with tablets and a 1:1 mixture of Ora-Plus and Ora-Sweet. Crush twenty 50 mg propylthiouracil tablets in a mortar and reduce to a fine powder. Add small portions of vehicle and mix to a uniform paste; mix while adding vehicle in incremental proportions to almost 200 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 200 mL. Label "shake well" and "refrigerate". Stable for 91 days refrigerated (preferred) and 70 days at room temperature.
Nahata MC, Pai VB, and Hipple TF, Pediatric Drug Formulations, 5th ed, Cincinnati, OH: Harvey Whitney Books Co, 2004.
Administration
Oral: Administer in 3 equally divided doses at approximately 8-hour intervals.
Storage
Store at 15°C to 30°C (59°F to 86°F).
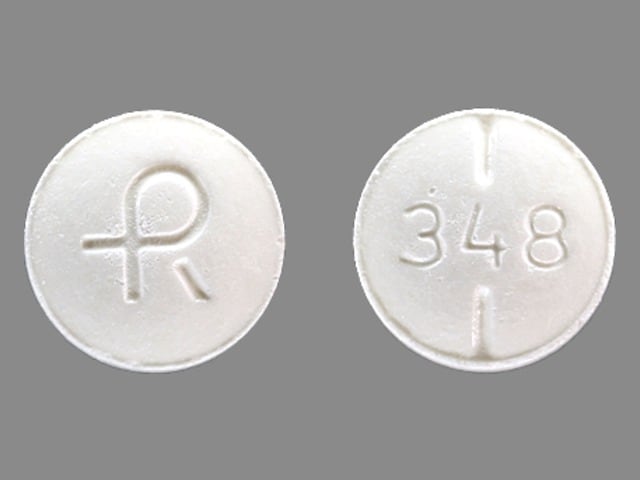
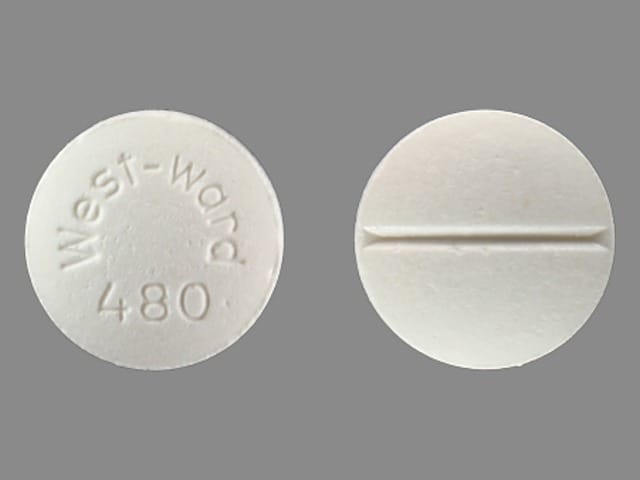
Propylthiouracil Images
Drug Interactions
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Cardiac Glycosides: Antithyroid Agents may increase the serum concentration of Cardiac Glycosides. Monitor therapy
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Macimorelin: Propylthiouracil may diminish the diagnostic effect of Macimorelin. Avoid combination
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Sodium Iodide I131: Antithyroid Agents may diminish the therapeutic effect of Sodium Iodide I131. Management: Discontinue antithyroid therapy 3-4 days prior to sodium iodide I-131 administration. Avoid combination
Theophylline Derivatives: Antithyroid Agents may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Antithyroid Agents may diminish the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Adverse Reactions
Frequency not defined.
Cardiovascular: Edema, periarteritis, vasculitis (ANCA-positive, cutaneous, leukocytoclastic)
Central nervous system: Drowsiness, drug fever, headache, neuritis, paresthesia, vertigo
Dermatologic: Alopecia, dermal ulcer, erythema nodosum, exfoliative dermatitis, pruritus, skin pigmentation, skin rash, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Gastrointestinal: Ageusia, dysgeusia, nausea, salivary gland disease, stomach pain, vomiting
Hematologic & oncologic: Agranulocytosis, aplastic anemia, granulocytopenia, hemorrhage, hypoprothrombinemia, leukopenia, lymphadenopathy, splenomegaly, thrombocytopenia
Hepatic: Acute hepatic failure, hepatitis, hepatotoxicity (idiosyncratic) (Chalasani 2014), jaundice
Neuromuscular & skeletal: Arthralgia, lupus-like syndrome, myalgia
Renal: Acute renal failure, glomerulonephritis, nephritis
Respiratory: Interstitial pneumonitis, pulmonary alveolar hemorrhage
Miscellaneous: Fever
Warnings/Precautions
Concerns related to adverse effects:
- Bleeding: May cause hypoprothrombinemia and bleeding. Monitoring is recommended, especially before surgical procedures.
- Bone marrow suppression: May cause significant bone marrow depression; the most severe manifestation is agranulocytosis (usually occurs within first 3 months of therapy). Aplastic anemia (Shaikh 2019), thrombocytopenia, and leukopenia may also occur. Use with caution in patients receiving other drugs known to cause myelosuppression (particularly agranulocytosis); discontinue if significant bone marrow suppression occurs, particularly agranulocytosis or aplastic anemia.
- Dermatologic toxicity: May occur; discontinue in the presence of exfoliative dermatitis.
- Fever: Discontinue in the presence of unexplained fever.
- Hepatotoxicity: [US Boxed Warning]: Severe liver injury and acute liver failure (some fatal) have been reported and have included cases requiring liver transplantation in adult and pediatric patients, including pregnant women. Reserve propylthiouracil for patients who cannot tolerate methimazole and in whom radioactive iodine therapy or surgery are not appropriate treatments for the management of hyperthyroidism. Routine liver function test monitoring may not reduce risk due to unpredictable and rapid onset. Patients should be counseled to recognize and report symptoms suggestive of hepatic dysfunction (eg, anorexia, pruritus, right upper quadrant pain), especially in first 6 months of treatment, which should prompt immediate discontinuation. Discontinue therapy if transaminases are >3 times the upper limit of normal or if levels elevated at the onset of therapy increase further (Ross 2016).
- Hypothyroidism: May cause hypothyroidism; routinely monitor TSH and free T4 levels, adjust dose to maintain euthyroid state.
- Lupus-like syndrome: A lupus-like syndrome (including splenomegaly and vasculitis) may occur.
- Nephritis: Has been associated with nephritis and glomerulonephritis, sometimes leading to acute renal failure.
- Pneumonitis: Interstitial pneumonitis has been reported; discontinue if this reaction occurs.
- Vasculitis: ANCA-positive vasculitis or leukocytoclastic vasculitis may occur; discontinue in patients who develop vasculitis during therapy.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pregnancy: [US Boxed Warning]: Due to the risk of fetal abnormalities associated with methimazole, propylthiouracil may be the treatment of choice when an antithyroid drug is indicated during or just prior to the first trimester of pregnancy.
Monitoring Parameters
Signs and symptoms of illness (ie fever, sore throat, skin eruptions, general malaise)
CBC with differential (baseline and if development of febrile illness or pharyngitis occurs); prothrombin time (especially before surgical procedures), liver function tests (bilirubin, alkaline phosphatase, ALT, AST at baseline and if symptoms of liver injury occur [Ross 2016])
Thyroid function tests:
Serum free T4 and total T3 2 to 6 weeks after initiation, repeat in 4 to 6 weeks if dose is adjusted and then every 2 to 3 months once euthyroid levels are achieved; [with long term therapy (ie, >18 months) may extend interval to every 4 to 6 months]; in patients with Graves’ disease, if TRAb is negative, thyroid function tests should be monitored every 2 to 3 months for the first 6 months after discontinuing therapy, then at 4- to 6-month intervals for the next 6 months, then every 6 to 12 months thereafter (Ross 2016)
TSH (periodically throughout treatment; TSH is not an adequate parameter to assess initial response as levels may remain suppressed for several months after starting therapy) (Ross 2016).
TRAb in patients with Graves’ disease (prior to stopping medication, elevation at the end of therapy decreases likelihood of remission) (Ross 2016).
Pregnancy
Pregnancy Risk Factor
D
Pregnancy Considerations
Propylthiouracil crosses the placenta.
Nonteratogenic adverse effects, including fetal and neonatal hypothyroidism, goiter, and hyperthyroidism, have been reported following maternal propylthiouracil use.
Uncontrolled maternal hyperthyroidism may result in adverse neonatal outcomes (eg, prematurity, low birth weight) and adverse maternal outcomes (eg, preeclampsia, congestive heart failure, stillbirth, and abortion).
The pharmacokinetic properties of propylthiouracil are not significantly changed by pregnancy; however, the severity of hyperthyroidism may fluctuate throughout pregnancy (De Groot 2012; Sitar 1979; Sitar 1982). Doses of propylthiouracil may be decreased as pregnancy progresses and discontinued weeks to months prior to delivery.
Antithyroid drugs are the treatment of choice for the control of hyperthyroidism during pregnancy (ACOG 148 2015; Alexander 2017; De Groot 2012). [US Boxed Warning]: Propylthiouracil may be the treatment of choice when an antithyroid drug is indicated during or just prior to the first trimester of pregnancy. Due to adverse maternal events, other antithyroid medications should be considered after the first trimester. To prevent adverse outcomes, maternal TT4/FT4 should be at or just above the pregnancy specific upper limit of normal (Alexander 2017). Propylthiouracil may be used for the treatment of thyroid storm in pregnant females (ACOG 148 2015).
Females taking propylthiouracil should notify their health care provider immediately once pregnancy is suspected (Alexander 2017).
Patient Education
What is this drug used for?
- It is used to treat an overactive thyroid gland.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Abdominal pain
- Fatigue
- Hair loss
- Muscle pain
- Joint pain
- Change in taste
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Bruising
- Bleeding
- Severe headache
- Severe dizziness
- Passing out
- Severe loss of strength and energy
- Shortness of breath
- Swollen glands
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Low thyroid level like constipation; difficulty handling heat or cold; memory problems; mood changes; or burning, numbness, or tingling feeling.
- Lupus like rash on the cheeks or other body parts, sunburn easy, muscle or joint pain, chest pain or shortness of breath, or swelling in the arms or legs.
- Infection
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.