Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Generic: 500 mg
Pharmacology
Mechanism of Action
Converted to pyrazinoic acid in susceptible strains of Mycobacterium which lowers the pH of the environment; exact mechanism of action has not been elucidated
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed
Distribution
Widely into body tissues and fluids including liver, lung, and CSF
Relative diffusion from blood into CSF: Adequate with or without inflammation (exceeds usual MICs)
CSF:blood level ratio: Inflamed meninges: 100%
Metabolism
Hepatic
Excretion
Urine (4% as unchanged drug)
Time to Peak
Serum: Within 2 hours
Half-Life Elimination
9 to 10 hours, prolonged with reduced renal or hepatic function
Protein Binding
50%
Use: Labeled Indications
Tuberculosis: Adjunctive treatment of tuberculosis (TB) in combination with other antituberculosis agents
Contraindications
Hypersensitivity to pyrazinamide or any component of the formulation; acute gout; severe hepatic damage
Dosage and Administration
Dosing: Adult
Tuberculosis, treatment (drug-susceptible): Oral: Note: Always administer in combination with other antitubercular drugs (Nahid 2016).
ATS/CDC/IDSA drug-sensitive tuberculosis guideline recommendations (Nahid 2016):
Dosing: Doses should be based on lean body weight for patients within a normal weight range for their height (optimal dosing for obese patients has not been established) (Nahid 2016):
Once-daily therapy:
40 to 55 kg: 1,000 mg once daily Note: The preferred frequency of administration is once daily; however, 5-days per week administration by directly-observed therapy (DOT) is an acceptable alternative (Nahid 2016).
56 to 75 kg: 1,500 mg once daily
76 to 90 kg: 2,000 mg once daily
Three-times-weekly DOT:
40 to 55 kg: 1,500 mg 3 times weekly
56 to75 kg: 2,500 mg 3 times weekly
76 to 90 kg: 3,000 mg 3 times weekly
Twice-weekly DOT:
40 to 55 kg: 2,000 mg twice weekly
56 to 75 kg: 3,000 mg twice weekly
76 to 90 kg: 4,000 mg twice weekly
Regimens: Treatment regimens for pulmonary tuberculosis and tuberculous meningitis consist of an initial 2-month phase of a 4-drug regimen that includes pyrazinamide, followed by a continuation phase of a 2-drug regimen (does not include pyrazinamide) of an additional 4 to 7 months for pulmonary tuberculosis and a continuation phase of an additional 7 to 10 months of a 2-drug regimen (does not include pyrazinamide) for tuberculous meningitis (optimal duration is not defined although continuation phase must continue for a minimum of 7 additional months). Adjunctive corticosteroid therapy (eg, dexamethasone, prednisolone) tapered over 6 to 8 weeks is also recommended for tuberculous meningitis; pyrazinamide frequency and dosing differs depending on treatment regimen selected; consult current drug-sensitive TB guidelines (Nahid 2016).
Dosing: Pediatric
Note: Recommendations often change due to epidemiology (resistance) and emerging information; consult CDC and WHO for current recommendations, as appropriate.
Active TB infection, treatment: Note: Always use as part of a multidrug regimen. Any regimens using less than once daily dosing should administer dosing as directly observed therapy (DOT). Treatment regimens for pulmonary tuberculosis consist of an initial 2-month intensive phase of a 4-drug regimen, followed by a continuation phase of an additional 4 to 7 months of isoniazid and rifampin. Pyrazinamide frequency and dosing differs depending on treatment regimen selected; consult current drug-sensitive TB guidelines for detailed information (ATS/CDC/IDSA [Nahid 2016]).
ATS/CDC/IDSA Recommendations (ATS/CDC/IDSA [Nahid 2016]):
Once daily or 5-times-weekly (DOT):
Infants, Children, and Adolescents weighing <40 kg: Oral: 35 mg/kg/dose once daily or 5 times weekly DOT; suggested range: 30 to 40 mg/kg/dose
Children and Adolescents weighing ≥40 kg: Note: Doses should be based on lean body weight for patients within a normal weight range for their height (optimal dosing for obese patients has not been established): Oral: Weight-band dosing for whole tablets:
40 to 55 kg: 1,000 mg (18.2 to 25 mg/kg/dose) once daily or 5-times-weekly (DOT)
56 to 75 kg: 1,500 mg (20 to 28.6 mg/kg/dose) once daily or 5-times-weekly (DOT)
76 to 90 kg: 2,000 mg (22.2 to 26.3 mg/kg/dose) once daily or 5-times-weekly (DOT)
Three-times-weekly DOT: Note: Although suggested dosing based on experience with twice-weekly regimen; experts suggest three-times-weekly regimens are more effective than twice-weekly DOT regimens; pyrazinamide-containing three-times-weekly DOT may be used as part of an intensive phase; consult guidelines for specific information
Infants, Children, and Adolescents weighing <40 kg: Oral: 50 mg/kg/dose three times weekly
Children and Adolescents weighing ≥40 kg: Note: Doses should be based on lean body weight for patients within a normal weight range for their height (optimal dosing for obese patients has not been established) Oral: Weight-band dosing for whole tablets:
40 to 55 kg: 1,500 mg (27.3 to 37.5 mg/kg/dose) three-times-weekly
56 to 75 kg: 2,500 mg (33.3 to 44.6 mg/kg/dose) three-times-weekly
76 to 90 kg: 3,000 mg (33.3 to 39.5 mg/kg/dose) three-times-weekly
Twice-weekly DOT: Note: Regimen not generally recommended; do not use in HIV patients or those with smear-positive and/or cavitary disease. This therapy should only be used following completion of a 2-week intensive phase once-daily (or 5-times-weekly) regimen. Missed doses result in the equivalent of once-weekly dosing which has been shown to be inferior and is associated with treatment failure, relapse, and development of drug resistance.
Infants, Children, and Adolescents weighing <40 kg: Oral: 50 mg/kg/dose twice weekly
Children and Adolescents weighing >40 kg: Oral:
40 to 55 kg: 2,000 mg (36.4 to 50 mg/kg/dose) twice weekly
56 to 75 kg: 3,000 mg (40 to 53.6 mg/kg/dose) twice weekly
76 to 90 kg: 4,000 mg (44.4 to 52.6 mg/kg/dose) twice weekly
Extemporaneously Prepared
100 mg/mL Oral Suspension (ASHP Standard Concentration) (ASHP 2017)
A 100 mg/mL oral suspension may be made with tablets. Crush two-hundred pyrazinamide 500 mg tablets and mix with a suspension containing 500 mL methylcellulose 1% and 500 mL simple syrup. Add to this a suspension containing one-hundred forty crushed pyrazinamide tablets in 350 mL methylcellulose 1% and 350 mL simple syrup to make 1.7 L suspension. Label "shake well" and "refrigerate". Stable for 60 days refrigerated (preferred) and 45 days at room temperature.
Nahata MC, Morosco RS, and Peritre SP, “Stability of Pyrazinamide in Two Suspensions,” Am J Health Syst Pharm, 1995, 52(14):1558-60.7552903
Storage
Store at controlled room temperature of 15°C to 30°C (59°F to 86°F).
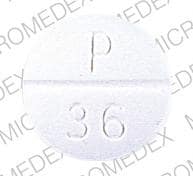
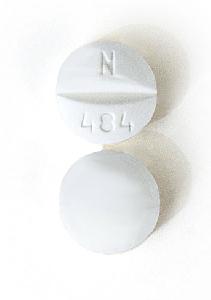
Pyrazinamide Images
Drug Interactions
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Benzbromarone: Pyrazinamide may diminish the therapeutic effect of Benzbromarone. Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
CycloSPORINE (Systemic): Pyrazinamide may decrease the serum concentration of CycloSPORINE (Systemic). Monitor therapy
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
RifAMPin: Pyrazinamide may enhance the hepatotoxic effect of RifAMPin. Severe (even fatal) liver injury has been reported in patients receiving these 2 drugs as a 2-month treatment regimen for latent TB infection. Consider therapy modification
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Test Interactions
Reacts with Acetest® and Ketostix® to produce pinkish-brown color
Adverse Reactions
1% to 10%:
Central nervous system: Malaise
Gastrointestinal: Anorexia, nausea, vomiting
Neuromuscular & skeletal: Arthralgia, myalgia
<1%, postmarketing, and/or case reports: Acne vulgaris, acquired blood coagulation disorder (anticoagulant effect), angioedema (rare), dysuria, fever, gout, hepatotoxicity, interstitial nephritis, porphyria, pruritus, sideroblastic anemia, skin photosensitivity, skin rash, thrombocytopenia, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Hepatotoxicity: Dose-related hepatotoxicity ranging from transient ALT/AST elevations to jaundice, hepatitis and/or liver atrophy (rare) has occurred.
Disease-related concerns:
- Alcoholism: Due to concerns for preexisting hepatic dysfunction, use with caution in patients with a history of alcoholism (even if ethanol consumption is discontinued during therapy).
- Diabetes: Use with caution in patients with diabetes mellitus.
- Gout: May inhibit uric acid excretion; acute gouty attacks have been reported. Use with caution in patients with chronic gout; contraindicated with acute gout.
- Porphyria: Use with caution in patients with porphyria.
- Renal impairment: Use with caution in patients with renal failure.
Concurrent drug therapy issues:
- Hepatotoxic agents: Use with caution in patients receiving concurrent medications associated with hepatotoxicity (particularly with rifampin). The 2-month rifampin-pyrazinamide regimen for the treatment of latent tuberculosis infection (LTBI) has been associated with severe and fatal liver injuries; incidence increased with pyrazinamide doses >30 mg/kg/day. The Infectious Diseases Society of America and Centers for Disease Control and Prevention recommend that the 2-month rifampin-pyrazinamide regimen should not generally be used in patients with LTBI.
Monitoring Parameters
Periodic liver function tests, serum uric acid, sputum culture, chest x-ray 2-3 months into treatment and at completion
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events have not been observed in animal reproduction studies. Due to the risk of tuberculosis to the fetus, treatment is recommended when the probability of maternal disease is moderate to high. Drug-susceptible TB guidelines recommend pyrazinamide as part of the initial treatment regimen; however, risks and benefits of use during pregnancy should be considered for each individual patient (Nahid 2016).
Patient Education
What is this drug used for?
- It is used to treat TB (tuberculosis). This drug is used with other drugs. Talk with your doctor.
Frequently reported side effects of this drug
- Muscle pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Joint pain
- Joint swelling
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.