Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Intravenous, as bromide:
Regonol: 10 mg/2 mL (2 mL) [contains benzyl alcohol]
Solution, Oral, as bromide:
Mestinon: 60 mg/5 mL (473 mL) [contains alcohol, usp, brilliant blue fcf (fd&c blue #1), fd&c red #40, sodium benzoate; raspberry flavor]
Generic: 60 mg/5 mL (5 mL, 473 mL)
Tablet, Oral, as bromide:
Mestinon: 60 mg [scored]
Generic: 30 mg, 60 mg
Tablet Extended Release, Oral, as bromide:
Mestinon: 180 mg [scored]
Generic: 180 mg
Pharmacology
Mechanism of Action
Inhibits destruction of acetylcholine by acetylcholinesterase which facilitates transmission of impulses across neuromuscular junction
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Very poor (10% to 20%)
Distribution
Vd: 0.53 to 1.76 L/kg (Aquilonius 1986)
Metabolism
Hepatic and at tissue site by cholinesterases
Excretion
Urine (80% to 90% as unchanged drug) (Aquilonius 1986)
Onset of Action
Recovery from vincristine neurotoxicity: Onset of action: 1 to 2 weeks (Akbayram 2010)
Myasthenia gravis: Oral: Within 30 minutes (Maggi 2011); IM: 15 to 30 minutes; IV: Within 2 to 5 minutes
Time to Peak
Oral: 1 to 2 hours (Aquilonius 1986)
Duration of Action
Oral: 3 to 4 hours in the daytime (Maggi 2011); IM, IV: 2 to 3 hours
Half-Life Elimination
Oral: 1 to 2 hours; renal failure: ~6 hours (Aquilonius 1986)
IV: ~1.5 hours (Aquilonius 1980)
Protein Binding
None (Aquilonius 1986)
Use: Labeled Indications
Myasthenia gravis (oral only): Treatment of myasthenia gravis.
Reversal of nondepolarizing muscle relaxants (injection only): Reversal agent or antagonist to the neuromuscular blocking effects of nondepolarizing muscle relaxants.
Military use: Pretreatment for Soman nerve gas exposure
Use: Off Label
Disopyramide-induced anticholingeric adverse effectsb
Data from a double-blind, randomized crossover study in patients treated with disopyramide supports the use of sustained-release pyridostigmine to mitigate anticholinergic adverse effects (eg, urinary retention, constipation, dry mouth) associated with the use of disopyramide without affecting its electrophysiologic or antiarrhythmic properties Teichman 1987. Clinical experience also suggests the utility of pyridostigmine for this purpose Sherrid 2016, Verlinden 2015.
Myasthenia gravis (IM, IV use)c
Clinical experience suggests the utility of IM or IV pyridostigmine in managing this condition Maggi 2011. A continuous infusion has been employed for some patients experiencing myasthenic crisis Berrouschot 1997, Saltis1993. Additional data may be necessary to further define the role of pyridostigmine in this condition.
Contraindications
Hypersensitivity to pyridostigmine, anticholinesterase agents, or any component of the formulation; mechanical intestinal or urinary obstruction
Documentation of allergenic cross-reactivity for anticholinergic muscle stimulants is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Myasthenia gravis:
Oral: Highly individualized dosing ranges:
Immediate-release: 60 to 1,500 mg/day, usually 600 mg/day divided into 5 to 6 doses, spaced to provide maximum relief
Sustained release: 180 to 540 mg once or twice daily (doses separated by at least 6 hours); Note: It may be necessary to use immediate-release therapy in conjunction with sustained-release therapy.
IM, IV (off-label use): To supplement during labor and postpartum, during myasthenic crisis, or when oral therapy is impractical: ~1/30th of oral dose; observe patient closely for cholinergic reactions. IM route preferred due to significant complications (eg, cardiac arrest) observed with the IV route (Maggi 2011; Varner 2013). May also administer as a continuous infusion for myasthenic crisis.
Continuous infusion: IV: 1 to 2 mg/hour with gradual titration in increments of 0.5 to 1 mg/hour, up to a maximum rate of 4 mg/hour (Berrouschot 1997; Saltis 1993)
Reversal of nondepolarizing muscle relaxants: IV: 0.1 to 0.25 mg/kg/dose (onset to peak effect is dose-dependent; return of twitch height to 90% of control occurs within ~6 minutes; full recovery usually occurs within 15 to 30 minutes)
Note: The monitoring of muscle twitch response to peripheral nerve stimulation is advised; administer pyridostigmine after spontaneous recovery of neuromuscular function has begun. Atropine sulfate or glycopyrrolate IV should be administered immediately prior to or simultaneously with pyridostigmine to minimize side effects. Inadequate reversal is possible; manage by manual or mechanical ventilation until recovery is judged adequate (additional doses are not recommended).
Soman nerve gas exposure, pretreatment (military use): Note: Do not administer pyridostigmine after Soman exposure; if taken immediately before exposure (eg, when gas attack alarm is given) or at the same time, it is not expected to be effective and may exacerbate the effects of a sub-lethal exposure to Soman.
Oral: 30 mg every 8 hours beginning several hours prior to exposure; discontinue at first sign of Soman exposure, then immediately begin atropine and pralidoxime.
Disopyramide-induced anticholingeric adverse effects (off-label use): Oral: Sustained release: 90 to 180 mg every 12 hours or as needed (Sherrid 2013; Sherrid 2016; Teichman 1987)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: All pediatric dosing recommendations based on immediate release product formulations. Dosage should be individualized based on patient response.
Myasthenic syndromes, congenital: Limited data available: Infants, Children, and Adolescents: Oral: 1 mg/kg/dose every 4 hours; usual range: 4 to 5 mg/kg/day in 4 to 6 divided doses; maximum daily dose: 7 mg/kg/day divided in 5-6 doses (Kliegman, 2011; Lorenzoni, 2012)
Myasthenia gravis, autoimmune (juvenile): Limited data available: Infants, Children, and Adolescents: Note: Dosage should be adjusted such that larger doses administered prior to time of greatest fatigue.
Oral: 1 mg/kg/dose every 4-6 hours; maximum daily dose: 7 mg/kg/day divided in 5-6 doses; usual daily dose: 600 mg/day; doses as high as 1500 mg/day have been used (Andrews, 1998; Maggi, 2011)
IM, IV: 0.05-0.15 mg/kg/dose; maximum dose: 10 mg (Kliegman, 2007)
Reversal of nondepolarizing neuromuscular blocker: Limited data available: Infants, Children, and Adolescents: IM, IV: 0.1-0.25 mg/kg/dose (Kliegman, 2007). Note: Give atropine or glycopyrrolate immediately prior to minimize side effects.
Vincristine-induced neurotoxicity: Limited data available: Children ≥2 years and Adolescents: Oral: 3 mg/kg/day divided in 2 doses, given with pyridoxine for 3 weeks; dosing based on a case series of four children (age: 2-13 years) receiving vincristine for treatment of ALL (Akbayram, 2010) and a 2-year old receiving vincristine for a cervical synovial sarcoma (Muller, 2004)
Reconstitution
Myasthenic crisis (off-label use): Continuous infusion: May dilute 25 mg in 100 mL of D5W (Saltis 1993).
Administration
Oral: Do not crush extended release tablet.
IV: For myasthenic crisis (off-label use), may administer IM, slow IV push, or as a continuous infusion (Maggi 2011; Saltis 1993).
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F); protect from moisture.
Military use: Store between 2°C and 8°C (36°F to 46°F); protect from light. Discard 3 months after issue. Do not dispense after removal from the refrigerator for more than a total of 3 months.
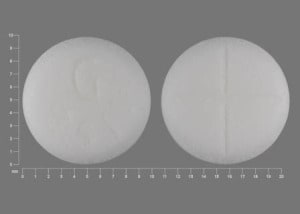
Pyridostigmine Images
Drug Interactions
Amifampridine: Acetylcholinesterase Inhibitors may enhance the therapeutic effect of Amifampridine. Amifampridine side effects may also be increased. Amifampridine may enhance the therapeutic effect of Acetylcholinesterase Inhibitors. Acetylcholinesterase inhibitor side effects may also be increased. Monitor therapy
Anticholinergic Agents: Acetylcholinesterase Inhibitors may diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Benoxinate: Acetylcholinesterase Inhibitors may enhance the therapeutic effect of Benoxinate. Specifically, the effects of benoxinate may be prolonged. Monitor therapy
Beta-Blockers: Acetylcholinesterase Inhibitors may enhance the bradycardic effect of Beta-Blockers. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Cholinergic Agonists: Acetylcholinesterase Inhibitors may enhance the adverse/toxic effect of Cholinergic Agonists. Monitor therapy
Corticosteroids (Systemic): May enhance the adverse/toxic effect of Acetylcholinesterase Inhibitors. Increased muscular weakness may occur. Monitor therapy
Dipyridamole: May diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Methocarbamol: May diminish the therapeutic effect of Pyridostigmine. Monitor therapy
Neuromuscular-Blocking Agents (Nondepolarizing): Acetylcholinesterase Inhibitors may diminish the neuromuscular-blocking effect of Neuromuscular-Blocking Agents (Nondepolarizing). Monitor therapy
Succinylcholine: Acetylcholinesterase Inhibitors may increase the serum concentration of Succinylcholine. Management: Consider alternatives to this combination due to a risk of prolonged neuromuscular blockade. Consider therapy modification
Adverse Reactions
1% to 10%:
Central nervous system: Twitching (3%), hyperesthesia (2%)
Dermatologic: Xeroderma (2%)
Gastrointestinal: Abdominal pain (7%), diarrhea (7%)
Genitourinary: Dysmenorrhea (5%), urinary frequency (2%)
Neuromuscular & skeletal: Myalgia (2%), neck pain (2%)
Ophthalmic: Amblyopia (2%)
Respiratory: Epistaxis (2%)
Frequency not defined:
Cardiovascular: Bradycardia (transient), chest tightness, decreased heart rate, increased blood pressure
Central nervous system: Confusion, depressed mood, disturbed sleep, drowsiness, headache, hypertonia, lack of concentration, lethargy, localized warm feeling, numbness of tongue, tingling of extremities, vertigo
Dermatologic: Alopecia, diaphoresis, skin rash
Gastrointestinal: Abdominal cramps, bloating, borborygmi, flatulence, increased peristalsis, nausea, salivation, vomiting
Hypersensitivity: Hypersensitivity reaction
Neuromuscular & skeletal: Fasciculations, muscle cramps, weakness
Ophthalmic: Eye pain, lacrimation, miosis, visual disturbance
Respiratory: Acute bronchitis (exacerbation), exacerbation of asthma, increased bronchial secretions
<1%, postmarketing, and/or case reports: Fecal incontinence, loss of consciousness, pallor (postsyncopal), stiffness (arms or upper torso), thrombophlebitis, urinary incontinence
Warnings/Precautions
Concerns related to adverse effects:
- Cholinergic effects: Symptoms of excess cholinergic activity may occur (eg, salivation, sweating, urinary incontinence). Overdosage may result in cholinergic crisis (eg, muscle weakness), which must be distinguished from myasthenic crisis; discontinue immediately in the presence of cholinergic crisis.
- Hypersensitivity reactions: May occur; have atropine and epinephrine ready to treat hypersensitivity reactions.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with bradycardia or other cardiac arrhythmias.
- Glaucoma: Use with caution; additive effect with antiglaucoma drugs may cause or exacerbate problems with night vision.
- Renal impairment: Use with caution in patients with renal impairment; initial lower doses may be needed; titrate to effect.
- Respiratory disease: Use with extreme caution in patients with asthma, bronchospastic disease, or COPD.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Bromide sensitivity: Use with caution in patients with bromide sensitivity.
- Pediatrics: Injection not indicated for use in neonates; may contain benzyl alcohol which has been associated with "gasping syndrome" in neonates.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer's labeling.
- Injection: Must be administered by trained personnel; use of peripheral nerve stimulation to monitor neuromuscular function recovery and continuous patient observation until recovery of normal respiration is recommended. To counteract anticholinergic effects, use of glycopyrrolate or atropine sulfate simultaneously with or prior to administration is recommended. May contain benzyl alcohol which has been associated with "gasping syndrome" in neonates.
- Oral: Adequate facilities should be available for cardiopulmonary resuscitation when testing and adjusting dose for myasthenia gravis.
Other warnings/precautions:
- Inadequate reversal of nondepolarizing muscle relaxants: Inadequate reversal induced by nondepolarizing muscle relaxants is possible; manage with manual or mechanical ventilation until recovery is adequate (additional doses not recommended). Failure to produce prompt (within 30 minutes) reversal of neuromuscular blockade may occur in the presence of extreme debilitation, carcinomatosis, or with concomitant use of certain broad-spectrum antibiotics, or anesthetic agents and other drugs which enhance neuromuscular blockade or cause respiratory depression.
- Military use: Only for pretreatment for exposure to Soman; discontinue pyridostigmine at the first sign of Soman exposure (do not administer pyridostigmine after Soman exposure); atropine and pralidoxime must be administered after Soman exposure (pyridostigmine pretreatment offers no benefit against Soman unless atropine and pralidoxime are administered once symptoms of poisoning appear). Use in conjunction with protective garments, including gas mask, hood and overgarments.
Monitoring Parameters
ECG, blood pressure, and heart rate especially with IV use; observe for cholinergic reactions (eg, nausea, vomiting, diarrhea, increased salivation), particularly when administered IV; consult individual institutional policies and procedures
Pregnancy
Pregnancy Risk Factor
B/C (manufacturer dependent)
Pregnancy Considerations
Adverse events have not been observed in animal reproduction studies. Pyridostigmine may cross the placenta (Buckley 1968). Use of pyridostigmine may be continued during pregnancy for the treatment of myasthenia gravis (Norwood 2014; Skeie 2010) and its use should be continued during labor (Norwood 2014). Transient neonatal myasthenia gravis may occur in 10% to 20% of neonates due to placental transfer of maternal antibodies (Skeie 2010; Varner 2013).
In general, medications used as antidotes should take into consideration the health and prognosis of the mother; antidotes should be administered to pregnant women if there is a clear indication for use and should not be withheld because of fears of teratogenicity (Bailey 2003).
Patient Education
What is this drug used for?
All oral products:
- It is used to treat myasthenia gravis.
Injection:
- It is used to get back function in muscles after surgery.
All products:
- It may be given to you for other reasons. Talk with the doctor.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Difficulty breathing
- Slow heartbeat
- Nausea
- Vomiting
- Abdominal cramps
- Diarrhea
- Drooling
- Small pupils
- Sweating a lot
- Muscle cramps
- Twitching
- Weakness
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.