Boxed Warning
Nocturnal leg cramps:
Quinine use for the treatment or prevention of nocturnal leg cramps may result in serious and life-threatening hematologic reactions, including thrombocytopenia and hemolytic uremic syndrome/thrombotic thrombocytopenic purpura (TTP). Chronic renal impairment associated with the development of TTP has been reported. The risk associated with quinine use in the absence of evidence of its effectiveness in the treatment or prevention of nocturnal leg cramps outweighs any potential benefit.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
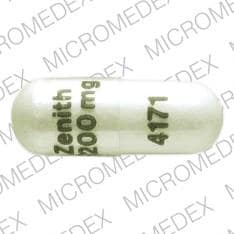
Capsule, Oral, as sulfate:
Qualaquin: 324 mg
Generic: 324 mg
Pharmacology
Mechanism of Action
Depresses oxygen uptake and carbohydrate metabolism; intercalates into DNA, disrupting the parasite's replication and transcription; cardiovascular effects similar to quinidine
Pharmacokinetics/Pharmacodynamics
Absorption
Readily, mainly from upper small intestine
Distribution
Adults: 2.5 to 7.1 L/kg (varies with severity of infection); Children: ~0.9 L/kg (subjects with malaria)
Intraerythrocytic levels are ~30% to 50% of the plasma concentration; distributes poorly to the CSF (~2% to 7% of plasma concentration)
Metabolism
Hepatic via CYP450 enzymes, primarily CYP3A4; forms metabolites; major metabolite, 3-hydroxyquinine, is less active than parent
Excretion
Urine (~20% as unchanged drug); renal excretion is twofold in the presence of acidic urine
Time to Peak
Children: Serum: 2 hours in healthy subjects; 4 hours with malaria
Adults: Serum: 2 to 4 hours in healthy subjects; 1 to 11 hours with malaria
Half-Life Elimination
Children: ~3 hours in healthy subjects; ~12 hours with malaria
Healthy adults: 10 to 13 hours
Healthy elderly subjects: 18 hours
Protein Binding
69% to 92% in healthy subjects; 78% to 95% with malaria (due to increase in alpha1-acid glycoprotein)
Use in Specific Populations
Special Populations: Renal Function Impairment
The effects of mild and moderate renal impairment on the pharmacokinetics and efficacy of quinine are not known. The plasma half-life is prolonged to 26 hours in patients with severe long-term renal impairment; dosage adjustment needed.
Special Populations: Hepatic Function Impairment
AUC increased 55% without a significant change in Cmax in patients with moderate hepatic impairment. Plasma elimination half-life and volume of distribution are increased in patients with severe hepatic impairment.
Special Populations: Elderly
Mean AUC is ~38% higher in healthy subjects 65 to 78 years of age compared with subjects 20 to 35 years of age. Mean Tmax and Cmax are similar in elderly and younger subjects. Mean oral clearance is decreased and mean elimination half-life is increased in elderly compared with younger subjects. The proportion of quinine excreted unchanged in the urine is larger in elderly compared with younger subjects. Despite these pharmacokinetic differences, no alteration in dosage is needed.
Use: Labeled Indications
Malaria, uncomplicated, due to Plasmodium falciparum (treatment): Treatment of uncomplicated chloroquine-resistant P. falciparum malaria, in combination with other antimalarial agents
Use: Off Label
Babesiosiscyes
Clinical experience suggests the utility of quinine (in combination with clindamycin) for the treatment of Babesia microti infection Vannier 2012.
Based on the Infectious Diseases Society of America (IDSA) guidelines for the Clinical Assessment, Treatment, and Prevention of Lyme Disease, Human Granulocytic Anaplasmosis, and Babesiosis, quinine (in combination with clindamycin) is an effective and recommended initial therapy in the treatment of babesiosis.
Malaria, uncomplicated, due to Plasmodium vivax (treatment)yes
Based on the Centers for Disease Control and Prevention (CDC) Guidelines for Treatment of Malaria in the United States, quinine (in combination with other antimalarial agents) is effective and recommended in the treatment of uncomplicated chloroquine-resistant P. vivax malaria.
Contraindications
Hypersensitivity to quinine or any component of the formulation; hypersensitivity to mefloquine or quinidine (cross sensitivity reported); history of potential hypersensitivity reactions (including blackwater fever, immune thrombocytopenia (formerly known as idiopathic thrombocytopenic purpura), thrombotic thrombocytopenic purpura [TTP], hemolytic uremic syndrome [HUS], or thrombocytopenia) associated with prior quinine use; prolonged QT interval; myasthenia gravis; optic neuritis.
Dosage and Administration
Dosing: Adult
Note: Dosage expressed in terms of the salt; 1 capsule Qualaquin = 324 mg of quinine sulfate = 269 mg of base; Canadian products contain 200 mg of quinine sulfate = 167 mg of base or 300 mg of quinine sulfate = 250 mg of base.
Malaria, uncomplicated, due to chloroquine-resistant P. falciparum (treatment): Oral:
CDC guidelines: 648 mg every 8 hours, in combination with doxycycline, tetracycline, or clindamycin (preferred in pregnancy). Note: Administer quinine for 3 days unless the infection was acquired in Southeast Asia, in which case quinine duration of therapy is 7 days. Duration of concomitant agent is 7 days, regardless of geographic region (CDC 2013).
Canadian product: 600 mg every 8 hours for 3 to 7 days. Note: Use in combination with tetracycline, doxycycline, or clindamycin.
Malaria, uncomplicated, due to chloroquine-resistant P. vivax (treatment) (off-label use): Oral: 648 mg every 8 hours, in combination with doxycycline or tetracycline plus primaquine. Note: Quinine in combination with clindamycin is an alternative regimen for pregnant patients. Administer quinine for 3 days unless the infection was acquired in Southeast Asia, in which case quinine duration of therapy is 7 days. Duration of concomitant agent is 7 days (doxycycline, tetracycline, clindamycin) or 14 days (primaquine), regardless of geographic region (CDC 2013).
Babesiosis (off-label use): Oral: 650 mg every 6 to 8 hours for at least 7 to 10 days with clindamycin (Vannier 2012; Wormser 2006). Relapsing infection may require at least 6 weeks of therapy (Vannier 2012). Note: US manufactured quinine sulfate capsule is 324 mg; 2 capsules (648 mg quinine sulfate) should be sufficient for adult dosing.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dosage expressed in terms of the quinine sulfate salt; 324 mg capsule quinine sulfate = 269 mg of base. Canadian products: 200 mg capsule of quinine sulfate = 167 mg of base or 300 mg capsule of quinine sulfate = 250 mg of base.
Malaria: Children and Adolescents; regardless of HIV status (HHS [OI pediatric 2013]): Limited data available in ages <16 years: Note: Duration of quinine treatment for malaria dependent upon the geographic region or pathogen. Lack of an appropriate quinine dosage form may restrict use in some smaller patients.
P. falciparum (chloroquine resistant), uncomplicated; treatment: Oral: 10 mg/kg/dose quinine sulfate every 8 hours for 3 to 7 days depending on region; maximum dose: 650 mg/dose; use in combination with tetracycline, doxycycline, or clindamycin (dependent upon patient age) (CDC 2013)
P. vivax (chloroquine resistant), uncomplicated; treatment: Oral: 10 mg/kg/dose quinine sulfate every 8 hours for 3 to 7 days depending on region; maximum dose: 650 mg/dose; use in combination with primaquine and tetracycline or doxycycline (dependent upon patient age) (CDC 2013)
Severe malaria: Oral quinine, using the regimens previously described (dose and duration), may be used following IV quinidine including antimicrobial regimen once parasite density is <1% and patient is able to tolerate oral medications (CDC 2013)
Babesiosis: Limited data available: Children and Adolescents: Oral: 10 mg/kg/dose quinine sulfate every 8 hours for 7 to 10 days; maximum dose: 650 mg/dose (Red Book [AAP 2015]; Wittner 1982); use in combination with clindamycin as a first-line treatment option (IDSA [Wormser 2006])
Administration
Avoid use of aluminum- or magnesium-containing antacids because of drug absorption problems. Swallow dose whole to avoid bitter taste. May be administered with food.
Dietary Considerations
Take with food to decrease incidence of gastric upset.
Storage
Store at 20°C to 25°C (68°F to 77°F).
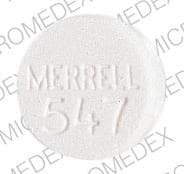
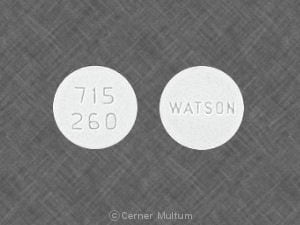
QuiNINE Images
Drug Interactions
Afatinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Afatinib. Management: Reduce afatinib by 10 mg if not tolerated. Some non-US labeling recommends avoiding combination if possible. If used, administer the P-gp inhibitor simultaneously with or after the dose of afatinib. Consider therapy modification
Alkalinizing Agents: May increase the serum concentration of QuiNINE. Monitor therapy
Amiodarone: QT-prolonging Miscellaneous Agents (Highest Risk) may enhance the QTc-prolonging effect of Amiodarone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Amisulpride: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Amisulpride. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Androgens: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Exceptions: Danazol. Monitor therapy
Antacids: May decrease the serum concentration of QuiNINE. Exceptions: Calcium Carbonate; Potassium Bicarbonate; Sodium Bicarbonate. Avoid combination
Antidiabetic Agents: May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Antihepaciviral Combination Products: May increase the serum concentration of QuiNINE. Avoid combination
Antipsychotic Agents (Phenothiazines): Antimalarial Agents may increase the serum concentration of Antipsychotic Agents (Phenothiazines). Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Arsenic Trioxide: QT-prolonging Miscellaneous Agents (Highest Risk) may enhance the QTc-prolonging effect of Arsenic Trioxide. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Artemether: May enhance the adverse/toxic effect of Antimalarial Agents. Management: Artemether/Lumefantrine (combination product) should not be used with other antimalarials unless there is no other treatment option. Avoid combination
Astemizole: QT-prolonging Miscellaneous Agents (Highest Risk) may enhance the QTc-prolonging effect of Astemizole. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Azithromycin (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Azithromycin (Systemic). Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Bedaquiline: QT-prolonging Miscellaneous Agents (Highest Risk) may enhance the QTc-prolonging effect of Bedaquiline. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Bepridil: QT-prolonging Miscellaneous Agents (Highest Risk) may enhance the QTc-prolonging effect of Bepridil. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Betrixaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Betrixaban. Management: Decrease the adult betrixaban dose to an initial single dose of 80 mg followed by 40 mg once daily if combined with a P-glycoprotein inhibitor. Consider therapy modification
Bilastine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Bilastine. Management: Consider alternatives when possible; bilastine should be avoided in patients with moderate to severe renal insufficiency who are receiving p-glycoprotein inhibitors. Consider therapy modification
Blood Pressure Lowering Agents: Herbs (Hypotensive Properties) may enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brentuximab Vedotin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be increased. Monitor therapy
CarBAMazepine: May decrease the serum concentration of QuiNINE. QuiNINE may increase the serum concentration of CarBAMazepine. Consider therapy modification
Celiprolol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Celiprolol. Monitor therapy
Chloroquine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Chloroquine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
ChlorproMAZINE: QT-prolonging Miscellaneous Agents (Highest Risk) may enhance the QTc-prolonging effect of ChlorproMAZINE. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Cimetidine: May increase the serum concentration of QuiNINE. Management: Consider using an alternative H2-receptor antagonist (eg, ranitidine) instead of cimetidine due to a lower interaction risk. If combined, monitor patients closely for signs and symptoms of quinine toxicity. Consider therapy modification
Cisapride: QT-prolonging Miscellaneous Agents (Highest Risk) may enhance the QTc-prolonging effect of Cisapride. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Citalopram: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Citalopram. Avoid combination
Clarithromycin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Clarithromycin. Avoid combination
Clofazimine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Clofazimine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
CloZAPine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of CloZAPine. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Colchicine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Colchicine. Colchicine distribution into certain tissues (e.g., brain) may also be increased. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a p-glycoprotein inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. See full monograph for details. Consider therapy modification
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP2D6 Substrates (High risk with Inhibitors): QuiNINE may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Dabigatran Etexilate: P-glycoprotein/ABCB1 Inhibitors may increase serum concentrations of the active metabolite(s) of Dabigatran Etexilate. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapsone (Systemic): Antimalarial Agents may enhance the adverse/toxic effect of Dapsone (Systemic). Specifically, concomitant use of antimalarial agents with dapsone may increase the risk of hemolytic reactions. Dapsone (Systemic) may enhance the adverse/toxic effect of Antimalarial Agents. Specifically, concomitant use of dapsone with antimalarial agents may increase the risk for hemolytic reactions. Management: Closely monitor patients for signs/symptoms of hemolytic reactions with concomitant use of dapsone and antimalarial agents, particularly in patients deficient in glucose-6-phosphate dehydrogenase (G6PD), methemoglobin reductase, or with hemoglobin M. Consider therapy modification
Dapsone (Topical): Antimalarial Agents may enhance the adverse/toxic effect of Dapsone (Topical). Specifically, the risk of hemolytic reactions may be increased. Management: Closely monitor for signs/symptoms of hemolytic reactions with concomitant use of topical dapsone and antimalarial agents. Patients with glucose-6-phosphate dehydrogenase deficiency may be at particularly high risk for adverse hematologic effects. Consider therapy modification
Dasatinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Dasatinib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Delamanid: QT-prolonging Miscellaneous Agents (Highest Risk) may enhance the QTc-prolonging effect of Delamanid. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Digoxin: QuiNINE may increase the serum concentration of Digoxin. Monitor therapy
Domperidone: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Domperidone. Avoid combination
Doxepin-Containing Products: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Doxepin-Containing Products. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
DOXOrubicin (Conventional): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to P-glycoprotein inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Dronedarone: QT-prolonging Miscellaneous Agents (Highest Risk) may enhance the QTc-prolonging effect of Dronedarone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Droperidol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Droperidol. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Edoxaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Edoxaban. Management: See full monograph for details. Reduced doses are recommended for patients receiving edoxaban for venous thromboembolism in combination with certain P-gp inhibitors. Similar dose adjustment is not recommended for edoxaban use in atrial fibrillation. Consider therapy modification
Encorafenib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Entrectinib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Erythromycin (Systemic): QT-prolonging Miscellaneous Agents (Highest Risk) may enhance the QTc-prolonging effect of Erythromycin (Systemic). Erythromycin (Systemic) may enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Escitalopram: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Escitalopram. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Everolimus: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Everolimus. Monitor therapy
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Avoid combination
Fingolimod: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias (including TdP) with a continuous overnight ECG when fingolimod is combined with QT prolonging drugs. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Flecainide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Flecainide. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Fluconazole: QT-prolonging Miscellaneous Agents (Highest Risk) may enhance the QTc-prolonging effect of Fluconazole. Fluconazole may enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Flupentixol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Flupentixol. Avoid combination
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosphenytoin: May decrease the serum concentration of QuiNINE. Consider therapy modification
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Gadobenate Dimeglumine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Gadobenate Dimeglumine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Gemifloxacin: May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Gilteritinib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Consider alternatives to this combination. If use is necessary, monitor for QTc interval prolongation and arrhythmias. Consider therapy modification
Halofantrine: May enhance the QTc-prolonging effect of QuiNINE. Avoid combination
Haloperidol: QT-prolonging Miscellaneous Agents (Highest Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Herbs (Hypoglycemic Properties): May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the adverse/toxic effect of other Herbs (Hypotensive Properties). Excessive blood pressure lowering may manifest. Monitor therapy
HMG-CoA Reductase Inhibitors (Statins): QuiNINE may increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Exceptions: Fluvastatin; Pitavastatin; Pravastatin; Rosuvastatin. Monitor therapy
Hypoglycemia-Associated Agents: May enhance the hypoglycemic effect of other Hypoglycemia-Associated Agents. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Inotuzumab Ozogamicin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Inotuzumab Ozogamicin. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Larotrectinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Larotrectinib. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lefamulin: May enhance the QTc-prolonging effect of QT-prolonging CYP3A4 Substrates. Management: Do not use lefamulin tablets with QT-prolonging CYP3A4 substrates. Lefamulin prescribing information lists this combination as contraindicated. Avoid combination
Levofloxacin-Containing Products (Systemic): May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Lofexidine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Lofexidine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Lopinavir: May decrease the serum concentration of QuiNINE. This effect has been seen with lopinavir/ritonavir. The individual contributions of lopinavir and ritonavir to this effect are unclear. Avoid combination
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lumefantrine: Antimalarial Agents may enhance the adverse/toxic effect of Lumefantrine. Management: Artemether/Lumefantrine (combination product) should not be used with other antimalarials unless there is no other treatment option. Avoid combination
Maitake: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Mefloquine: QuiNINE may enhance the adverse/toxic effect of Mefloquine. Specifically, the risk for QTc-prolongation and the risk for convulsions may be increased. Mefloquine may increase the serum concentration of QuiNINE. Management: Avoid concurrent use, and delay administration of mefloquine until at least 12 hours after the last dose of quinine when possible. Avoid combination
Methadone: May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Midostaurin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Midostaurin. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Monoamine Oxidase Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Moxifloxacin (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Moxifloxacin (Systemic). Avoid combination
Naldemedine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naldemedine. Monitor therapy
Naloxegol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naloxegol. Monitor therapy
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Neuromuscular-Blocking Agents: QuiNINE may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents. Avoid combination
Nevirapine: May decrease the serum concentration of QuiNINE. Monitor therapy
Nilotinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Nilotinib. Avoid combination
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
OLANZapine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of OLANZapine. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Ondansetron: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Ondansetron. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Osimertinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Osimertinib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
PAZOPanib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of PAZOPanib. Avoid combination
Pegvisomant: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Pentamidine (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pentamidine (Systemic). Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Substrates: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Exceptions: Loperamide. Monitor therapy
PHENobarbital: QuiNINE may increase the serum concentration of PHENobarbital. PHENobarbital may decrease the serum concentration of QuiNINE. Consider therapy modification
Phenytoin: May decrease the serum concentration of QuiNINE. Consider therapy modification
Pilsicainide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pilsicainide. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Pimozide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pimozide. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Avoid combination
Piperaquine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Piperaquine. Avoid combination
Posaconazole: May increase the serum concentration of QT-prolonging CYP3A4 Substrates. Such increases may lead to a greater risk for proarrhythmic effects and other similar toxicities. Avoid combination
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Probucol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Probucol. Avoid combination
Propafenone: May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Prothionamide: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Prucalopride: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Prucalopride. Monitor therapy
QT-prolonging Agents (Indeterminate Risk - Avoid): May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Agents (Indeterminate Risk - Caution): May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Class IA Antiarrhythmics (Highest Risk): May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Class III Antiarrhythmics (Highest Risk): May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Dronedarone. Consider therapy modification
QT-prolonging Kinase Inhibitors (Highest Risk): May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Miscellaneous Agents (Highest Risk): May enhance the QTc-prolonging effect of QuiNINE. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Arsenic Trioxide; Astemizole; Bedaquiline; Bepridil; ChlorproMAZINE; Cisapride; Delamanid. Consider therapy modification
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Erythromycin (Systemic); Fluconazole; Nilotinib; Ribociclib. Consider therapy modification
QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Miscellaneous Agents (Highest Risk). Exceptions: Clarithromycin. Avoid combination
QUEtiapine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of QUEtiapine. Avoid combination
Quinolones: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Quinolones may diminish the therapeutic effect of Blood Glucose Lowering Agents. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
Ranolazine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Ranolazine. Monitor therapy
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Ribociclib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Ribociclib. Avoid combination
RifAMPin: May decrease the serum concentration of QuiNINE. Avoid combination
RifAXIMin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of RifAXIMin. Monitor therapy
RisperiDONE: QT-prolonging Agents (Highest Risk) may enhance the CNS depressant effect of RisperiDONE. QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of RisperiDONE. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Ritonavir: May decrease the serum concentration of QuiNINE. This effect has been seen with lopinavir/ritonavir. The individual contributions of lopinavir and ritonavir to this effect are unclear. QuiNINE may increase the serum concentration of Ritonavir. Ritonavir may increase the serum concentration of QuiNINE. Avoid combination
Salicylates: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Silodosin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Silodosin. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Sodium Stibogluconate: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Sodium Stibogluconate. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Sparfloxacin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Sparfloxacin. Avoid combination
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Talazoparib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Talazoparib. Management: These listed exceptions are discussed in detail in separate interaction monographs. Monitor therapy
Tegaserod: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Tegaserod. Monitor therapy
Telithromycin: May enhance the QTc-prolonging effect of QuiNINE. Telithromycin may increase the serum concentration of QuiNINE. Management: Concomitant therapy with quinine and telithromycin should be avoided, if possible, due to the risk of elevated quinine serum levels and potential adverse cardiac effects. If combined, monitor for QT prolongation and quinine toxicities. Consider therapy modification
Tetracycline (Systemic): May increase the serum concentration of QuiNINE. Monitor therapy
Theophylline Derivatives: QuiNINE may increase the serum concentration of Theophylline Derivatives. Monitor therapy
Thioridazine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Thioridazine. Avoid combination
Tobacco (Smoked): May decrease the serum concentration of QuiNINE. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Topotecan: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Topotecan. Avoid combination
Ubrogepant: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 50 mg and second dose (if needed) of 50 mg when used with a P-gp inhibitor. Consider therapy modification
Vemurafenib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Vemurafenib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Venetoclax: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Venetoclax. Management: Consider a venetoclax dose reduction by at least 50% in patients requiring concomitant treatment with P-glycoprotein (P-gp) inhibitors. Consider therapy modification
VinCRIStine (Liposomal): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of VinCRIStine (Liposomal). Avoid combination
Vitamin K Antagonists (eg, warfarin): QuiNINE may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Test Interactions
May interfere with urine detection of opioids (false-positive); positive Coombs' [direct]; false elevation of urinary steroids (when assayed by Zimmerman method) and catecholamines; qualitative and quantitative urine dipstick protein assays
Adverse Reactions
Frequency not defined.
Cardiovascular: Appearance of U waves on ECG, atrial fibrillation, atrioventricular block, bradycardia, cardiac arrhythmia, chest pain, flushing, hypersensitivity angiitis, hypotension, nodal rhythm disorder (nodal escape beats), orthostatic hypotension, palpitations, prolonged QT interval on ECG, syncope, tachycardia, torsades de pointes, unifocal premature ventricular contractions, vasodilation, ventricular fibrillation, ventricular tachycardia
Central nervous system: Altered mental status, aphasia, ataxia, chills, coma, confusion, disorientation, dizziness, dystonic reaction, headache, restlessness, seizure, vertigo
Dermatologic: Allergic contact dermatitis, bullous dermatitis, diaphoresis, exfoliative dermatitis, erythema multiforme, pruritus, skin necrosis (acral), skin photosensitivity, skin rash (papular rash, scarlatiniform rash, urticaria), Stevens-Johnson syndrome, toxic epidermal necrolysis
Endocrine & metabolic: Hypoglycemia
Gastrointestinal: Abdominal pain, anorexia, diarrhea, esophagitis, gastric irritation, nausea, vomiting
Genitourinary: Hemoglobinuria
Hematologic & oncologic: Agranulocytosis, aplastic anemia, blood coagulation disorder, bruise, disseminated intravascular coagulation, hemolysis (blackwater fever), hemolytic anemia, hemolytic-uremic syndrome, hemorrhage, hypoprothrombinemia, immune thrombocytopenia (ITP), leukopenia, neutropenia, pancytopenia, petechia, thrombocytopenia, thrombotic thrombocytopenic purpura
Hepatic: Abnormal hepatic function tests, granulomatous hepatitis, hepatitis, jaundice
Hypersensitivity: Hypersensitivity reaction
Immunologic: Antibody development (lupus anticoagulant syndrome)
Neuromuscular & skeletal: Lupus-like syndrome, myalgia, tremor, weakness
Ophthalmic: Blindness, blurred vision (with or without scotomata), diplopia, mydriasis, nocturnal amblyopia, optic neuritis, photophobia, vision color changes, vision loss (sudden), visual field loss
Otic: Auditory impairment, deafness, tinnitus
Renal: Acute interstitial nephritis, renal failure, renal insufficiency
Respiratory: Asthma, dyspnea, pulmonary edema
Miscellaneous: Fever
Warnings/Precautions
Concerns related to adverse effects:
- Hemolytic anemia: Acute hemolytic anemia has been reported, including in patients with G6PD deficiency; causal relationship has not been established. Monitor hemoglobin and hematocrit during use; discontinue therapy if hemolytic anemia develops.
- Hypersensitivity reactions: Severe hypersensitivity reactions (eg, Stevens-Johnson syndrome, anaphylactic shock) have occurred; discontinue following any signs of sensitivity. Other events (including acute interstitial nephritis, neutropenia, and granulomatous hepatitis) may also be attributed to hypersensitivity reactions.
- Hypoglycemia: Use may cause significant hypoglycemia due to quinine-induced insulin release.
- Thrombocytopenia: Immune-mediated thrombocytopenia, including life-threatening cases and immune thrombocytopenia, has occurred with use. Chronic renal failure associated with TTP has also been reported. Thrombocytopenia generally resolves within a week upon discontinuation. Re-exposure may result in increased severity of thrombocytopenia and faster onset.
Disease-related concerns:
- Altered cardiac conduction: Use with caution in patients with atrial fibrillation or flutter (paradoxical increase in heart rate may occur). Use with caution in patients with clinical conditions which may prolong the QT interval or cause cardiac arrhythmias. Quinine may cause QT-interval prolongation, with maximum increase corresponding to maximum plasma concentration. Fatal torsade de pointes and ventricular fibrillation has been reported. Use contraindicated in patients with QT prolongation. Concurrent use of Class IA (eg, quinidine, procainamide) or Class III (eg, amiodarone, dofetilide, sotalol) antiarrhythmic agents or with other drugs known to prolong the QT interval is not recommended. Quinine may also cause concentration-dependent prolongation of the PR and QRS intervals. Risk of prolonged PR and/or QRS intervals is higher in patients with underlying structural heart disease, myocardial ischemia, preexisting conduction system abnormalities, elderly patients with sick sinus syndrome, patients with atrial fibrillation with slow ventricular response and concomitant use of drugs known to prolong the PR interval (eg, verapamil) or QRS interval (eg, flecainide or quinidine).
- Hepatic impairment: Use with caution in patients with mild to moderate hepatic impairment. Avoid in patients with severe hepatic impairment.
- Renal impairment: Use with caution in patients with renal impairment; dosage adjustment recommended in severe chronic impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information
Other warnings/precautions:
- Appropriate use: Quinine should not be used for the prevention of malaria or in the treatment of complicated or severe P. falciparum malaria (oral antimalarial agents are not appropriate for initial therapy of severe malaria).
- Nocturnal leg cramps: [US Boxed Warning]: Quinine is not recommended for the prevention/treatment of nocturnal leg cramps due to the potential for severe and/or life-threatening side effects (eg, cardiac arrhythmias, thrombocytopenia, and HUS/TTP, severe hypersensitivity reactions). These risks, as well as the absence of clinical effectiveness, do not justify its use in the unapproved/off-label prevention and/or treatment of leg cramps.
Monitoring Parameters
Monitor CBC with platelet count, liver function tests, blood glucose; ECG; ophthalmologic examination
Pregnancy
Pregnancy Considerations
Quinine crosses the human placenta. Cord plasma to maternal plasma quinine ratios have been reported as 0.18 to 0.46 and should not be considered therapeutic to the infant.
Based on available data, therapeutic doses used for malaria are not associated with an increased risk of adverse fetal events. Quinine may cause significant maternal hypoglycemia and an increased risk of other adverse maternal events, including dizziness, nausea, tinnitus, and vomiting.
Untreated malaria is also associated with adverse fetal and maternal outcomes. Malaria infection in pregnant women may be more severe than in nonpregnant women. Because P. falciparum malaria can cause maternal death and fetal loss, pregnant women traveling to malaria-endemic areas must use personal protection against mosquito bites. Quinine may be used for the treatment of malaria in pregnant women; consult current CDC guidelines.
A decrease in sperm motility and an increase in abnormal sperm morphology was observed in men receiving quinine.
Patient Education
What is this drug used for?
- It is used to treat malaria.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Diarrhea
- Lack of appetite
- Dizziness
- Headache
- Noise or ringing in the ears
- Change in hearing
- Flushing
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in your urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Kidney problems like not able to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating
- Lupus like rash on the cheeks or other body parts, sunburn easy, muscle or joint pain, chest pain or shortness of breath, or swelling in the arms or legs
- Thrombotic thrombocytopenic purpura/hemolytic uremic syndrome like bruising or bleeding; severe loss of strength and energy; dark urine or yellow skin; pale skin; change in amount of urine passed; vision changes; change in strength on one side is greater than the other, trouble speaking or thinking, change in balance; or fever
- Hearing loss
- Confusion
- Change in balance
- Fast heartbeat
- Abnormal heartbeat
- Passing out
- Vision changes
- Color blindness
- Blindness
- Pinpoint red spots on skin
- Abdominal pain
- Sore throat
- Anxiety
- Chills
- Muscle pain
- Muscle weakness
- Sweating a lot
- Seizures
- Tremors
- Restlessness
- Thoughts of suicide
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.