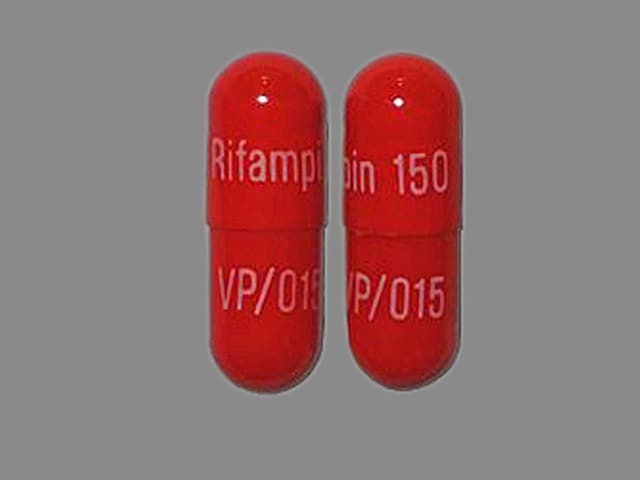
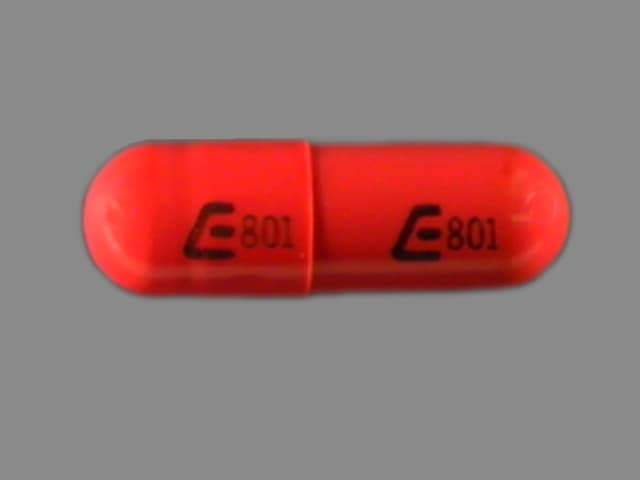
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Rifadin: 150 mg, 300 mg [contains brilliant blue fcf (fd&c blue #1), corn starch, fd&c red #40]
Generic: 150 mg, 300 mg
Solution Reconstituted, Intravenous:
Rifadin: 600 mg (1 ea)
Solution Reconstituted, Intravenous [preservative free]:
Rifadin: 600 mg (1 ea) [contains sodium formaldehyde sulfoxylate]
Generic: 600 mg (1 ea)
Pharmacology
Mechanism of Action
Inhibits bacterial RNA synthesis by binding to the beta subunit of DNA-dependent RNA polymerase, blocking RNA transcription
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Well absorbed; food may delay or slightly reduce peak
Distribution
Crosses the blood-brain barrier well
Relative diffusion of antimicrobial agents from blood into cerebrospinal fluid (CSF): Adequate with or without inflammation (exceeds usual MICs)
Ratio of CSF to blood level (%): Inflamed meninges: 25
Metabolism
Hepatic; undergoes enterohepatic recirculation
Excretion
Feces (60% to 65%) and urine (~30%) as unchanged drug
Time to Peak
Serum: Oral: 2 to 4 hours
Duration of Action
≤24 hours
Half-Life Elimination
3 to 4 hours, prolonged with hepatic impairment; End-stage renal disease: 1.8 to 11 hours
Protein Binding
80%
Use in Specific Populations
Special Populations: Children
After oral administration, the Cmax ranged from 3.5 to 15 mcg/mL, Tmax was 1 hour, and half-life was approximately 2.9 hours. After IV administration, the Cmax after the initial infusion was approximately 25.9 mcg/mL and half-life ranged from 1.04 to 3.81 hours.
Use: Labeled Indications
Meningococcal prophylaxis: Treatment of asymptomatic carriers of Neisseria meningitidis to eliminate meningococci from the nasopharynx
Tuberculosis: Treatment of tuberculosis in combination with other agents
Use: Off Label
Anaplasmosisyes
Based on the IDSA guidelines for the clinical assessment, treatment, and prevention of Lyme disease, human granulocytic anaplasmosis (HGA) and babesiosis and the Centers for Disease Control and Prevention (CDC) guideline for the diagnosis and management of tickborne rickettsial diseases: Rocky Mountain spotted fever and other spotted fever group rickettsioses, ehrlichioses, and anaplasmosis, rifampin may be considered as an alternative therapy to doxycycline for the treatment of mild cases of human anaplasmosis (also known as human granulocytic anaplasmosis [HGA]) in patients who are pregnant or who have a severe drug allergy to doxycycline. Due to similar symptoms, Rocky Mountain spotted fever (RMSF) should be ruled out before considering rifampin treatment for human anaplasmosis; rifampin is not an acceptable treatment of RMSF. In addition, rifampin does not treat coinfection with Lyme disease (B. burgdorferi).
Brain abscess, empyema, and epidural abscess (MRSA)cyes
According to Infectious Diseases Society of America (IDSA) guidelines regarding the treatment of methicillin-resistant Staphylococcus aureus (MRSA) infections, rifampin can be considered as adjunctive therapy to vancomycin in the treatment of brain abscess, empyema, or spinal epidural abscess. The use of rifampin warrants increased awareness of possible drug interactions caused by liver enzyme induction. Rifampin should only be used in combination with other antibiotics for S. aureus infections because resistance can develop rapidly with monotherapy.
Brucellosisbyes
Data from randomized studies support the use of rifampin, in combination with doxycycline, as an alternative regimen for the treatment of brucellosis Hashemi 2012, Solera 1995. Additional trials may be necessary to further define the role of rifampin in this condition.
Based on the World Health Organization (WHO) guidelines for brucellosis, rifampin, in combination with doxycycline, is an effective and recommended alternative agent in the management of uncomplicated brucellosis.
Cholestatic pruritusayes
Data from a meta-analysis of randomized controlled trials support the use of rifampin in the treatment of cholestatic pruritus.
American Association for the Study of Liver Diseases practice guidelines for primary biliary cirrhosis recommend the use of rifampin for cholestatic pruritus refractory to bile acid sequestrants.
Device-related osteoarticular infection (MRSA)cyes
According to IDSA guidelines, rifampin is recommended as part of the treatment regimen for MRSA in device-related osteoarticular infection. Initial therapy should include a parenteral therapy regimen for osteomyelitis followed by rifampin and another antibiotic (a fluoroquinolone, sulfamethoxazole/trimethoprim, a tetracycline, or clindamycin). At this time, treatment of device-related osteoarticular infection with rifampin alone or without initial parenteral antibiotic therapy is not recommended.
Endocarditis (prosthetic valve), treatmentyes
Based on the American Heart Association (AHA) Scientific Statement for Infective Endocarditis in Adults, rifampin (in combination with other antibiotics) is an effective and recommended treatment regimen for infective endocarditis due to staphylococci (methicillin-susceptible or methicillin-resistant) involving a prosthetic valve.
Haemophilus influenzae type B, chemoprophylaxisyes
Based on the Advisory Committee on Immunization Practices (ACIP) recommendations for prevention and control of H. influenzae type b disease, rifampin is effective and recommended as chemoprophylaxis in index patients with invasive Hib disease (unless treated with cefotaxime or ceftriaxone); all household contacts in households with members aged <4 years who are not fully vaccinated or members aged <18 years who are immunocompromised, regardless of their vaccination status; and child care settings when two or more cases of invasive Hib disease occurred within 60 days and unimmunized or underimmunized children attend the facility.
Leprosyyes
Based on the National Hansen’s Disease Program (NHDP) treatment recommendations and World Health Organization (WHO) Expert Committee on Leprosy, rifampin, in combination with other agents, is an effective and recommended treatment for lepromatous (multibacillary) and tuberculoid (paucibacillary) leprosy.
Meningitis, bacterial (adjunct therapy)yes
Based on the IDSA guidelines for management of bacterial meningitis and health care-associated ventriculitis and meningitis, rifampin is an effective and recommended adjunctive agent in the treatment of bacterial meningitis caused by S. pneumoniae (when used in combination with a third-generation cephalosporin and vancomycin if MIC to ceftriaxone is >2 mcg/mL) and in patients with ventriculitis or meningitis caused by susceptible staphylococci (in combination with an antistaphylococcal agent) who have intracranial or spinal hardware (eg, CSF shunt or drain), especially in cases where the hardware cannot be removed.
Nasal decolonization of S. aureusyes
Based on the IDSA guidelines for the Treatment of Methicillin-Resistant S. aureus Infections, rifampin, in combination with another antistaphylococcal antibiotic (eg, trimethoprim and sulfamethoxazole, doxycycline), is an effective and recommended alternative option for nasal decolonization of S. aureus in patients who continue to experience infections in spite of other decolonization measures.
Nontuberculous mycobacterial disease, pulmonaryyes
Based on the American Thoracic Society (ATS) and Infectious Diseases Society of America (IDSA) Guideline for the Diagnosis, Treatment, and Prevention of Nontuberculosis Mycobacterial Disease, rifampin (in combination with other antimicrobials) is effective and recommended for the treatment of Mycobacterium avium complex (MAC) and Mycobacterium kansasii pulmonary disease.
Osteomyelitis (MRSA)cyes
IDSA, SIMIT, and BSAC guidelines recommend the use of rifampin as a therapeutic option for MRSA and MSSA osteomyelitis. Evidence for the use of rifampin is based largely on clinical experience and observational studies. The use of rifampin warrants increased awareness of possible drug interactions caused by liver enzyme induction. Rifampin should only be used in combination with other antibiotics for S. aureus infections because resistance can develop rapidly with monotherapy.
Prosthetic joint infectionyes
Based on the Infectious Diseases Society of America (IDSA) guidelines for the management of prosthetic joint infection, rifampin is an effective and recommended adjunctive agent for the treatment of prosthetic joint infection with Staphylococci (oxacillin-susceptible or -resistant) infection.
Septic thrombosis of cavernous or dural venous sinus (MRSA)cyes
According to IDSA guidelines regarding the treatment of MRSA infections, rifampin can be considered as add-on therapy to vancomycin in septic thrombosis of cavernous or dural venous sinus. The use of rifampin warrants increased awareness of possible drug interactions caused by liver enzyme induction. Rifampin should only be used in combination with other antibiotics for S. aureus infections because resistance can develop rapidly with monotherapy.
Streptococcus (group A) chronic carriageyes
Based on the IDSA Clinical Practice Guideline for the Diagnosis and Management of Group A Streptococcal Pharyngitis, rifampin (in combination with oral penicillin V or intramuscular benzathine penicillin G) is an effective and recommended treatment option in chronic carriers of group A Streptococcus.
Contraindications
Hypersensitivity to rifampin, any rifamycins, or any component of the formulation; concurrent use of atazanavir, darunavir, fosamprenavir, praziquantel, ritonavir/saquinavir, saquinavir, or tipranavir.
Canadian labeling: Additional contraindications (not in US labeling): Jaundice associated with reduced bilirubin excretion; premature and newborn infants; breastfeeding women; hepatic function impairment.
Dosage and Administration
Dosing: Adult
Meningococcal prophylaxis: Oral, IV: 600 mg twice daily for 2 days
Tuberculosis, active (drug-susceptible): Oral, IV: Note: Always administer in combination with other antitubercular drugs (Nahid 2016).
Dosing:
Manufacturer's labeling: 10 mg/kg/day once daily (maximum: 600 mg/day)
Alternate recommendations: ATS/CDC/IDSA Drug-susceptible tuberculosis guideline recommendations (Nahid 2016):
Once-daily therapy: 10 mg/kg/day once daily (usual dose: 600 mg). Note: The preferred frequency of administration is once daily during the intensive and continuation phases; however, 5-days-per-week administration by directly observed therapy (DOT) is an acceptable alternative.
Twice-weekly or three-times-weekly DOT: 10 mg/kg/dose (usual dose: 600 mg) administered 2 or 3 times weekly (Nahid 2016)
Regimens: Treatment regimens for pulmonary tuberculosis and tuberculous meningitis consist of an initial 2-month phase of a 4-drug regimen, followed by a continuation phase of an additional 4 to 7 months of rifampin and isoniazid for pulmonary tuberculosis and a continuation phase of an additional 7 to 10 months of rifampin and isoniazid for tuberculous meningitis (optimal duration is not defined although continuation phase must continue for a minimum of 7 additional months). If community rates of isoniazid resistance are <4%, an initial treatment regimen with less than 4 drugs may be considered. Readdress need for fourth drug when susceptibility results are available. Adjunctive corticosteroid therapy (eg, dexamethasone, prednisolone) tapered over 6 to 8 weeks is also recommended for tuberculous meningitis. Rifampin frequency and dosing differs depending on treatment regimen selected; consult current Drug-sensitive TB guidelines (Nahid 2016).
Tuberculosis, latent infection (LTBI): As an alternative to isoniazid: Oral, IV: 10 mg/kg/day (maximum: 600 mg/day) for 4 months. Note: Combination with pyrazinamide should not generally be offered (MMWR Aug 8, 2003).
Anaplasmosis, mild cases (patients with severe allergy to doxycycline) (off-label use): Oral: 300 mg twice daily for 7 to 10 days. Note: Rifampin is not an effective agent for Rocky Mountain spotted fever (RMSF); ensure that RMSF has been ruled out prior to use. Rifampin is also not effective for Lyme disease; if co-infection with B. burgdorferi is suspected, treat with an additional appropriate antimicrobial agent (CDC [Biggs 2016]; IDSA [Wormser 2006]).
Brain abscess, empyema, and epidural abscess (MRSA) (off-label use): Oral, IV: 600 mg once daily or 300 to 450 mg twice daily with concomitant vancomycin for 4 to 6 weeks (IDSA [Liu 2011])
Brucellosis (off-label use): Oral: 600 to 900 mg once daily for 6 weeks; use in combination with doxycycline (WHO 2006). Additional data may be necessary to further define the role of rifampin in this condition.
Cholestatic pruritus (off-label use) (Lindor 2009): Oral: Dose based on bilirubin value:
Bilirubin <3 mg/dL: 150 mg daily
Bilirubin ≥3 mg/dL: 150 mg twice daily
Device-related osteoarticular infection (MRSA) (off-label use): Oral: 600 mg once daily or 300 to 450 mg twice daily in combination with another antistaphylococcal antibiotic (IDSA [Liu 2011])
Endocarditis, treatment (prosthetic valve) (off-label use): Oral, IV:
MRSA: 300 mg every 8 hours for at least 6 weeks (combine with vancomycin for the entire duration of therapy and gentamicin for the first 2 weeks) (IDSA [Liu 2011]; AHA [Baddour 2015])
MSSA: 300 mg every 8 hours for at least 6 weeks (combine with nafcillin or oxacillin for the entire duration of therapy and gentamicin for the first 2 weeks) (AHA [Baddour 2015])
H. influenzae type B, chemoprophylaxis (off-label use): Oral: 600 mg once daily for 4 days (Red Book [AAP] 2015)
Leprosy (off-label use): Oral:
Lepromatous (multibacillary):
National Hansen Disease Program: 600 mg once daily for 24 months in combination with clofazimine and dapsone (NHDP [HRSA 2016])
World Health Organization: 600 mg once monthly for 12 months in combination with clofazimine and dapsone (WHO 2012)
Tuberculoid (paucibacillary):
National Hansen Disease Program: 600 mg once daily for 12 months in combination with dapsone (NHDP [HRSA 2016])
World Health Organization: 600 mg once monthly for 6 months in combination with dapsone (WHO 2012)
Meningitis, bacterial (adjunct therapy) (off-label use): Pathogen-specific therapy (eg, staphylococci [in patients with prosthetic material], S. pneumoniae [when MIC to ceftriaxone is >2 mcg/mL]): Oral, IV: 600 mg once daily; use in combination with other antimicrobials (IDSA [Tunkel 2004]; IDSA [Tunkel 2017])
Nasal decolonization of Staphylococcus aureus (off-label use): Oral, IV: 600 mg/day for 5 to 10 days; Note: Must use in combination with at least one other systemic antistaphylococcal antibiotic. Not recommended as first-line drug for decolonization; evidence is weak for use in patients with recurrent infections (IDSA [Liu 2011]).
Nontuberculous mycobacterial disease, pulmonary (off-label use): Oral, IV:
M. avium complex (nodular/bronchiectatic disease) (ATS/IDSA [Griffith 2007]): 600 mg 3 times weekly in combination with a 3-times-weekly regimen of a macrolide (azithromycin or clarithromycin) and ethambutol; continue treatment until patient is culture negative on therapy for 1 year.
M. avium complex (severe nodular/bronchiectatic or cavitary disease) (ATS/IDSA [Griffith 2007]): 600 mg (450 mg in patients weighing <50 kg) once daily in combination with daily macrolide (azithromycin or clarithromycin) and ethambutol therapy; continue treatment until patient is culture negative on therapy for 1 year. May also consider addition of 3 times weekly amikacin or streptomycin early in therapy.
M. avium complex (cystic fibrosis patients) (Floto 2016):
<50 kg: 450 mg once daily in combination with daily macrolide (azithromycin [preferred] or clarithromycin) and ethambutol therapy
>50 kg: 600 mg once daily in combination with daily macrolide (azithromycin [preferred] or clarithromycin) and ethambutol therapy
M. kansasii (ATS/IDSA [Griffith 2007]): 600 mg once daily in combination with daily ethambutol and isoniazid therapy; continue treatment until patient is culture negative on therapy for 1 year.
Osteomyelitis (MRSA) (off-label use): Oral, IV: 600 mg once daily or 300 to 450 mg twice daily for at least 8 weeks with concomitant trimethoprim/sulfamethoxazole, linezolid or clindamycin (IDSA [Liu 2011])
Prosthetic joint infection (off-label use): Staphylococci (oxacillin-susceptible or oxacillin-resistant): Oral:
Debridement and prosthesis retention or following 1-stage exchange, acute treatment: 300 to 450 mg every 12 hours in combination with an IV antistaphylococcal antibiotic for 2 to 6 weeks (IDSA [Osmon 2013])
Debridement and prosthesis retention or following 1-stage exchange, chronic treatment:
Total ankle, elbow, hip, or shoulder arthroplasty: 300 to 450 mg every 12 hours in combination with an oral antistaphylococcal antibiotic for 3 months (IDSA [Osmon 2013])
Total knee arthroplasty: 300 to 450 mg every 12 hours in combination with an oral antistaphylococcal antibiotic for 6 months (IDSA [Osmon 2013])
Septic thrombosis of cavernous or dural venous sinus (MRSA) (off-label use): Oral, IV: 600 mg once daily or 300 to 450 mg twice daily with concomitant vancomycin for 4 to 6 weeks (IDSA [Liu 2011])
Streptococcus (group A) chronic carriage (off-label use): Note: Most individuals with chronic carriage do not require antibiotics (IDSA [Shulman 2012]):
When combined with oral penicillin V: Oral: 600 mg once daily for the last 4 days of treatment (Chaudhary 1985; IDSA [Shulman 2012])
When combined with single dose IM penicillin G benzathine: Oral: 300 mg twice daily for 4 days (IDSA [Shulman 2012]; Tanz 1985)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Rifampin monotherapy is rarely indicated; most indications require combination therapy with other antimicrobial agent. Recommendations often change due to epidemiology (resistance) and emerging information; consult CDC and WHO for current recommendations, as appropriate (ATS/CDC/IDSA [Nahid 2016]; WHO 2010; WHO 2014).
Active tuberculosis infection (excluding meningitis), treatment (drug susceptible): Note: Always use as part of a multidrug regimen. Any regimens using less than once daily dosing should administer dosing as directly observed therapy (DOT). Treatment regimens for pulmonary tuberculosis consist of an initial 2-month intensive phase of a 4-drug regimen, followed by a continuation phase of an additional 4 to 7 months of isoniazid and rifampin. Rifampin frequency and dosing differs depending on treatment regimen selected; consult current drug-sensitive TB guidelines for detailed information (ATS/CDC/IDSA [Nahid 2016].
ATS/CDC/IDSA Recommendations (ATS/CDC/IDSA [Nahid 2016]): Note: For HIV-exposed/-positive, refer to specific guidelines for guidance on drug interaction management with antiretroviral therapy (see Drug-Drug Interactions)
Once daily or 5-times-weekly (DOT):
Infants, Children, and Adolescents <15 years, weighing ≤40 kg: Oral, IV: 10 to 20 mg/kg/dose once daily; maximum dose: 600 mg/dose
Children and Adolescents <15 years weighing >40 kg or Adolescents ≥15 years: Oral, IV: 10 mg/kg/dose once daily (typical dose: 600 mg)
Three-times-weekly DOT: Note: Although suggested dosing based on experience with twice-weekly regimen; experts suggest three-times-weekly regimens are more effective than twice-weekly DOT regimens; three-times-weekly DOT may be used as part of an intensive phase and/or continuation phase dosing regimen; consult guidelines for specific information
Infants, Children, and Adolescents <15 years, weighing ≤40 kg: Oral, IV: 10 to 20 mg/kg/dose 3-times-weekly; maximum dose: 600 mg/dose
Children and Adolescents <15 years weighing >40 kg or Adolescents ≥15 years: Oral, IV: 10 mg/kg/dose 3-times-weekly (typical dose: 600 mg)
Twice-weekly DOT: Note: Regimen not generally recommended; do not use in HIV patients or those with smear-positive and/or cavitary disease. This therapy should only be used following completion of a 2-week intensive phase once-daily (or 5-times-weekly) regimen. Missed doses result in the equivalent of once-weekly dosing which has been shown to be inferior and is associated with treatment failure, relapse, and development of drug resistance.
Infants, Children, and Adolescents <15 years, weighing ≤40 kg: Oral, IV: 10 to 20 mg/kg/dose twice weekly; maximum dose: 600 mg/dose
Children and Adolescents <15 years weighing >40 kg or Adolescents ≥15 years: Oral, IV: 10 mg/kg/dose twice weekly (typical dose: 600 mg)
Latent tuberculosis infection (LTBI), treatment: Note: May be considered for those unable to tolerate isoniazid or if isoniazid-resistance is suspected.
Non-HIV-exposed/-positive:
Infants, Children, and Adolescents: Oral: 15 to 20 mg/kg/dose once daily; maximum dose: 600 mg/dose; use in combination with isoniazid for 3 to 4 months or as monotherapy for 4 months (CDC 2018; Diallo 2018; Red Book [AAP 2018]; WHO 2018). Note: Lower doses of 10 mg/kg/day have been described; however, pharmacokinetic studies suggest that lower doses of rifampin do not provide adequate drug exposure (Kwara 2016). In addition, one clinical trial comparing 4 months of rifampin monotherapy to 9 months of isoniazid monotherapy in pediatric patients (n=422 in the rifampin group; age range: 0 to 17 years; rifampin dose: 15 to 20 mg/kg/dose) showed similar rates of efficacy and better treatment adherence (Diallo 2018).
HIV-exposed/-positive: Note: Not appropriate for all HIV patients due to drug-drug interactions with some antiretrovirals; refer to specific guidelines for guidance on drug interaction management with antiretroviral therapy (see Drug-Drug Interactions)
Infants and Children: Oral: 10 to 20 mg/kg/dose once daily; maximum dose: 600 mg/dose; use in combination with isoniazid for 3 to 4 months or as monotherapy for 4 to 6 months (HHS [OI pediatric 2018]); continue therapy for 6 months if exposure to an isoniazid mono-resistant source case (HHS [OI pediatric 2018]; WHO 2018). Note: Pharmacokinetic studies suggest that lower doses of rifampin do not provide adequate drug exposure (Kwara 2016).
Adolescents: Oral: 600 mg once daily for 4 months (HHS [OI adult 2018])
Catheter (peritoneal dialysis); exit-site or tunnel infection: Infants, Children, and Adolescents: Oral: 10 to 20 mg/kg/day divided into 2 doses. Maximum dose: 600 mg/dose (ISPD [Warady 2012]). Note: Should not be used as monotherapy or routinely used in areas where TB is endemic.
Endocarditis:
Empiric therapy, prosthetic valve/material (AHA [Baltimore 2015]): Note: Use in combination with other antibiotics:
Early infection (≤1 year postop)/nosocomial infection associated with cannulation: Children and Adolescents: Oral, IV: 20 mg/kg/day divided every 8 hours; maximum daily dose: 900 mg/day
Late infection (>1 year postop): Children and Adolescents: Oral, IV: 15 to 20 mg/kg/day divided every 12 hours; maximum daily dose: 600 mg/day
MRSA infection, prosthetic valve: Infants, Children, and Adolescents: Oral, IV: 15 mg/kg/day divided every 8 hours; maximum daily dose: 900 mg/day (IDSA [Liu 2011])
H. influenzae prophylaxis: Infants, Children, and Adolescents: Oral: 20 mg/kg/day once daily for 4 days, not to exceed 600 mg/dose (Kliegman 2016; Red Book [AAP 2018])
Meningococcal prophylaxis: Infants, Children, and Adolescents: Oral: 20 mg/kg/day in divided doses every 12 hours for 2 days, not to exceed 600 mg/dose
Peritonitis (peritoneal dialysis), treatment: Infants, Children, and Adolescents: Oral: 10 to 20 mg/kg/day divided into 2 doses; maximum dose: 600 mg/dose (ISPD [Warady 2012])
Pharyngeal chronic carriers of group A streptococci, treatment: Children and Adolescents: Oral: 20 mg/kg/day once daily for the last 4 days of treatment when combined with oral penicillin V or 20 mg/kg/day in 2 divided doses for 4 days when combined with intramuscular benzathine penicillin G; maximum daily dose: 600 mg/day (IDSA [Shulman 2012])
Staphylococcus aureus, nasal carriers: Children and Adolescents: Oral, IV: 15 mg/kg/day divided every 12 hours for 5 to 10 days; Note: Must use in combination with at least one other systemic antistaphylococcal antibiotic. Maximum daily dose: 600 mg/day. Not recommended as first-line drug for decolonization; evidence is weak for use in patients with recurrent infections (IDSA [Liu 2011]).
Reconstitution
Reconstitute vial with 10 mL SWFI. Prior to injection, dilute in appropriate volume of a compatible solution (eg, 100 mL D5W).
Extemporaneously Prepared
25 mg/mL Oral Suspension (ASHP Standard Concentration) (ASHP 2017)
A 25 mg/mL oral suspension may be made with capsules and one of three different vehicles (a 1:1 mixture of Ora-Sweet and Ora-Plus, a 1:1 mixture of Ora-Sweet SF and Ora-Plus, or cherry syrup concentrate diluted 1:4 with simple syrup, NF). Empty the contents of ten 300 mg capsules into a mortar and reduce to a fine powder. Add 20 mL of the vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 120 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 120 mL. Label "shake well," “protect from light” and " refrigerate." Stable for 28 days refrigerated (preferred) or at room temperature (Allen 1998; Nahata 2014).
Allen LV Jr, Erickson MA. Stability of bethanechol chloride, pyrazinamide, quinidine sulfate, rifampin, and tetracycline hydrochloride in extemporaneously compounded oral liquids. Am J Health Syst Pharm. 1998;55(17):1804-1809.9775343Nahata MC and Pai VB. Pediatric Drug Formulations. 6th ed. Cincinnati, OH: Harvey Whitney Books Co; 2014.
10 mg/mL Oral Suspension
A 10 mg/mL oral suspension may be made with capsules and simple syrup, NF. Empty the contents of four 300 mg capsules into a mortar. If necessary, crush contents to produce a fine powder. Add 20 mL of simple syrup, NF and mix to a uniform paste; mix while adding simple syrup in incremental proportions to almost 120 mL; transfer to a calibrated bottle, rinse mortar with simple syrup, and add quantity of vehicle sufficient to make 120 mL. Label "shake well." Stable for 42 days at room temperature (Nahata 2014).
Nahata MC and Pai VB. Pediatric Drug Formulations. 6th ed. Cincinnati, OH: Harvey Whitney Books Co; 2014.
Administration
IV: Administer IV preparation by slow IV infusion over 30 minutes to 3 hours at a final concentration not to exceed 6 mg/mL. Do not administer IM or SubQ. Avoid extravasation.
Oral: Administer on an empty stomach (ie, 1 hour prior to, or 2 hours after meals or antacids) to increase total absorption. The compounded oral suspension must be shaken well before using. May mix contents of capsule with applesauce or jelly.
Storage
Capsule: Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F); avoid excessive heat.
Injection: Store intact vials at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F); avoid excessive heat (>40°C [104°F]). Protect the intact vials from light. Reconstituted vials are stable for 30 hours at room temperature. Stability of parenteral admixture at room temperature (25°C [77°F]) is 8 hours for D5W or 6 hours for NS. Note: As of July 2018, the storage of reconstituted vials was changed from 24 hours to 30 hours at room temperature, the stability when admixed in D5W was changed from 4 hours to 8 hours, and the stability when admixed in NS from 24 hours to 6 hours in the Rifadin prescribing information. Similar changes may not be reflected in the Rifadin prescribing information for product distributed prior to July 2018 or in generic manufacturer's labeling.
Rifampin Images
Drug Interactions
Abemaciclib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Abemaciclib. Avoid combination
Abiraterone Acetate: CYP3A4 Inducers (Strong) may decrease the serum concentration of Abiraterone Acetate. Management: Avoid whenever possible. If such a combination cannot be avoided, increase abiraterone acetate dosing frequency from once daily to twice daily during concomitant use. Consider therapy modification
Acalabrutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Acalabrutinib. Management: Avoid co-administration of strong CYP3A inducers in patients taking acalabrutinib. If strong CYP3A inducers cannot be avoided, increase the dose of acalabrutinib to 200 mg twice daily. Consider therapy modification
Afatinib: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Afatinib. Management: Per US labeling: if requiring chronic use of P-gp inducers, increase afatinib dose by 10 mg as tolerated; reduce to original afatinib dose 2-3 days after stopping P-gp inducers. Per Canadian labeling: avoid combination if possible. Consider therapy modification
Agomelatine: RifAMPin may decrease the serum concentration of Agomelatine. Monitor therapy
Alfentanil: Rifamycin Derivatives may decrease the serum concentration of Alfentanil. Management: Monitor closely for decreased alfentanil effectiveness. Increased alfentanil doses will likely be needed. Alternatively, changing from alfentanil to a different opioid anesthetic (e.g., sufentanil) may also be considered. Consider therapy modification
Alpelisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Alpelisib. Avoid combination
Amiodarone: RifAMPin may decrease serum concentrations of the active metabolite(s) of Amiodarone. Specifically, desethylamiodarone concentrations may decrease. RifAMPin may decrease the serum concentration of Amiodarone. Monitor therapy
Antifungal Agents (Azole Derivatives, Systemic): May increase the serum concentration of Rifamycin Derivatives. Only rifabutin appears to be affected. Rifamycin Derivatives may decrease the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). Management: Avoid these combinations when possible. Voriconazole and isavuconazonium are considered contraindicated. Consider therapy modification
Antihepaciviral Combination Products: CYP3A4 Inducers (Strong) may decrease the serum concentration of Antihepaciviral Combination Products. Avoid combination
Apalutamide: CYP3A4 Inducers (Strong) may decrease the serum concentration of Apalutamide. Monitor therapy
Apixaban: Inducers of CYP3A4 (Strong) and P-glycoprotein may decrease the serum concentration of Apixaban. Avoid combination
Apremilast: CYP3A4 Inducers (Strong) may decrease the serum concentration of Apremilast. Avoid combination
Aprepitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Aprepitant. Avoid combination
ARIPiprazole: CYP3A4 Inducers (Strong) may decrease the serum concentration of ARIPiprazole. Management: Double the oral aripiprazole dose and closely monitor. Reduce oral aripiprazole dose to 10-15 mg/day (for adults) if the inducer is discontinued. Avoid use of strong CYP3A4 inducers for more than 14 days with extended-release injectable aripiprazole. Consider therapy modification
ARIPiprazole Lauroxil: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of ARIPiprazole Lauroxil. Management: Patients taking the 441 mg dose of aripiprazole lauroxil increase their dose to 662 mg if used with a strong CYP3A4 inducer for more than 14 days. No dose adjustment is necessary for patients using the higher doses of aripiprazole lauroxil. Consider therapy modification
Artemether: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Artemether. Specifically, dihydroartemisinin concentrations may be reduced. CYP3A4 Inducers (Strong) may decrease the serum concentration of Artemether. Avoid combination
Asunaprevir: RifAMPin may decrease the serum concentration of Asunaprevir. This effect is most likely with longer-term coadministration; single-dose rifampin may increase asunaprevir concentrations. RifAMPin may increase the serum concentration of Asunaprevir. This effect is likely following only single-dose or short-term rifampin administration. Longer-term coadministration is likely to result in decreased asunaprevir concentrations. Avoid combination
Ataluren: RifAMPin may decrease the serum concentration of Ataluren. Monitor therapy
Atazanavir: RifAMPin may decrease the serum concentration of Atazanavir. Avoid combination
Atovaquone: Rifamycin Derivatives may decrease the serum concentration of Atovaquone. Avoid combination
Avapritinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Avapritinib. Avoid combination
Avatrombopag: RifAMPin may decrease the serum concentration of Avatrombopag. Management: Management of this interaction varies based on avatrombopag indication. Dose adjustments are required for patients using avatrombopag for chronic immune thrombocytopenia. See monograph for details. Consider therapy modification
Axitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Axitinib. Avoid combination
Barbiturates: Rifamycin Derivatives may increase the metabolism of Barbiturates. Monitor therapy
Bazedoxifene: RifAMPin may decrease the serum concentration of Bazedoxifene. This may lead to loss of efficacy or, if bazedoxifene is combined with estrogen therapy, an increased risk of endometrial hyperplasia. Monitor therapy
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Bedaquiline: CYP3A4 Inducers (Strong) may decrease the serum concentration of Bedaquiline. Avoid combination
Benperidol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Benperidol. Monitor therapy
Benzhydrocodone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Benzhydrocodone. Specifically, the serum concentrations of hydrocodone may be reduced. Monitor therapy
Beta-Blockers: Rifamycin Derivatives may decrease the serum concentration of Beta-Blockers. Exceptions: Atenolol; Carteolol (Ophthalmic); Levobunolol; Metipranolol; Nadolol. Monitor therapy
Betrixaban: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Betrixaban. Avoid combination
Bictegravir: RifAMPin may decrease the serum concentration of Bictegravir. Avoid combination
Bortezomib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Bortezomib. Avoid combination
Bosentan: RifAMPin may decrease the serum concentration of Bosentan. Following the initial several weeks of concurrent rifampin, this effect is most likely. RifAMPin may increase the serum concentration of Bosentan. This effect is most likely to be observed within the initial few weeks of concurrent therapy (and may be greatest immediately following initiation of the combination). Management: Weekly monitoring of liver function tests during the first 4 weeks of concurrent therapy is recommended, with a return to normal recommended monitoring thereafter as appropriate. Monitor therapy
Bosutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Bosutinib. Avoid combination
Brentuximab Vedotin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be decreased. Monitor therapy
Brentuximab Vedotin: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be decreased. Monitor therapy
Brexpiprazole: CYP3A4 Inducers (Strong) may decrease the serum concentration of Brexpiprazole. Management: If brexpiprazole is used together with a strong CYP3A4 inducer, the brexpiprazole dose should gradually be doubled over the course of 1 to 2 weeks. Consider therapy modification
Brigatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Brigatinib. Avoid combination
Brivaracetam: RifAMPin may decrease the serum concentration of Brivaracetam. Management: Increase the brivaracetam dose by up to 100% (ie, double the dose) if used together with rifampin. Consider therapy modification
Buprenorphine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Buprenorphine. Monitor therapy
BusPIRone: CYP3A4 Inducers (Strong) may decrease the serum concentration of BusPIRone. Management: Consider alternatives to this combination. If coadministration of these agents is deemed necessary, monitor patients for reduced buspirone effects and increase buspirone doses as needed. Consider therapy modification
Cabozantinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cabozantinib. Management: Avoid use of strong CYP3A4 inducers with cabozantinib if possible. If combined, cabozantinib dose adjustments are recommended and vary based on the cabozantinib product used and the indication for use. See monograph for details. Consider therapy modification
Calcifediol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Calcifediol. Monitor therapy
Calcium Channel Blockers: Rifamycin Derivatives may decrease the serum concentration of Calcium Channel Blockers. This primarily affects oral forms of calcium channel blockers. Management: The labeling for some US and Canadian calcium channel blockers contraindicate use with rifampin, however recommendations vary. Consult appropriate labeling. Exceptions: Clevidipine. Consider therapy modification
Canagliflozin: RifAMPin may decrease the serum concentration of Canagliflozin. Management: Consider increasing canagliflozin dose to 200 mg/day in patients tolerating 100 mg/day. A further increase to 300 mg/day can be considered in patients with an estimated glomerular filtration rate (GFR) of 60 mL/min/1.73 m2 or greater. Consider therapy modification
Cannabidiol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cannabidiol. Monitor therapy
Cannabidiol: CYP2C19 Inducers (Strong) may decrease the serum concentration of Cannabidiol. Monitor therapy
Cannabis: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cannabis. More specifically, tetrahydrocannabinol and cannabidiol serum concentrations may be decreased. Monitor therapy
CarBAMazepine: CYP3A4 Inducers (Strong) may decrease the serum concentration of CarBAMazepine. Monitor therapy
Cariprazine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cariprazine. Avoid combination
Caspofungin: RifAMPin may decrease the serum concentration of Caspofungin. Management: Caspofungin prescribing information recommends using a dose of 70 mg daily in adults (or 70 mg/m2, up to a maximum of 70 mg, daily in pediatric patients) who are also receiving rifampin. Consider therapy modification
CeFAZolin: May enhance the adverse/toxic effect of RifAMPin. Specifically, the risk for bleeding may be increased. Management: Avoid concomitant use of rifampin with cefazolin when possible. If combined, closely monitor prothrombin time or other coagulation tests and administer vitamin K as needed. Consider therapy modification
Celiprolol: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Celiprolol. Monitor therapy
Cephalosporins (N-methylthiotetrazole [NMTT] Side Chain Containing): May enhance the adverse/toxic effect of RifAMPin. Specifically, the risk for bleeding may be increased. Management: Avoid concomitant use of rifampin with cephalosporins that contain an N-methylthiotetrazole (NMTT) side chain when possible. If combined, closely monitor prothrombin time or other coagulation tests and administer vitamin K as needed. Consider therapy modification
Ceritinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ceritinib. Avoid combination
Chloramphenicol (Systemic): RifAMPin may increase the metabolism of Chloramphenicol (Systemic). Consider therapy modification
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Citalopram: RifAMPin may decrease the serum concentration of Citalopram. Monitor therapy
Cladribine: BCRP/ABCG2 Inducers may decrease the serum concentration of Cladribine. Monitor therapy
Cladribine: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Cladribine. Monitor therapy
Clarithromycin: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Clarithromycin. Clarithromycin may increase the serum concentration of CYP3A4 Inducers (Strong). CYP3A4 Inducers (Strong) may decrease the serum concentration of Clarithromycin. Management: Consider alternative antimicrobial therapy for patients receiving a CYP3A inducer. Drugs that enhance the metabolism of clarithromycin into 14-hydroxyclarithromycin may alter the clinical activity of clarithromycin and may impair clarithromycin efficacy. Consider therapy modification
Clopidogrel: CYP2C19 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Clopidogrel. Monitor therapy
CloZAPine: CYP3A4 Inducers (Strong) may decrease the serum concentration of CloZAPine. Avoid combination
Cobicistat: RifAMPin may decrease the serum concentration of Cobicistat. Avoid combination
Cobimetinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cobimetinib. Avoid combination
Codeine: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Codeine. Monitor therapy
Copanlisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Copanlisib. Avoid combination
Corticosteroids (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Corticosteroids (Systemic). Exceptions: Hydrocortisone (Systemic); PrednisoLONE (Systemic); PredniSONE. Monitor therapy
Crizotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Crizotinib. Avoid combination
CycloSPORINE (Systemic): Rifamycin Derivatives may increase the metabolism of CycloSPORINE (Systemic). Consider therapy modification
CYP2B6 Substrates (High risk with Inducers): CYP2B6 Inducers (Moderate) may decrease the serum concentration of CYP2B6 Substrates (High risk with Inducers). Monitor therapy
CYP2C19 Substrates (High risk with Inducers): CYP2C19 Inducers (Strong) may increase the metabolism of CYP2C19 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP2C9 Substrates (High risk with Inducers): CYP2C9 Inducers (Moderate) may decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Substrates (High risk with Inducers): CYP3A4 Inducers (Strong) may increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Exceptions: Benzhydrocodone; Buprenorphine; CarBAMazepine; Etizolam; HYDROcodone; Mirtazapine; TraMADol; Zolpidem. Consider therapy modification
Dabigatran Etexilate: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Dabigatran Etexilate. Management: Avoid concurrent use of dabigatran with P-glycoprotein inducers whenever possible. Avoid combination
Dabrafenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dabrafenib. Monitor therapy
Daclatasvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Daclatasvir. Avoid combination
Darolutamide: Inducers of CYP3A4 (Strong) and P-glycoprotein may decrease the serum concentration of Darolutamide. Avoid combination
Darunavir: RifAMPin may decrease the serum concentration of Darunavir. Avoid combination
Dasabuvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dasabuvir. Avoid combination
Dasatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dasatinib. Management: Avoid when possible. If such a combination cannot be avoided, consider increasing dasatinib dose and monitor clinical response and toxicity closely. Consider therapy modification
Deferasirox: RifAMPin may decrease the serum concentration of Deferasirox. Management: Avoid combination when possible; if the combination must be used, consider a 50% increase in initial deferasirox dose, with monitoring of serum ferritin concentrations and clinical responses to guide further dosing. Consider therapy modification
Deflazacort: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Deflazacort. Avoid combination
Delamanid: CYP3A4 Inducers (Strong) may decrease the serum concentration of Delamanid. Avoid combination
Delavirdine: Rifamycin Derivatives may increase the metabolism of Delavirdine. Delavirdine may increase the serum concentration of Rifamycin Derivatives. Specifically, Rifabutin serum concentration may be increased. Avoid combination
DexAMETHasone (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of DexAMETHasone (Systemic). Management: Consider dexamethasone dose increases in patients receiving strong CYP3A4 inducers and monitor closely for reduced dexamethasone efficacy. Consider avoiding this combination when treating life threatening conditions (ie, multiple myeloma). Consider therapy modification
Diclofenac (Systemic): CYP2C9 Inducers (Moderate) may decrease the serum concentration of Diclofenac (Systemic). Monitor therapy
Dienogest: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dienogest. Management: Avoid use of dienogest for contraception when using medications that induce CYP3A4 and for at least 28 days after discontinuation of a CYP3A4 inducer. An alternative form of contraception should be used during this time. Avoid combination
Diethylstilbestrol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Diethylstilbestrol. Monitor therapy
DilTIAZem: RifAMPin may decrease the serum concentration of DilTIAZem. Avoid combination
Disopyramide: RifAMPin may decrease the serum concentration of Disopyramide. Monitor therapy
Dolutegravir: RifAMPin may decrease the serum concentration of Dolutegravir. Management: Increase dolutegravir dose to 50 mg twice daily in adults or children. Consider alternatives to rifampin for INSTI experienced patients with clinically suspected INSTI resistance or certain INSTI associated resistance substitutions. Consider therapy modification
Doravirine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Doravirine. Avoid combination
Doxercalciferol: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Doxercalciferol. Monitor therapy
DOXOrubicin (Conventional): CYP3A4 Inducers (Strong) may decrease the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to strong CYP3A4 inducers in patients treated with doxorubicin. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
DOXOrubicin (Conventional): P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to P-glycoprotein inducers in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Doxycycline: RifAMPin may decrease the serum concentration of Doxycycline. Monitor therapy
Dronabinol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dronabinol. Monitor therapy
Dronedarone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dronedarone. Avoid combination
Duvelisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Duvelisib. Avoid combination
Edoxaban: RifAMPin may decrease the serum concentration of Edoxaban. Avoid combination
Efavirenz: RifAMPin may decrease the serum concentration of Efavirenz. Monitor therapy
Elagolix: RifAMPin may increase the serum concentration of Elagolix. Management: Use of the elagolix 200 mg twice daily dose with rifampin is not recommended. Limit combined use of the elagolix 150 mg once daily dose with rifampin to a maximum of 6 months. Consider therapy modification
Elbasvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Elbasvir. Avoid combination
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Avoid combination
Eliglustat: CYP3A4 Inducers (Strong) may decrease the serum concentration of Eliglustat. Avoid combination
Eltrombopag: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Eluxadoline: RifAMPin may increase the serum concentration of Eluxadoline. Management: Decrease the eluxadoline dose to 75 mg twice daily if combined with rifampin and monitor patients for increased eluxadoline effects/toxicities. Consider therapy modification
Elvitegravir: RifAMPin may decrease the serum concentration of Elvitegravir. Avoid combination
Encorafenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Encorafenib. Avoid combination
Enfortumab Vedotin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Enfortumab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be decreased. Monitor therapy
Entrectinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Entrectinib. Avoid combination
Enzalutamide: CYP3A4 Inducers (Strong) may decrease the serum concentration of Enzalutamide. Management: Consider using an alternative agent that has no or minimal CYP3A4 induction potential when possible. If this combination cannot be avoided, increase the dose of enzalutamide from 160 mg daily to 240 mg daily. Consider therapy modification
Eravacycline: CYP3A4 Inducers (Strong) may decrease the serum concentration of Eravacycline. Management: Increase the eravacycline dose to 1.5 mg/kg every 12 hours when combined with strong CYP3A4 inducers. Consider therapy modification
Erdafitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Erdafitinib. Avoid combination
Erlotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Erlotinib. Management: Avoid combination if possible. If combination must be used, increase erlotinib dose by 50 mg increments every 2 weeks as tolerated, to a maximum of 450 mg/day. Consider therapy modification
Esomeprazole: RifAMPin may decrease the serum concentration of Esomeprazole. Avoid combination
Estriol (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Estriol (Systemic). Monitor therapy
Estriol (Topical): CYP3A4 Inducers (Strong) may decrease the serum concentration of Estriol (Topical). Monitor therapy
Estrogen Derivatives (Contraceptive): Rifamycin Derivatives may decrease the serum concentration of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of an alternative, nonhormonal contraceptive is recommended. Consider therapy modification
Etoposide: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etoposide. Management: When possible, seek alternatives to strong CYP3A4-inducing medications in patients receiving etoposide. If combined, monitor patients closely for diminished etoposide response and need for etoposide dose increases. Consider therapy modification
Etoposide Phosphate: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etoposide Phosphate. Management: When possible, seek alternatives to strong CYP3A4-inducing medications in patients receiving etoposide phosphate. If these combinations cannot be avoided, monitor patients closely for diminished etoposide phosphate response. Consider therapy modification
Etravirine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etravirine. Avoid combination
Everolimus: CYP3A4 Inducers (Strong) may decrease the serum concentration of Everolimus. Management: Avoid concurrent use of strong CYP3A4 inducers if possible. If coadministration cannot be avoided, double the daily dose of everolimus using increments of 5 mg or less. Monitor everolimus serum concentrations closely when indicated. Consider therapy modification
Evogliptin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Evogliptin. Monitor therapy
Exemestane: CYP3A4 Inducers (Strong) may decrease the serum concentration of Exemestane. Management: Exemestane U.S. product labeling recommends using an increased dose (50 mg/day) in patients receiving concurrent strong CYP3A4 inducers. The Canadian product labeling does not recommend a dose adjustment with concurrent use of strong CYP3A4 inducers. Consider therapy modification
Fedratinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Fedratinib. Avoid combination
FentaNYL: CYP3A4 Inducers (Strong) may decrease the serum concentration of FentaNYL. Monitor therapy
Fexofenadine: RifAMPin may decrease the serum concentration of Fexofenadine. RifAMPin may increase the serum concentration of Fexofenadine. Monitor therapy
Fimasartan: RifAMPin may increase the serum concentration of Fimasartan. Avoid combination
Flibanserin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Flibanserin. Avoid combination
Fosamprenavir: RifAMPin may decrease the serum concentration of Fosamprenavir. Specifically, concentrations of amprenavir (active metabolite) may be decreased. Avoid combination
Fosaprepitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Fosaprepitant. Specifically, CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite aprepitant. Avoid combination
Fosnetupitant: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Fosnetupitant. Avoid combination
Fosphenytoin: RifAMPin may decrease the serum concentration of Fosphenytoin. Management: Seek alternatives when possible. If used together, monitor closely for decreased serum phenytoin concentrations following rifampin initiation/dose increase, or increased concentrations and toxic effects following rifampin discontinuation/dose decrease. Consider therapy modification
Fostamatinib: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Fostamatinib. Avoid combination
Gefitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Gefitinib. Management: In the absence of severe adverse reactions, increase gefitinib dose to 500 mg daily in patients receiving strong CYP3A4 inducers; resume 250 mg dose 7 days after discontinuation of the strong inducer. Carefully monitor clinical response. Consider therapy modification
Gemfibrozil: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. See separate drug interaction monographs for agents listed as exceptions. Monitor therapy
Gemigliptin: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Gemigliptin. CYP3A4 Inducers (Strong) may decrease the serum concentration of Gemigliptin. Avoid combination
Gestrinone: RifAMPin may decrease the serum concentration of Gestrinone. Monitor therapy
Gilteritinib: Combined Inducers of CYP3A4 and P-glycoprotein may decrease the serum concentration of Gilteritinib. Avoid combination
Glasdegib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Glasdegib. Avoid combination
Glecaprevir and Pibrentasvir: RifAMPin may decrease the serum concentration of Glecaprevir and Pibrentasvir. RifAMPin may increase the serum concentration of Glecaprevir and Pibrentasvir. Specifically, a single dose of rifampin may increase glecaprevir/pibrentasvir concentrations, while chronic daily use of rifampin may decrease glecaprevir/pibrentasvir concentrations. Avoid combination
Grazoprevir: RifAMPin may decrease the serum concentration of Grazoprevir. Conversely, single doses of Rifampin may increase Grazoprevir concentrations. Avoid combination
GuanFACINE: CYP3A4 Inducers (Strong) may decrease the serum concentration of GuanFACINE. Management: Increase the guanfacine dose by up to double when initiating guanfacine in a patient taking a strong CYP3A4 inducer. Increase guanfacine dose gradually over 1 to 2 weeks if initiating strong CYP3A4 inducer therapy in a patient already taking guanfacine. Consider therapy modification
HMG-CoA Reductase Inhibitors (Statins): Rifamycin Derivatives may decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Consider use of noninteracting antilipemic agents (note: pitavastatin concentrations may increase with rifamycin treatment). Monitor for altered HMG-CoA reductase inhibitor effects. Rifabutin and fluvastatin, or possibly pravastatin, may pose lower risk. Exceptions: Pitavastatin; Rosuvastatin. Consider therapy modification
HYDROcodone: CYP3A4 Inducers (Strong) may decrease the serum concentration of HYDROcodone. Monitor therapy
Hydrocortisone (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Hydrocortisone (Systemic). Monitor therapy
Ibrutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ibrutinib. Avoid combination
Idelalisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Idelalisib. Avoid combination
Ifosfamide: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Ifosfamide. CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Imatinib: Rifamycin Derivatives may decrease the serum concentration of Imatinib. Management: Avoid concurrent use of imatinib with the rifamycin derivatives when possible. If such a combination must be used, increase imatinib dose by at least 50% and monitor the patient's clinical response closely. Consider therapy modification
Imatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Imatinib. Management: Avoid concurrent use of imatinib with strong CYP3A4 inducers when possible. If such a combination must be used, increase imatinib dose by at least 50% and monitor the patient's clinical response closely. Consider therapy modification
Indinavir: RifAMPin may decrease the serum concentration of Indinavir. Avoid combination
Irinotecan Products: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Irinotecan Products. Specifically, serum concentrations of SN-38 may be reduced. CYP3A4 Inducers (Strong) may decrease the serum concentration of Irinotecan Products. Avoid combination
Isavuconazonium Sulfate: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Isavuconazonium Sulfate. Specifically, CYP3A4 Inducers (Strong) may decrease isavuconazole serum concentrations. Avoid combination
Isoniazid: Rifamycin Derivatives may enhance the hepatotoxic effect of Isoniazid. Even so, this is a frequently employed combination regimen. Monitor therapy
Istradefylline: CYP3A4 Inducers (Strong) may decrease the serum concentration of Istradefylline. Avoid combination
Itraconazole: CYP3A4 Inducers (Strong) may decrease the serum concentration of Itraconazole. Avoid combination
Ivabradine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ivabradine. Avoid combination
Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ivacaftor. Avoid combination
Ivosidenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ivosidenib. Avoid combination
Ixabepilone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ixabepilone. Management: Avoid this combination whenever possible. If this combination must be used, a gradual increase in ixabepilone dose from 40 mg/m2 to 60 mg/m2 (given as a 4-hour infusion), as tolerated, should be considered. Consider therapy modification
Ixazomib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ixazomib. Avoid combination
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
LamoTRIgine: RifAMPin may increase the metabolism of LamoTRIgine. Monitor therapy
Lapatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lapatinib. Management: If therapy overlap cannot be avoided, consider titrating lapatinib gradually from 1,250 mg/day up to 4,500 mg/day (HER2 positive metastatic breast cancer) or 1,500 mg/day up to 5,500 mg/day (hormone receptor/HER2 positive breast cancer) as tolerated. Avoid combination
Larotrectinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Larotrectinib. Management: Avoid use of strong CYP3A4 inducers with larotrectinib. If this combination cannot be avoided, double the larotrectinib dose. Reduced to previous dose after stopping the inducer after a period of 3 to 5 times the inducer half-life. Consider therapy modification
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Ledipasvir: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Ledipasvir. Avoid combination
Lefamulin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin with strong CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lefamulin: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin with P-glycoprotein/ABCB1 inducers unless the benefits outweigh the risks. Consider therapy modification
Lefamulin (Intravenous): CYP3A4 Inducers (Strong) may decrease the serum concentration of Lefamulin (Intravenous). Management: Avoid concomitant use of lefamulin intravenous infusion with strong CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lefamulin (Intravenous): P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Lefamulin (Intravenous). Management: Avoid concomitant use of lefamulin (intravenous) with P-glycoprotein/ABCB1 inducers unless the benefits outweigh the risks. Consider therapy modification
Leflunomide: RifAMPin may increase serum concentrations of the active metabolite(s) of Leflunomide. Monitor therapy
Lemborexant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lemborexant. Avoid combination
Lesinurad: CYP2C9 Inducers (Moderate) may decrease the serum concentration of Lesinurad. Monitor therapy
Letermovir: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Letermovir. Avoid combination
Letermovir: May increase the serum concentration of UGT1A1 Inducers. Avoid combination
Levomethadone: RifAMPin may decrease the serum concentration of Levomethadone. Monitor therapy
LinaGLIPtin: CYP3A4 Inducers (Strong) may decrease the serum concentration of LinaGLIPtin. Management: Strongly consider using an alternative to any strong CYP3A4 inducer in patients who are being treated with linagliptin. If this combination is used, monitor patients closely for evidence of reduced linagliptin effectiveness. Consider therapy modification
LinaGLIPtin: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of LinaGLIPtin. Management: Strongly consider using an alternative to any strong P-glycoprotein inducer in patients who are being treated with linagliptin. If this combination is used, monitor patients closely for evidence of reduced linagliptin effectiveness. Consider therapy modification
Lopinavir: RifAMPin may enhance the adverse/toxic effect of Lopinavir. Specifically, the risk of hepatocellular toxicity may be increased. RifAMPin may decrease the serum concentration of Lopinavir. Avoid combination
Lorlatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lorlatinib. Avoid combination
Lornoxicam: CYP2C9 Inducers (Moderate) may decrease the serum concentration of Lornoxicam. Monitor therapy
Losartan: RifAMPin may decrease the serum concentration of Losartan. Monitor therapy
Lumacaftor and Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lumacaftor and Ivacaftor. Specifically, the serum concentration of ivacaftor may be decreased. Avoid combination
Lumateperone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lumateperone. Avoid combination
Lumefantrine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lumefantrine. Avoid combination
Lurasidone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lurasidone. Avoid combination
Macimorelin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Macimorelin. Avoid combination
Macitentan: CYP3A4 Inducers (Strong) may decrease the serum concentration of Macitentan. Avoid combination
Macrolide Antibiotics: May decrease the metabolism of Rifamycin Derivatives. Exceptions: Azithromycin (Systemic); Fidaxomicin; Roxithromycin; Spiramycin. Consider therapy modification
Manidipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Manidipine. Management: Consider avoiding concomitant use of manidipine and strong CYP3A4 inducers. If combined, monitor closely for decreased manidipine effects and loss of efficacy. Increased manidipine doses may be required. Consider therapy modification
Maraviroc: CYP3A4 Inducers (Strong) may decrease the serum concentration of Maraviroc. Management: Increase maraviroc adult dose to 600 mg twice daily when used with strong CYP3A4 inducers. This does not apply to patients also receiving strong CYP3A4 inhibitors. Do not use maraviroc with strong CYP3A4 inducers in patients with CrCl less than 30 mL/min. Consider therapy modification
Meperidine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Meperidine. Monitor therapy
Methadone: Rifamycin Derivatives may decrease the serum concentration of Methadone. Management: Seek alternatives when possible. If used concomitantly, monitor closely for symptoms of methadone withdrawal upon rifamycin derivative initiation, and for excess sedation upon rifamycin derivative discontinuation. Consider therapy modification
MethylPREDNISolone: CYP3A4 Inducers (Strong) may decrease the serum concentration of MethylPREDNISolone. Management: Consider methylprednisolone dose increases in patients receiving strong CYP3A4 inducers and monitor closely for reduced steroid efficacy. Consider therapy modification
Midostaurin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Midostaurin. Avoid combination
MiFEPRIStone: CYP3A4 Inducers (Strong) may decrease the serum concentration of MiFEPRIStone. Avoid combination
Mirabegron: RifAMPin may decrease the serum concentration of Mirabegron. Monitor therapy
Mirodenafil: CYP3A4 Inducers (Strong) may decrease the serum concentration of Mirodenafil. Management: Consider avoiding the concomitant use of mirodenafil and strong CYP3A4 inducers. If combined, monitor for decreased mirodenafil effects. Mirodenafil dose increases may be required to achieve desired effects. Consider therapy modification
Mirtazapine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Mirtazapine. Monitor therapy
Morphine (Systemic): RifAMPin may decrease the serum concentration of Morphine (Systemic). Monitor therapy
Mycophenolate: Rifamycin Derivatives may decrease the serum concentration of Mycophenolate. Specifically, rifamycin derivatives may decrease the concentration of the active metabolite mycophenolic acid. Avoid combination
Naldemedine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Naldemedine. Avoid combination
Nalmefene: RifAMPin may decrease the serum concentration of Nalmefene. Monitor therapy
Naloxegol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Naloxegol. Avoid combination
Nelfinavir: RifAMPin may decrease the serum concentration of Nelfinavir. Avoid combination
Neratinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Neratinib. Avoid combination
Netupitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Netupitant. Avoid combination
Nevirapine: RifAMPin may decrease the serum concentration of Nevirapine. Management: Avoid whenever possible. When this combination is necessary, use immediate-release nevirapine (avoid extended-release nevirapine) at a dose of 200 mg twice daily with no lead-in (per adult/adolescent HIV guidelines). Monitor nevirapine response closely. Consider therapy modification
NIFEdipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of NIFEdipine. Avoid combination
Nilotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Nilotinib. Avoid combination
NiMODipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of NiMODipine. Avoid combination
Nintedanib: Combined Inducers of CYP3A4 and P-glycoprotein may decrease the serum concentration of Nintedanib. Avoid combination
Nisoldipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Nisoldipine. Avoid combination
Nitrazepam: RifAMPin may decrease the serum concentration of Nitrazepam. Management: Monitor closely for reduced effects of nitrazepam. When possible, consider alternatives to one of these drugs, or increases in initial nitrazepam doses. Consider therapy modification
OLANZapine: RifAMPin may decrease the serum concentration of OLANZapine. Monitor therapy
Olaparib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Olaparib. Avoid combination
Omeprazole: RifAMPin may decrease the serum concentration of Omeprazole. Avoid combination
Osimertinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Osimertinib. Consider therapy modification
OXcarbazepine: CYP3A4 Inducers (Strong) may decrease the serum concentration of OXcarbazepine. Specifically, the concentrations of the 10-monohydroxy active metabolite of oxcarbazepine may be decreased. Monitor therapy
OxyCODONE: RifAMPin may decrease the serum concentration of OxyCODONE. Monitor therapy
Palbociclib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Palbociclib. Avoid combination
Paliperidone: Inducers of CYP3A4 (Strong) and P-glycoprotein may decrease the serum concentration of Paliperidone. Management: Avoid using the 3-month extended-release injectable suspension (Invega Trinza) with inducers of both CYP3A4 and P-glycoprotein during the 3-month dosing interval if possible. If combination is necessary, consider using extended-release tablets. Consider therapy modification
Panobinostat: CYP3A4 Inducers (Strong) may decrease the serum concentration of Panobinostat. Avoid combination
PAZOPanib: CYP3A4 Inducers (Strong) may decrease the serum concentration of PAZOPanib. Avoid combination
Perampanel: CYP3A4 Inducers (Strong) may decrease the serum concentration of Perampanel. Management: Increase the perampanel starting dose to 4 mg/day when perampanel is used concurrently with moderate and strong CYP3A4 inducers. Consider therapy modification
Pexidartinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pexidartinib. Avoid combination
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Substrates: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Exceptions: Betrixaban; Edoxaban. Monitor therapy
Phenytoin: RifAMPin may decrease the serum concentration of Phenytoin. Management: Seek alternatives when possible. If used together, monitor closely for decreased serum phenytoin concentrations following rifampin initiation/dose increase, or increased concentrations and toxic effects following rifampin discontinuation/dose decrease. Consider therapy modification
Pimavanserin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pimavanserin. Avoid combination
Pioglitazone: CYP2C8 Inducers (Moderate) may decrease the serum concentration of Pioglitazone. Monitor therapy
Piperaquine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Piperaquine. Avoid combination
Pitavastatin: Rifamycin Derivatives may increase the serum concentration of Pitavastatin. Management: Limit pitavastatin dose to a maximum of 2 mg/day with concurrent rifampin. Consider therapy modification
Pitolisant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pitolisant. Management: For patients who are stable on pitolisant doses of 8.9 mg or 17.8 mg/day and who are also taking a strong CYP3A4 inducer, increase the pitolisant dose over 7 days to double the original dose (ie, to either 17.8 mg/day or 35.6 mg/day, respectively). Consider therapy modification
Polatuzumab Vedotin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Polatuzumab Vedotin. Exposure to unconjugated MMAE, the cytotoxic small molecule component of polatuzumab vedotin, may be decreased. Monitor therapy
PONATinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of PONATinib. Avoid combination
Prasugrel: RifAMPin may diminish the antiplatelet effect of Prasugrel. Monitor therapy
Pravastatin: RifAMPin may decrease the serum concentration of Pravastatin. Monitor therapy
Praziquantel: CYP3A4 Inducers (Strong) may decrease the serum concentration of Praziquantel. Management: Use of praziquantel with strong CYP3A4 inducers is contraindicated. Discontinue rifampin 4 weeks prior to initiation of praziquantel therapy. Rifampin may be resumed the day following praziquantel completion. Avoid combination
PrednisoLONE (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of PrednisoLONE (Systemic). Monitor therapy
PredniSONE: CYP3A4 Inducers (Strong) may decrease the serum concentration of PredniSONE. Monitor therapy
Pretomanid: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pretomanid. Avoid combination
Progestins (Contraceptive): Rifamycin Derivatives may decrease the serum concentration of Progestins (Contraceptive). Contraceptive failure is possible. Management: Contraceptive failure is possible. Use of an alternative, nonhormonal contraceptive is recommended. Consider therapy modification
Propacetamol: RifAMPin may increase the metabolism of Propacetamol. . This may 1) diminish the desired effects of propacetamol; and 2) increase the risk of liver damage. Monitor therapy
Propafenone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Propafenone. Monitor therapy
Propofol: RifAMPin may enhance the hypotensive effect of Propofol. Management: Note that use of propofol in a patient who has been taking rifampin may result in clinically significant hypotension. If possible, avoid use of this combination. Consider therapy modification
Prothionamide: RifAMPin may enhance the hepatotoxic effect of Prothionamide. Management: Avoid concomitant use of prothionamide and rifampin if possible. If combined use is considered necessary, monitor patients closely for signs and symptoms of hepatotoxicity (eg, jaundice, elevations in liver function tests). Consider therapy modification
Pyrazinamide: May enhance the hepatotoxic effect of RifAMPin. Severe (even fatal) liver injury has been reported in patients receiving these 2 drugs as a 2-month treatment regimen for latent TB infection. Consider therapy modification
QUEtiapine: CYP3A4 Inducers (Strong) may decrease the serum concentration of QUEtiapine. Management: An increase in quetiapine dose (as much as 5 times the regular dose) may be required to maintain therapeutic benefit. Reduce the quetiapine dose back to the previous/regular dose within 7-14 days of discontinuing the inducer. Consider therapy modification
QuiNIDine: Rifamycin Derivatives may decrease the serum concentration of QuiNIDine. Management: Consider alternatives to combination treatment with quinidine and rifampin due to large potential decreases in quinidine concentrations. Monitor for decreased quinidine concentrations/effects with initiation/dose increase of any rifamycin derivative. Consider therapy modification
QuiNINE: RifAMPin may decrease the serum concentration of QuiNINE. Avoid combination
Radotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Radotinib. Management: Consider alternatives to this combination when possible as the risk of radotinib treatment failure may be increased. Consider therapy modification
Raltegravir: RifAMPin may decrease the serum concentration of Raltegravir. Management: Increase raltegravir dose to 800 mg twice daily (adult dose) when used concomitantly with rifampin. Concurrent use of rifampin with once-daily raltegravir (Isentress HD) is not recommended. Consider therapy modification
Ramelteon: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ramelteon. Monitor therapy
Ranolazine: RifAMPin may decrease the serum concentration of Ranolazine. Avoid combination
Reboxetine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Reboxetine. Monitor therapy
Regorafenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Regorafenib. Avoid combination
Repaglinide: RifAMPin may decrease the serum concentration of Repaglinide. Monitor therapy
Revefenacin: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase serum concentrations of the active metabolite(s) of Revefenacin. Avoid combination
Ribociclib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ribociclib. Avoid combination
Rilpivirine: Rifamycin Derivatives may decrease the serum concentration of Rilpivirine. Avoid combination
RisperiDONE: CYP3A4 Inducers (Strong) may decrease the serum concentration of RisperiDONE. Management: Consider increasing the dose of oral risperidone (to no more than double the original dose) if a strong CYP3A4 inducer is initiated. For patients on IM risperidone, consider an increased IM dose or supplemental doses of oral risperidone. Consider therapy modification
Ritonavir: RifAMPin may decrease the serum concentration of Ritonavir. Avoid combination
Rivaroxaban: CYP3A4 Inducers (Strong) may decrease the serum concentration of Rivaroxaban. Avoid combination
Roflumilast: RifAMPin may decrease the serum concentration of Roflumilast. Management: Roflumilast U.S. prescribing information recommends against combining rifampin with roflumilast. The Canadian product monograph makes no such recommendation but notes that rifampin may reduce roflumilast therapeutic effects. Avoid combination
Rolapitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Rolapitant. Management: Avoid rolapitant use in patients requiring chronic administration of strong CYP3A4 inducers. Monitor for reduced rolapitant response and the need for alternative or additional antiemetic therapy even with shorter-term use of such inducers. Consider therapy modification
RomiDEPsin: RifAMPin may increase the serum concentration of RomiDEPsin. Avoid combination
Rosiglitazone: CYP2C8 Inducers (Moderate) may decrease the serum concentration of Rosiglitazone. Monitor therapy
Rosuvastatin: RifAMPin may decrease the serum concentration of Rosuvastatin. Monitor therapy
Ruxolitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ruxolitinib. Monitor therapy
Saquinavir: RifAMPin may enhance the adverse/toxic effect of Saquinavir. Specifically, the risk of hepatocellular toxicity may be increased. RifAMPin may decrease the serum concentration of Saquinavir. Avoid combination
SAXagliptin: CYP3A4 Inducers (Strong) may decrease the serum concentration of SAXagliptin. Monitor therapy
Selexipag: RifAMPin may decrease serum concentrations of the active metabolite(s) of Selexipag. Management: Increase the selexipag dose (up to 2-fold) when combined with rifampin. Monitor for decreased selexipag efficacy. Consider therapy modification
Sertraline: CYP3A4 Inducers (Strong) may decrease the serum concentration of Sertraline. Monitor therapy
Simeprevir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Simeprevir. Avoid combination
Siponimod: RifAMPin may decrease the serum concentration of Siponimod. Management: Coadministration of siponimod with rifampin, a moderate inducer of CYP2C9 and a strong inducer of CYP3A4, is not recommended. Avoid combination
Sirolimus: CYP3A4 Inducers (Strong) may decrease the serum concentration of Sirolimus. Management: Avoid concomitant use of strong CYP3A4 inducers and sirolimus if possible. If combined, monitor for reduced serum sirolimus concentrations. Sirolimus dose increases will likely be necessary to prevent subtherapeutic sirolimus levels. Consider therapy modification
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Sofosbuvir: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Sofosbuvir. Avoid combination
Sonidegib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Sonidegib. Avoid combination
SORAfenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of SORAfenib. Avoid combination
SUFentanil: CYP3A4 Inducers (Strong) may decrease the serum concentration of SUFentanil. Monitor therapy
Sulfamethoxazole: RifAMPin may decrease the serum concentration of Sulfamethoxazole. Monitor therapy
Sulfonylureas: RifAMPin may decrease the serum concentration of Sulfonylureas. Management: Seek alternatives to these combinations when possible. Monitor closely for diminished therapeutic effects of sulfonylureas if rifampin is initiated/dose increased, or enhanced effects if rifampin is discontinued/dose decreased. Consider therapy modification
SUNItinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of SUNItinib. Management: Avoid when possible. If such a combination cannot be avoided, sunitinib dose increases are recommended, and vary by indication. See full monograph for details. Consider therapy modification
Tacrolimus (Systemic): Rifamycin Derivatives may decrease the serum concentration of Tacrolimus (Systemic). Management: Consider alternatives when possible. If these combination are used, monitor for reduced tacrolimus concentrations/effects following rifamycin initiation/dose increase, or increased concentrations/effects following rifamycin discontinuation/dose decrease. Consider therapy modification
Tadalafil: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tadalafil. Management: Erectile dysfunction: monitor for decreased effectiveness - no standard dose adjustments recommended. Avoid use of tadalafil for pulmonary arterial hypertension in patients receiving a strong CYP3A4 inducer. Consider therapy modification
Tamoxifen: Rifamycin Derivatives may increase the metabolism of Tamoxifen. Consider therapy modification
Tamoxifen: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Tamoxifen. CYP3A4 Inducers (Strong) may decrease the serum concentration of Tamoxifen. Management: Consider alternatives to concomitant use of strong CYP3A4 inducers and tamoxifen. If the combination cannot be avoided, monitor for reduced therapeutic effects of tamoxifen. Consider therapy modification
Tasimelteon: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tasimelteon. Avoid combination
Tazemetostat: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tazemetostat. Avoid combination
Telithromycin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Telithromycin. Avoid combination
Temsirolimus: Rifamycin Derivatives may decrease the serum concentration of Temsirolimus. Rifamycins will likely cause an even greater decrease in the concentration of the active metabolite sirolimus. Management: Temsirolimus prescribing information recommends against coadministration with strong CYP3A4 inducers such as rifampin; however, if concurrent therapy is necessary, an increase in temsirolimus adult dose to 50 mg/week should be considered. Consider therapy modification
Temsirolimus: CYP3A4 Inducers (Strong) may decrease the serum concentration of Temsirolimus. Management: Consider increasing the dose of temsirolimus to 50 mg IV/week (from 25 mg IV/week) if a concomitant CYP3A4 strong inducer is necessary. Consider therapy modification
Tenofovir Alafenamide: RifAMPin may decrease the serum concentration of Tenofovir Alafenamide. Avoid combination
Terbinafine (Systemic): RifAMPin may decrease the serum concentration of Terbinafine (Systemic). Monitor therapy
Teriflunomide: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Tertatolol: RifAMPin may decrease the serum concentration of Tertatolol. Monitor therapy
Tetrahydrocannabinol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tetrahydrocannabinol. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tetrahydrocannabinol and Cannabidiol. Monitor therapy
Tezacaftor and Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tezacaftor and Ivacaftor. Avoid combination
Thiotepa: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Thiotepa. CYP3A4 Inducers (Strong) may decrease the serum concentration of Thiotepa. Management: Thiotepa prescribing information recommends avoiding concomitant use of thiotepa and strong CYP3A4 inducers. If concomitant use is unavoidable, monitor for adverse effects. Consider therapy modification
Thyroid Products: RifAMPin may decrease the serum concentration of Thyroid Products. Monitor therapy
TiaGABine: CYP3A4 Inducers (Strong) may decrease the serum concentration of TiaGABine. Management: Approximately 2-fold higher tiagabine doses and a more rapid dose titration will likely be required in patients concomitantly taking a strong CYP3A4 inducer. Consider therapy modification
Ticagrelor: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Ticagrelor. CYP3A4 Inducers (Strong) may decrease the serum concentration of Ticagrelor. Avoid combination
Tipranavir: RifAMPin may decrease the serum concentration of Tipranavir. Avoid combination
Tofacitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tofacitinib. Avoid combination
Tolvaptan: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tolvaptan. Management: If concurrent use is necessary, increased doses of tolvaptan (with close monitoring for toxicity and clinical response) may be needed. Avoid combination
Toremifene: CYP3A4 Inducers (Strong) may decrease the serum concentration of Toremifene. Avoid combination
Trabectedin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Trabectedin. Avoid combination
TraMADol: CYP3A4 Inducers (Strong) may decrease the serum concentration of TraMADol. Monitor therapy
Trimethoprim: RifAMPin may decrease the serum concentration of Trimethoprim. Monitor therapy
Tropisetron: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tropisetron. Monitor therapy
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Ubrogepant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ubrogepant. Avoid combination
Udenafil: CYP3A4 Inducers (Strong) may decrease the serum concentration of Udenafil. Monitor therapy
Ulipristal: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ulipristal. Avoid combination
Upadacitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Upadacitinib. Avoid combination
Valbenazine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Valbenazine. Avoid combination
Valproate Products: RifAMPin may decrease the serum concentration of Valproate Products. Consider therapy modification
Vandetanib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vandetanib. Avoid combination
Velpatasvir: CYP2B6 Inducers (Moderate) may decrease the serum concentration of Velpatasvir. Avoid combination
Velpatasvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Velpatasvir. Avoid combination
Velpatasvir: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Velpatasvir. Avoid combination
Vemurafenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vemurafenib. Management: Avoid concurrent use of vemurafenib with a strong CYP3A4 inducer and replace with another agent when possible. If a strong CYP3A4 inducer is indicated and unavoidable, the dose of vemurafenib may be increased by 240 mg (1 tablet) as tolerated. Consider therapy modification
Venetoclax: CYP3A4 Inducers (Strong) may decrease the serum concentration of Venetoclax. Avoid combination
Vilazodone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vilazodone. Management: Consider increasing vilazodone dose by as much as 2-fold (do not exceed 80 mg/day), based on response, in patients receiving strong CYP3A4 inducers for > 14 days. Reduce to the original vilazodone dose over 1-2 weeks after inducer discontinuation. Consider therapy modification
VinCRIStine (Liposomal): CYP3A4 Inducers (Strong) may decrease the serum concentration of VinCRIStine (Liposomal). Avoid combination
VinCRIStine (Liposomal): P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of VinCRIStine (Liposomal). Avoid combination
Vinflunine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vinflunine. Avoid combination
Vitamin K Antagonists (eg, warfarin): Rifamycin Derivatives may increase the metabolism of Vitamin K Antagonists. Monitor therapy
Vorapaxar: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vorapaxar. Avoid combination
Voriconazole: May increase the serum concentration of Rifamycin Derivatives. Rifamycin Derivatives may decrease the serum concentration of Voriconazole. Avoid combination
Vortioxetine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vortioxetine. Management: Consider increasing the vortioxetine dose to no more than 3 times the original dose when used with a strong drug metabolism inducer for more than 14 days. The vortioxetine dose should be returned to normal within 14 days of stopping the strong inducer. Consider therapy modification
Voxelotor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Voxelotor. Management: Avoid concomitant use of voxelotor and strong CYP3A4 inducers. If concomitant use is unavoidable, increase the voxelotor dose to 2,500 mg once daily. Consider therapy modification
Voxilaprevir: RifAMPin may increase the serum concentration of Voxilaprevir. Specifically, a single dose of rifampin may increase voxilaprevir concentrations, while chronic daily use of rifampin may decrease voxilaprevir concentrations. RifAMPin may decrease the serum concentration of Voxilaprevir. Avoid combination
Zaleplon: CYP3A4 Inducers (Strong) may decrease the serum concentration of Zaleplon. Management: Consider the use of an alternative hypnotic that is not metabolized by CYP3A4 in patients receiving strong CYP3A4 inducers. If zalephon is combined with a strong CYP3A4 inducer, monitor for decreased effectiveness of zaleplon. Consider therapy modification
Zanubrutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Zanubrutinib. Avoid combination
Zidovudine: Rifamycin Derivatives may decrease the serum concentration of Zidovudine. Monitor therapy
Zolpidem: RifAMPin may decrease the serum concentration of Zolpidem. Avoid combination
Zuclopenthixol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Zuclopenthixol. Monitor therapy
Test Interactions
May interfere with urine detection of opioids (false-positive); positive Coombs' reaction [direct], rifampin inhibits standard assay's ability to measure serum folate and B12; transient increase in LFTs and decreased biliary excretion of contrast media
Adverse Reactions
Frequency not defined:
Cardiovascular: Decreased blood pressure, flushing, shock, vasculitis
Central nervous system: Ataxia, behavioral changes, confusion, dizziness, drowsiness, fatigue, headache, lack of concentration, myasthenia, numbness, peripheral pain, sore mouth
Dermatologic: Erythema multiforme, pemphigoid reaction, pruritus, skin rash, urticaria
Endocrine & metabolic: Adrenocortical insufficiency, menstrual disease
Gastrointestinal: Abdominal cramps, anorexia, diarrhea, epigastric discomfort, flatulence, glossalgia, heartburn, nausea, staining of tooth, vomiting
Genitourinary: Hemoglobinuria, hematuria
Hematologic & oncologic: Decreased hemoglobin, disorder of hemostatic components of blood (vitamin K-dependent), disseminated intravascular coagulation, eosinophilia, hemolysis, hemolytic anemia, hemorrhage, leukopenia, thrombocytopenia (especially with high-dose therapy)
Hepatic: Abnormal hepatic function tests, hepatic insufficiency, hyperbilirubinemia, jaundice
Hypersensitivity: Hypersensitivity reaction
Neuromuscular & skeletal: Myopathy
Ophthalmic: Conjunctivitis, visual disturbance
Renal: Acute renal failure, interstitial nephritis, renal insufficiency, renal tubular necrosis
Respiratory: Dyspnea, flu-like symptoms, wheezing
Miscellaneous: Fever
<1%, postmarketing, and/or case reports: Acute generalized exanthematous pustulosis, agranulocytosis, anaphylaxis, cerebral hemorrhage, cholestasis, Clostridioides difficile colitis, cutaneous lupus erythematosus (Patel 2001), drug reaction with eosinophilia and systemic symptoms, facial edema, hepatitis (including shock-like syndrome with hepatic involvement), increased blood urea nitrogen, increased uric acid, peripheral edema, psychosis, severe dermatological reaction, Stevens-Johnson syndrome, toxic epidermal necrolysis
Warnings/Precautions
Concerns related to adverse effects:
- Coagulopathy: May cause vitamin K-dependent coagulation disorders and bleeding. Monitor coagulation tests during treatment in patients at risk of vitamin K deficiency (eg, chronic liver disease, poor nutritional status, prolonged use of antibacterial agents or anticoagulants). Consider discontinuation if abnormal coagulation tests and/or bleeding occurs; consider supplemental vitamin K administration when appropriate.
- Dermatologic reactions: Cases of severe cutaneous adverse reactions (SCAR) such as Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), acute generalized exanthematous pustulosis (AGEP), and drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome have been reported. Discontinue treatment immediately and institute appropriate therapy if signs or symptoms of SCAR develop.
- Flu-like syndrome: Regimens of >600 mg once or twice weekly in adults have been associated with a high incidence of adverse reactions including a flu-like syndrome.
- Hematologic effects: May cause thrombocytopenia, leukopenia, or anemia with regimens >600 mg once or twice weekly in adults.
- Hepatotoxicity: Hepatotoxicity of hepatocellular, cholestatic, and mixed patterns has been reported; may include asymptomatic elevations in liver enzymes, isolated jaundice/hyperbilirubinemia, symptomatic self-limited hepatitis, or fulminant liver failure and death. Severe reactions, including fatalities, have occurred in patients with preexisting hepatic failure and in patients receiving concomitant hepatotoxic agents. Monitor for signs and symptoms of liver injury, especially if treatment is prolonged or given with other hepatotoxic drugs. Patients with impaired liver function should only be given rifampin when medically indicated and with monitoring of LFTs (AST, ALT, bilirubin) prior to therapy and then every 2 to 4 weeks during therapy. Discontinue use if hepatocellular damage occurs or worsens.
- Hypersensitivity: Hypersensitivity reactions have been reported. Signs and symptoms of hypersensitivity reactions may include fever, rash, urticaria, angioedema, hypotension, acute bronchospasm, conjunctivitis, thrombocytopenia, neutropenia, elevated liver transaminases, or flu-like syndrome. Monitor patients for signs/symptoms of hypersensitivity; discontinue therapy if signs/symptoms suggestive of hypersensitivity (eg, fever, lymphadenopathy, eosinophilia, liver abnormalities) occur, even if rash is not evident.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Alcoholism: Use with caution in patients with a history of alcoholism (even if ethanol consumption is discontinued during therapy).
- Diabetes mellitus: Use with caution in patients with diabetes mellitus; management of diabetes may be more difficult in patients taking rifampin.
- Hepatic impairment: Use with caution and close monitoring in patients with hepatic impairment.
- Meningococcal disease: Do not use for treatment of meningococcal disease, only for short-term treatment of asymptomatic carrier states.
- Porphyria: Use with caution in patients with porphyria; exacerbations have been reported due to enzyme-inducing properties.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate administration: Do not administer IV form via IM or SubQ routes; restart infusion at another site if extravasation occurs.
- Compliance: Monitor for compliance in patients on intermittent therapy.
- Contact lenses: Remove soft contact lenses during therapy since permanent staining may occur.
- Discoloration: Teeth (may be permanent), urine, feces, saliva, sweat, and tears may be discolored (yellow, orange, red, or brown).
Monitoring Parameters
Baseline LFTs (AST, ALT, bilirubin), serum creatinine, CBC; periodic (every 2 to 4 weeks during therapy) monitoring of liver function in patients with preexisting hepatic impairment and periodic monitoring of serum creatinine and CBC in patients with baseline abnormalities. Mental status, sputum culture, chest X-ray 2 to 3 months into treatment. Monitor coagulation tests during treatment in patients at risk of vitamin K deficiency.
Pregnancy
Pregnancy Considerations
Rifampin crosses the human placenta. Postnatal hemorrhages have been reported in the infant and mother with administration during the last few weeks of pregnancy.
Maternal treatment of tuberculosis is recommended when the probability of maternal disease is moderate to high due to the risk of infection to the fetus (ATC/CDC 2003). Rifampin may be considered for use as an alternative agent in pregnant women for the treatment of mild illness due to human anaplasmosis (also known as human granulocytic anaplasmosis [HGA]); case reports have shown favorable maternal and pregnancy outcomes in small numbers of rifampin-treated pregnant women (CDC [Biggs 2016]).
Patient Education
What is this drug used for?
- It is used to treat TB (tuberculosis).
- It is used to stop the spread of meningitis in people who carry the bacteria but are not sick with the disease.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Diarrhea
- Fatigue
- Passing gas
- Headache
- Nausea
- Vomiting
- Lack of appetite
- Heartburn
- Abdominal cramps
- Body fluid discoloration
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes
- Severe loss of strength and energy
- Confusion
- Dizziness
- Passing out
- Flu-like symptoms
- Chills
- Sore throat
- Swollen glands
- Joint pain
- Joint swelling
- Muscle pain
- Muscle weakness
- Shortness of breath
- Chest pain
- Cough
- Sweating a lot
- Abnormal heartbeat
- Swelling of arms or legs
- Bruising
- Bleeding
- Pinpoint red spots on skin
- Change in balance
- Trouble focusing
- Behavioral changes
- Menstrual changes
- Vision changes
- Eye pain
- Severe eye irritation
- Severe injection site redness, burning, pain, swelling, or fluid leakage
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Tooth discoloration
- Clostridioides (formerly Clostridium) difficile-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.