Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Suspension, Oral:
Tiglutik: 50 mg/10 mL (300 mL) [contains saccharin sodium]
Tablet, Oral:
Rilutek: 50 mg
Generic: 50 mg
Pharmacology
Mechanism of Action
Mechanism of action is not known. Pharmacologic properties include inhibitory effect on glutamate release, inactivation of voltage-dependent sodium channels; and ability to interfere with intracellular events that follow transmitter binding at excitatory amino acid receptors
Pharmacokinetics/Pharmacodynamics
Absorption
Suspension: High-fat meal decreases AUC by 9% and peak blood levels by 55%.
Tablets: High-fat meal decreases AUC by 20% and peak blood levels by 45%.
Distribution
Vd: ~3.4 L/kg
Metabolism
Hepatic via CYP1A2 and UGT-HP4
Excretion
Urine (90%; 2% as unchanged drug) and feces (5%)
Time to Peak
Suspension: 0.8 hours
Half-Life Elimination
12 hours
Protein Binding
Plasma: 96%, primarily to albumin and lipoproteins
Use in Specific Populations
Special Populations: Hepatic Function Impairment
AUC increased by about 1.7- and 3-fold in patients with mild and moderate chronic hepatic insufficiency, respectively. The pharmacokinetics have not been studied in patients with severe hepatic impairment.
Special Populations: Gender
Mean AUC was found to be 45% higher in women compared with men.
Special Populations: Race
Clearance was 50% lower in male Japanese patients than in white patients.
Special Populations Note
Smoking: Clearance was 20% greater in smokers compared to nonsmokers.
Use: Labeled Indications
Amyotrophic lateral sclerosis: Treatment of patients with amyotrophic lateral sclerosis (ALS); may extend survival and/or time to tracheostomy
Contraindications
Hypersensitivity to riluzole or any component of the formulation
Canadian labeling: Additional contraindications (not in US labeling): Hepatic disease or baseline serum transaminases >3 times ULN; pregnancy; breast-feeding
Dosage and Administration
Dosing: Adult
Amyotrophic lateral sclerosis (ALS): Oral: 50 mg twice daily.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Adjustment for Toxicity
Pulmonary toxicity: If interstitial lung disease develops, discontinue riluzole immediately.
Administration
Oral:
Film: Administer at least 1 hour before or 2 hours after a meal; only one film should be taken at a time. Place film on tongue and allow to dissolve; do not administer with liquids. As film dissolves, swallow saliva in a normal manner but avoid chewing, spitting, or talking. Do not cut or split film.
Suspension, tablet: Administer orally or through a percutaneous endoscopic gastrostomy (PEG) tube (silicone or polyurethane) at least 1 hour before or 2 hours after a meal. Gently shake suspension for ≥30 seconds prior to administration. If administered via PEG tube, flush tube with 30 mL of water before and after administration.
Storage
Store at 20°C to 25°C (68°F to 77°F). Protect from bright light. Use suspension within 15 days after opening bottle; discard unused suspension after 15 days.
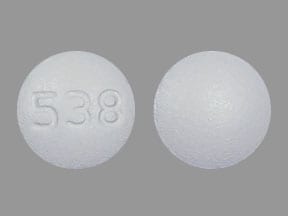
Riluzole Images
Drug Interactions
Allopurinol: May enhance the adverse/toxic effect of Riluzole. Specifically, the risk of hepatotoxicity may be increased. Management: Consider alternatives to allopurinol in patients receiving treatment with riluzole due to the potential for additive hepatotoxicity. Consider therapy modification
Broccoli: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
Cannabis: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
CYP1A2 Inducers (Moderate): May decrease the serum concentration of Riluzole. Monitor therapy
CYP1A2 Inhibitors (Strong): May increase the serum concentration of Riluzole. Monitor therapy
Methyldopa: May enhance the adverse/toxic effect of Riluzole. Specifically, the risk of hepatotoxicity may be increased. Management: Consider alternatives to methyldopa in patients receiving treatment with riluzole due to the potential for additive hepatotoxicity. Consider therapy modification
SulfaSALAzine: May enhance the adverse/toxic effect of Riluzole. Specifically, the risk of hepatotoxicity may be increased. Management: Consider alternatives to sulfasalazine in patients receiving treatment with riluzole due to the potential for additive hepatotoxicity. Consider therapy modification
Tobacco (Smoked): May decrease the serum concentration of Riluzole. Monitor therapy
Adverse Reactions
>10%:
Gastrointestinal: Nausea (16%)
Neuromuscular & skeletal: Weakness (19%)
1% to 10%:
Cardiovascular: Hypertension (5%), peripheral edema (3%), tachycardia (3%)
Central nervous system: Dizziness (4%), drowsiness (2%), vertigo (2%), malaise (1%)
Dermatologic: Pruritus (4%), eczema (2%), exfoliative dermatitis (1%)
Gastrointestinal: Abdominal pain (5%), vomiting (4%), flatulence (3%), oral paresthesia (2%), dental caries (1%), oral candidiasis (1%), stomatitis (1%)
Genitourinary: Urinary tract infection (3%), dysuria (1%)
Hepatic: Increased liver enzymes (>3 x ULN: 8%; >5 x ULN: 2%)
Neuromuscular & skeletal: Arthralgia (4%), tremor (1%)
Respiratory: Decreased lung function (10%), cough (3%)
<1%, postmarketing, and/or case reports (Limited to important or life-threatening): Amblyopia, anaphylactoid reaction, anaphylaxis, angioedema, aplastic anemia, arthropathy, asthma, ataxia, bradycardia, bundle branch block, cardiac failure, cataract, cerebral hemorrhage, deafness, dementia, diabetes mellitus, diabetes insipidus, drug-induced extrapyramidal reaction, edema, erythema multiforme, facial paralysis, gastrointestinal hemorrhage, gastrointestinal ulcer, glaucoma, hallucination, hematemesis, hematuria, hemoptysis, hepatitis, hypercalcemia, hypokalemia, hypokinesia, hyponatremia, hypotension, hypersensitivity pneumonitis, increased gamma-glutamyl transferase, increased lactate dehydrogenase, increased serum alkaline phosphatase, interstitial pulmonary disease, jaundice, leukocytosis, leukopenia, lymphadenopathy, mania, myoclonus, neutropenia, osteonecrosis, osteoporosis, pancreatitis, peripheral neuritis, pleural effusion, pseudomembranous colitis, purpura, respiratory acidosis, seizure, subarachnoid hemorrhage, thrombosis, urinary retention, urticaria, uterine hemorrhage, ventricular fibrillation, ventricular tachycardia
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause dizziness or somnolence; caution should be used performing tasks which require alertness (operating machinery or driving).
- Hepatic effects: May cause drug-induced hepatic injury (including fatality); asymptomatic elevations of hepatic transaminases may also occur. Elevations of transaminases may occur within 3 months of use. Use is not recommended in patients who develop hepatic transaminases >5 times the upper limit of normal. Monitor for signs and symptoms of hepatic injury every month for the first 3 months and periodically thereafter; discontinue use if evidence of hepatic dysfunction occurs (eg, elevated bilirubin).
- Neutropenia: Severe neutropenia has been reported (ANC <500/mm3) within the first 2 months of therapy. Evaluate patients with febrile illnesses.
- Pulmonary disorders: Interstitial lung disease (ILD), including hypersensitivity pneumonitis, has occurred. Discontinue therapy immediately if ILD occurs.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with hepatic impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Monitoring Parameters
Serum aminotransferases including ALT levels before and during therapy; signs and symptoms of hepatic injury every month for the first 3 months and periodically thereafter.
Pregnancy
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies.
Patient Education
What is this drug used for?
- It is used to treat amyotrophic lateral sclerosis (ALS).
Frequently reported side effects of this drug
- Nausea
- Loss of strength and energy
- Abdominal pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Severe pulmonary disorder like lung or breathing problems like difficulty breathing, shortness of breath, or a cough that is new or worse.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Severe dizziness
- Passing out
- Vision changes
- Severe headache
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.