Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Packet, Oral, as carbonate:
Renvela: 0.8 g (1 ea, 90 ea); 2.4 g (1 ea, 90 ea) [citrus flavor]
Generic: 0.8 g (1 ea, 90 ea); 2.4 g (1 ea, 90 ea)
Tablet, Oral, as carbonate:
Renvela: 800 mg
Generic: 800 mg
Tablet, Oral, as hydrochloride:
Renagel: 400 mg [DSC], 800 mg
Generic: 400 mg, 800 mg
Pharmacology
Mechanism of Action
Sevelamer (a polymeric compound) binds phosphate within the intestinal lumen, limiting absorption and decreasing serum phosphate concentrations without altering calcium, aluminum, or bicarbonate concentrations.
Pharmacokinetics/Pharmacodynamics
Absorption
Not systemically absorbed
Excretion
Feces
Onset of Action
Reduction in serum phosphorus has been demonstrated after 1-2 weeks (Burke 1997; Chertow 1997).
Use: Labeled Indications
Control of serum phosphorous: Control of serum phosphorous in patients with chronic kidney disease on hemodialysis
Contraindications
Hypersensitivity to sevelamer or any component of the formulation; bowel obstruction
Canadian labeling: Additional contraindications (not in US labeling): Hypophosphatemia; active mucosal injury (eg, necrosis, perforation, ulcerative colitis, GI bleeding)
Dosage and Administration
Dosing: Adult
Note: The dosing of sevelamer carbonate and sevelamer hydrochloride are similar; when switching from one product to another, the same dose (on a mg per mg basis) should be utilized.
Control of serum phosphorous: Oral:
Patients not taking a phosphate binder: Initial: 800 to 1,600 mg 3 times daily with meals; the initial dose may be based on serum phosphorous levels:
>5.5 mg/dL to <7.5 mg/dL: 800 mg 3 times daily
≥7.5 mg/dL to <9 mg/dL: 1,200 to 1,600 mg 3 times daily
≥9 mg/dL: 1,600 mg 3 times daily
Maintenance dose adjustment based on serum phosphorous concentration (goal range of 3.5 to 5.5 mg/dL; maximum dose studied was equivalent to 13 g/day [sevelamer hydrochloride] or 14 g/day [sevelamer carbonate]):
>5.5 mg/dL: Increase by 400 to 800 mg per meal at 2-week intervals
3.5 to 5.5 mg/dL: Maintain current dose
<3.5 mg/dL: Decrease by 400 to 800 mg per meal
Dosage adjustment when switching between phosphate-binder products: 667 mg of calcium acetate is equivalent to ~800 mg sevelamer (carbonate or hydrochloride)
Conversion based on dose per meal:
Calcium acetate 667 mg: Convert to 800 mg Renagel/Renvela
Calcium acetate 1,334 mg: Convert to 1,600 mg as Renagel/Renvela (800 mg tablets x 2) or 1,200 mg as Renagel (400 mg tablets x 3)
Calcium acetate 2,001 mg: Convert to 2,400 mg as Renagel/Renvela (800 mg tablets x 3) or 2,000 mg as Renagel (400 mg tablets x 5)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Phosphate binding capacity: Sevelamer HCl 400 mg binds ~32 mg of phosphate; 800 mg binds ~64 mg of phosphate (KDOQI 2005)
Hyperphosphatemia:
Sevelamer carbonate (Renvela): Children ≥6 years and Adolescents: Oral:
Patients not taking a phosphate binder: Initial:
BSA ≥0.75 to <1.2 m2: 800 mg 3 times daily with meals; titrate as needed by 400 mg per dose at 2 week intervals.
BSA ≥1.2 m2: 1,600 mg 3 times daily with meals; titrate as needed by 800 mg per dose at 2 week intervals.
Dosage adjustment when switching from calcium acetate to sevelamer carbonate: 667 mg of calcium acetate is equivalent to ~800 mg sevelamer; conversion based on dose per meal:
Calcium acetate 667 mg: Convert to 800 mg sevelamer carbonate
Calcium acetate 1,334 mg: Convert to 1,600 mg sevelamer carbonate
Calcium acetate 2,001 mg: Convert to 2,400 mg sevelamer carbonate
Sevelamer hydrochloride (Renagel): Limited data available:
Infants ≥10 months and Children <2 years: Oral: Mean final dose: 140 ± 86 mg/kg/day (5.38 ± 3.24 g/day) was reported in a small trial (n=18, age range: 10 months to 18 years) to achieve the targeted serum phosphorus level. Initial dosing was based upon prior phosphate binder dose and serum phosphorus concentrations (Pieper 2006). In a case report of a 19-month old, an initial dose of 100 mg/kg/day divided every 8 hours with titration up to 130 mg/kg/day was reported to effectively lower serum phosphorus levels (Storms 2006).
Children ≥2 years and Adolescents: Oral: Initial dose: 400 or 800 mg 3 times daily administered with meals; titrate at monthly intervals in 1,200 mg/day increments (ie, 400 mg at each meal) to target phosphorus level; final mean range: 140 to 163 mg/kg/day (5.38 to 6.7 g/day); dosing based on experience in 46 patients; prior or final comparative calcium salt phosphate-binder dose: 4 ± 3 g/day (Gulati 2010; Mahdavi 2003; Pieper 2006).
Dosage adjustment when switching from calcium acetate to sevelamer hydrochloride: 667 mg of calcium acetate is equivalent to ~800 mg sevelamer; conversion based on dose per meal.
Hyperphosphatemia, pretreatment of oral and enteral nutrition: Limited data available: Oral: 800 mg (tablets or powder) added to up to 400 mL of breast milk or 100 mL of infant formula, tube feeding, and cow's milk; after sitting for 10 minutes, decant liquid from the precipitate at the bottom; reported experience has shown a decrease in phosphate of >85% in breast milk, 42% in cow's milk, 48% in tube feeding, and 68% in infant formula (KDOQI 2009; Raaijmakers 2013)
Reconstitution
Powder for oral suspension:
Mix powder with water prior to administration. Mix the 0.8 g packet (or half of packet for 0.4 g) with 30 mL of water and mix the 2.4 g packet with 60 mL of water (multiple packets may be mixed together using the appropriate amount of water). Suspension must be consumed within 30 minutes of preparation.
As an alternative to an oral suspension in water, the contents of the packet may be pre-mixed with a small amount of food or beverage and consumed immediately (or within 30 minutes) as part of a meal. Do not heat or add to heated food or liquid.
Extemporaneously Prepared
Note: An oral suspension product is commercially available. Sevelamer carbonate is commercially available as powder for oral suspension packets; however, it is a different salt form than described below:
50 mg/mL Sevelamer Hydrochloride Oral Suspension
A 50 mg/mL oral suspension may be made with tablets, distilled water, and simple syrup. Place fifteen 800 mg sevelamer hydrochloride tablets in a beaker with 120 mL of distilled water. Allow tablets to soak and disintegrate; stir occasionally. Add ~60 mL of simple syrup to the beaker and mix until a uniform suspension is achieved. Pour mixture into a calibrated cylinder and add quantity of simple syrup sufficient to make 240 mL. Pour mixture back into beaker and stir until thoroughly mixed. Transfer to amber bottle. Stable for 14 days under refrigeration. Label "shake well."
McElhiney LF. Sevelamer suspension in children with end-stage renal disease. Int J Pharm Compd. 2007;11(1):20-24.23974479
Administration
Administer with meals.
Powder for oral suspension: May prepare an oral suspension in water using the directed amount of water appropriate for the packet size or may premix the entire content of the packet with a small amount of food or beverage (do not heat or add to heated foods or liquids).
Preparations should be consumed immediately or within 30 minutes. Oral suspension in water may need to be resuspended immediately before drinking.
Tablets: Swallow whole; do not crush, chew, or break.
Dietary Considerations
Take with meals. Reduced levels of folic acid, and vitamins D, E, and K may occur; most hemodialysis patients in clinical trials received vitamin supplementation.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from moisture.
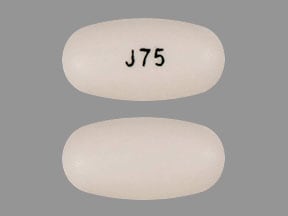
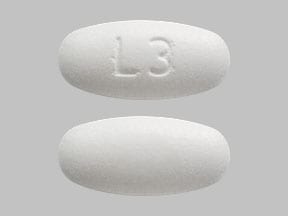
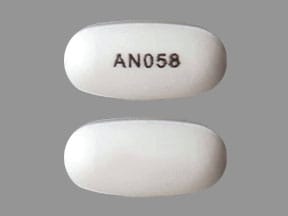
Sevelamer Images
Drug Interactions
Calcitriol (Systemic): Sevelamer may decrease the serum concentration of Calcitriol (Systemic). Monitor therapy
Cholic Acid: Sevelamer may decrease the absorption of Cholic Acid. Management: Administer cholic acid at least 1 hour before or 4 to 6 hours after administration of any bile acid-binding products, such as sevelamer, to minimize the potential for a significant interaction. Consider therapy modification
CycloSPORINE (Systemic): Sevelamer may decrease the serum concentration of CycloSPORINE (Systemic). Monitor therapy
Levothyroxine: Sevelamer may decrease the serum concentration of Levothyroxine. Management: Consider separating administration of sevelamer and levothyroxine by at least several hours whenever possible in order to decrease the risk of a significant interaction. Consider therapy modification
Mycophenolate: Sevelamer may decrease the serum concentration of Mycophenolate. Management: Administer mycophenolate at least 2 hours prior to sevelamer administration. Consider therapy modification
Quinolones: Sevelamer may decrease the absorption of Quinolones. Management: Administer oral quinolones at least 2 hours before or 6 hours after sevelamer. Exceptions: LevoFLOXacin (Oral Inhalation). Consider therapy modification
Tacrolimus (Systemic): Sevelamer may decrease the serum concentration of Tacrolimus (Systemic). Monitor therapy
Adverse Reactions
>10%:
Endocrine & metabolic: Metabolic acidosis (children: 34% [Pieper 2006]); adults: Frequency not defined)
Gastrointestinal: Vomiting (22%), nausea (20%), diarrhea (19%), dyspepsia (16%)
1% to 10%:
Gastrointestinal: Abdominal pain (9%), constipation (8%), flatulence (8%), peritonitis (peritoneal dialysis: 8%)
<1%, postmarketing, and/or case reports: Fecal impaction, hypersensitivity reaction, intestinal obstruction (rare), intestinal perforation (rare), pruritus, skin rash
Warnings/Precautions
Concerns related to adverse effects:
- Gastrointestinal effects: Bowel obstruction and perforation have been reported. Dysphagia and esophageal tablet retention have also been reported with the tablet formulation; consider change to suspension formulation in patients with a history of swallowing disorders
Disease-related concerns:
- Gastrointestinal disease: Use with caution in patients with gastrointestinal disorders including dysphagia, swallowing disorders, severe gastrointestinal motility disorders (including severe constipation), or major gastrointestinal surgery.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions for more detailed information
- Vitamins: May cause reductions in vitamin D, E, K, or folic acid absorption.
Dosage form specific issues:
- Tablets: Should not be taken apart or chewed; broken or crushed tablets will rapidly expand in water/saliva and may be a choking hazard.
Monitoring Parameters
Serum chemistries, including bicarbonate and chloride
Serum calcium, phosphorus, and parathyroid hormone (PTH): Frequency of measurement may be dependent upon the presence and magnitude of abnormalities, the rate of progression of chronic kidney disease (CKD), and the use of treatments for chronic kidney disease-mineral and bone disorder (CKD-MBD) (KDIGO 2017):
CKD stage G3a to G3b: Serum calcium and phosphate: Every 6 to 12 months; PTH: Frequency based on baseline level and progression of CKD
CKD stage G4: Serum calcium and phosphate: Every 3 to 6 months; PTH: Every 6 to 12 months
CKD stage G5 and G5D: Serum calcium and phosphate: Every 1 to 3 months; PTH: Every 3 to 6 months
Periodic 24-hour urinary calcium and phosphorus; magnesium; alkaline phosphatase every 12 months or more frequently in the presence of elevated PTH; creatinine, BUN, albumin; intact parathyroid hormone (iPTH) every 3 to 12 months depending on CKD severity
Pregnancy
Pregnancy Considerations
Sevelamer is not absorbed systemically; however, it may reduce maternal absorption of fat soluble vitamins and folic acid; supplementation may be needed.
Patient Education
What is this drug used for?
- It is used to lower high phosphate levels.
Frequently reported side effects of this drug
- Diarrhea
- Passing gas
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe constipation
- Severe nausea
- Vomiting
- Severe abdominal pain
- Difficulty swallowing
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.