Boxed Warning
Immunosuppression:
Increased susceptibility to infection and the possible development of lymphoma and other malignancies may result from immunosuppression.
Experienced physician:
Only physicians experienced in immunosuppressive therapy and management of renal transplant patients should use sirolimus for prophylaxis of organ rejection in patients receiving renal transplants. Patients receiving sirolimus should be managed in facilities equipped and staffed with adequate laboratory and supportive medical resources. The physician responsible for maintenance therapy should have complete information requisite for the follow-up of the patient.
Liver transplantation:
The use of sirolimus in combination with tacrolimus was associated with excess mortality and graft loss in a study in de novo liver transplant patients. Many of these patients had evidence of infection at or near the time of death. In this and another study in de novo liver transplant patients, the use of sirolimus in combination with cyclosporine or tacrolimus was associated with an increase in hepatic artery thrombosis; most cases of hepatic artery thrombosis occurred within 30 days posttransplantation, and most led to graft loss or death. The safety and efficacy of sirolimus as immunosuppressive therapy have not been established in liver transplant patients; therefore, such use is not recommended.
Lung transplantation:
Cases of bronchial anastomotic dehiscence, most fatal, have been reported in de novo lung transplant patients when sirolimus has been used as part of an immunosuppressive regimen. The safety and efficacy of sirolimus as immunosuppressive therapy have not been established in lung transplant patients; therefore, such use is not recommended.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Oral:
Rapamune: 1 mg/mL (60 mL) [contains alcohol, usp]
Generic: 1 mg/mL (60 mL)
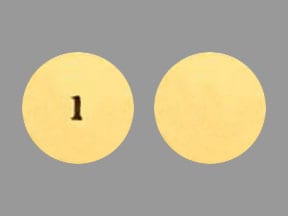
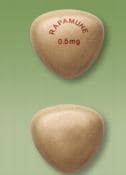
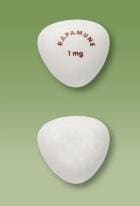
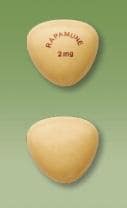
Tablet, Oral:
Rapamune: 0.5 mg, 1 mg, 2 mg
Generic: 0.5 mg, 1 mg, 2 mg
Pharmacology
Mechanism of Action
Sirolimus inhibits T-lymphocyte activation and proliferation in response to antigenic and cytokine stimulation and inhibits antibody production. Its mechanism differs from other immunosuppressants. Sirolimus binds to FKBP-12, an intracellular protein, to form an immunosuppressive complex which inhibits the regulatory kinase, mTOR (mechanistic target of rapamycin). This inhibition suppresses cytokine mediated T-cell proliferation, halting progression from the G1 to the S phase of the cell cycle. It inhibits acute rejection of allografts and prolongs graft survival.
In lymphangioleiomyomatosis, the mTOR signaling pathway is activated through the loss of the tuberous sclerosis complex (TSC) gene function (resulting in cellular proliferation and release of lymphangiogenic growth factors). By inhibiting the mTOR pathway, sirolimus prevents the proliferation of lymphangioleiomyomatosis cells.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
12 L/kg (range: 4 to 20 L/kg)
Metabolism
Extensive; in intestinal wall via P-glycoprotein and hepatic via CYP3A4 to 7 major metabolites
Excretion
Feces (91% via P-glycoprotein-mediated efflux into gut lumen); urine (2%)
Time to Peak
Oral solution: 1 to 3 hours; Tablet: 1 to 6 hours
Half-Life Elimination
Children: 13.7 ± 6.2 hours
Adults: Mean: 62 hours (range; 46 to 78 hours); extended in hepatic impairment (Child-Pugh class A or B) to 113 hours
Protein Binding
~92%, primarily to albumin
Use in Specific Populations
Special Populations: Renal Function Impairment
Minimal (2.2%) renal excretion of the drug and its metabolites.
Special Populations: Hepatic Function Impairment
Patients with mild, moderate, and severe hepatic impairment had 43%, 94%, and 189% higher mean values for sirolimus AUC, respectively, with no statistically significant differences in mean Cmax. As the severity of hepatic impairment increased, there were steady increases in mean sirolimus half-life and decreases in the mean sirolimus clearance normalized for body weight.
Special Populations: Gender
Clearance is 12% lower and the half-life is prolonged in men compared with women (~72 hours versus ~61 hours, respectively).
Use: Labeled Indications
Lymphangioleiomyomatosis: Treatment of lymphangioleiomyomatosis. Therapeutic drug monitoring is recommended for all patients receiving sirolimus.
Renal transplantation (rejection prophylaxis): Prophylaxis of organ rejection in patients receiving renal transplants (in low-to-moderate immunologic risk patients in combination with cyclosporine and corticosteroids with cyclosporine withdrawn 2 to 4 months after transplant, and in high immunologic risk patients in combination with cyclosporine and corticosteroids for the first year after transplant). Therapeutic drug monitoring is recommended for all patients receiving sirolimus. High immunologic risk renal transplant patients are defined (per the manufacturer's labeling) as Black transplant recipients and/or repeat renal transplant recipients who lost a previous allograft based on an immunologic process and/or patients with high PRA (panel-reactive antibodies; peak PRA level >80%).
Limitations of use (renal transplantation): Cyclosporine withdrawal has not been studied in patients with Banff grade 3 acute rejection or vascular rejection prior to cyclosporine withdrawal, patients who are dialysis-dependent, patients with serum creatinine >4.5 mg/dL, Black patients, patients with multiorgan transplants or secondary transplants, or those with high levels of PRA. In patients at high immunologic risk, the safety and efficacy of sirolimus used in combination with cyclosporine and corticosteroids have not been studied beyond 1 year; therefore, after the first 12 months following transplantation, consider any adjustments to the immunosuppressive regimen on the basis of the clinical status of the patient. The safety and efficacy of sirolimus have not been established in patients younger than 13 years or in pediatric renal transplant patients younger than 18 years who are considered at high immunologic risk. The Kidney Disease: Improving Global Outcomes (KDIGO) guidelines for the care of renal transplant recipients recommend not initiating sirolimus until graft function has been established and surgical wounds have healed (KDIGO 2009). Avoid the use of sirolimus in combination with calcineurin inhibitors, particularly in the early posttransplant period due to an increased risk of nephrotoxicity (KDIGO 2009; Webster 2006).
Use: Off Label
Chordoma (advanced)c
Data from a limited number of patients with advanced chordoma (case series) suggests that sirolimus may be beneficial for the treatment of this condition Stacchiotti 2009. Additional data is necessary to further define the role of sirolimus in this condition.
Graft-versus-host disease preventionb
Data from one retrospective analysis and data from an open-label trial in patients who underwent hematopoietic stem cell transplantation for lymphoma suggests that sirolimus (in combination with tacrolimus) may be beneficial for the prevention of graft-versus-host disease (GVHD) after transplantation Armand 2008, Cutler 2007. Additional trials may be necessary to further define the role of sirolimus in this setting.
Acute graft-versus-host disease treatmentc
Data from a pilot study conducted in patients with acute graft-versus-host disease (GVHD) after allogeneic hematopoietic stem cell transplantation suggests that sirolimus may be an effective treatment option in patients with this condition Benito 2001. Additional trials may be necessary to further define the role of sirolimus in this condition.
Chronic graft-versus-host disease treatmentc
Data from a phase II open-label trial in patients with steroid-resistant chronic graft-versus-host disease (GVHD) suggests that sirolimus (in combination with tacrolimus and corticosteroids) may be beneficial in the treatment of this condition Couriel 2005. Additional trials may be necessary to further define the role of sirolimus in this condition.
Heart transplant (prophylaxis of organ rejection and allograft vasculopathy)byes
Data from an open-label, prospective, randomized trial in patients with graft arteriosclerosis using sirolimus versus standard care supports the use of sirolimus for the prophylaxis of organ rejection and allograft vasculopathy in heart transplant recipients Mancini 2003. Additionally, data from a randomized, controlled, parallel-group, multicenter, open-label trial and a small prospective trial of conversion from a calcineurin inhibitor (cyclosporine or tacrolimus) to sirolimus supports the use of sirolimus in this setting Kushwaha 2005, Zuckermann 2012. Substituting sirolimus for a calcineurin inhibitor (in combination with steroids and an antiproliferative immunosuppressive agent) may lead to improved short- and long-term renal function without compromising cardiac allograft function or the incidence of rejection Gustafsson 2007, Hunt 2005. Sirolimus also may attenuate cardiac allograft vasculopathy (CAV) progression and improve cardiac-related events and long-term survival Raichlin 2007b, Topilsky 2012.
Based on the The International Society for Heart & Lung Transplantation (ISHLT) Guidelines for the Care of Heart Transplant Recipients, the substitution of a calcineurin inhibitor later than 6 months after heart transplant is effective and recommended to reduce CNI-related nephrotoxicity and cardiac allograft vasculopathy in low-risk patients.
Lung transplantation (rejection prophylaxis)c
Data from a small single center study suggests that sirolimus may be used as an alternative immunosuppressant in lung transplant patients who develop renal impairment due to calcineurin inhibitor therapy Snell 2002. Additional trials may be necessary to further define the role of sirolimus in this condition.
Renal angiomyolipomab
Data from a multicenter phase II nonrandomized open label trial in patients with renal angiomyolipoma due to lymphangioleiomyomatosis or tuberous sclerosis supports the use of sirolimus for this condition Davies 2011.
Contraindications
Hypersensitivity to sirolimus or any component of the formulation
Dosage and Administration
Dosing: Adult
Lymphangioleiomyomatosis: Adults: Oral: Initial: 2 mg once daily. Obtain trough concentration in 10 to 20 days; adjust dose to maintain a target concentration of 5 to 15 ng/mL.
Dosage adjustment for lymphangioleiomyomatosis: Once the maintenance dose is adjusted, further adjustments should be made at 7- to 14-day intervals to account for the long half-life of sirolimus. In general, dose proportionality may be assumed. New sirolimus dose equals current dose multiplied by (target concentration divided by current concentration). Once a stable dose is achieved, trough concentrations should be assessed at least every 3 months.
Renal transplant (rejection prophylaxis): Oral:
Low-to-moderate immunologic risk:
<40 kg: Loading dose: 3 mg/m2 on day 1, followed by maintenance dosing of 1 mg/m2 once daily
≥40 kg: Loading dose: 6 mg on day 1; maintenance: 2 mg once daily
High immunologic risk: Loading dose: Up to 15 mg on day 1; maintenance: 5 mg/day; obtain trough concentration between days 5 to 7 and adjust accordingly. Continue concurrent cyclosporine/sirolimus/corticosteroid therapy for 1 year following transplantation. Further adjustment of the regimen must be based on clinical status.
Dosage adjustment for renal transplantation: Sirolimus dosages should be adjusted in small increments to maintain 24-hour trough concentrations within desired range based on risk and concomitant therapy. Dosage should be adjusted at intervals of 7 to 14 days to account for the long half-life of sirolimus. Maximum loading dose: 40 mg/day (although typical loading doses are not generally this high). Whole blood concentrations should not be used as the sole basis for dosage adjustment (monitor clinical signs/symptoms, tissue biopsy, and laboratory parameters).
Maintenance therapy after withdrawal of cyclosporine: According to the manufacturer, cyclosporine withdrawal is not recommended in high immunological risk renal transplant patients. Following 2 to 4 months of combined therapy, withdrawal of cyclosporine may be considered in low-to-moderate immunologic risk patients. Cyclosporine should be discontinued over 4 to 8 weeks, and a necessary increase in the dosage of sirolimus (up to fourfold) should be anticipated due to removal of metabolic inhibition by cyclosporine and to maintain adequate immunosuppressive effects. Dose-adjusted trough target concentrations are typically 16 to 24 ng/mL for the first year post-transplant and 12 to 20 ng/mL thereafter (per the manufacturer; measured by chromatographic methodology). Target trough concentrations of ~5 to 15 ng/mL are often used in clinical practice (Kahan 2000; Stenton 2005); refer to specific institutional protocol for target sirolimus trough concentrations.
Graft-versus-host disease (GVHD) (off-label use): Oral:
GVHD (prevention): 12 mg loading dose on day -3, followed by 4 mg daily (target trough level: 3 to 12 ng/mL); taper off after 6 to 9 months (Armand 2008; Cutler 2007). Additional trials may be necessary to further define the role of sirolimus in this condition.
Treatment of refractory acute GVHD: 4 to 5 mg/m2 for 14 days (no loading dose) (Benito 2001). Additional trials may be necessary to further define the role of sirolimus in this condition.
Treatment of chronic GVHD: 6 mg loading dose, followed by 2 mg daily (target trough level: 7 to 12 ng/mL) for 6 to 9 months (Couriel 2005). Additional trials may be necessary to further define the role of sirolimus in this condition.
Heart transplantation (prophylaxis of organ rejection and allograft vasculopathy) (off-label use): Oral: Note: The use of sirolimus in the immediate post-cardiac transplant period (ie, de novo heart transplant) as a primary immunosuppressant has fallen out of favor due to adverse effects (eg, impaired wound healing and infection); however, patients may be converted to sirolimus from a calcineurin inhibitor (after at least 6 months from time of transplant [Costanzo 2010]).
Conversion from a calcineurin inhibitor (CNI) (ie, cyclosporine, tacrolimus): Reduce cyclosporine by 25 mg twice daily or tacrolimus by 1 mg twice daily followed by initiation of sirolimus 1 mg once daily; adjust sirolimus dose to target trough level of 8 to 14 ng/mL, withdraw CNI, repeat biopsy 2 weeks after CNI withdrawal (Topilsky 2012). Alternatively, maintain CNI concentrations and initiate sirolimus 1 mg once daily for 1 week; adjust sirolimus to target trough levels of 10 to 15 ng/mL over 2 weeks, then reduce CNI to target 50% of therapeutic concentrations and after 2 weeks evaluate for rejection. If no rejection, continue same regimen for an additional month, then reduce CNI to 25% of therapeutic concentrations with repeat biopsy 2 weeks later; if no rejection, may discontinue CNI after 2 weeks and continue to maintain sirolimus trough levels of 10 to 15 ng/mL (usual doses required to maintain target levels: 1 to 8 mg daily) (Kushwaha 2005). Refer to specific institutional protocol for target sirolimus trough concentrations; trough will vary based on time from transplant, assay method, and concurrent or transitioning therapies.
Conversion from antiproliferative immunosuppressive drug (ie, azathioprine or mycophenolate) while maintaining calcineurin inhibitor: Upon discontinuation of antiproliferative, administer sirolimus 6 mg loading dose followed by 2 mg once daily titrated to a target trough level of 4 to 15 ng/mL (Mancini 2003) or 4 to 12 ng/mL per ISHLT recommendations (Costanzo 2010).
Lung transplantation (rejection prophylaxis) (off-label use): Oral: Initial loading dose: 5 mg once, followed by a maintenance dose of 3 mg once daily; titrate to a target trough level of 5 to 13 ng/mL (Snell 2002). Do not initiate sirolimus until after the bronchial anastomosis has completely healed (approximately 90 days) due to potential fatal airway dehiscence with earlier initiation (King-Biggs 2003). Additional trials may be necessary to further define the role of sirolimus in this condition.
Renal angiomyolipoma (off-label use): Oral: Initial: 0.5 mg/m2 once daily titrated to a target trough level of 3 to 6 ng/mL (may increase to target trough level of 6 to 10 ng/mL if <10% reduction in lesion diameters at 2 months) for 2 years (Davies 2011)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Sirolimus tablets and oral solution are not bioequivalent due to differences in absorption; however, clinical equivalence has been demonstrated at the 2 mg dose. Dosage should be individualized and based on monitoring of serum trough concentrations; target range is variable and may depend upon transplantation type, length of time since transplant, renal function, infection, rejection history, drug combinations used, and side effects of individual agents.
Heart transplantation: Limited data available: Children and Adolescents: Oral: Note: Not used first-line; most data describes as alternative immunosuppression in combination with either cyclosporine or tacrolimus in patients for renal-sparing effects, following retransplantation (treatment of rejection) or to prevent or promote regression of transplant coronary artery disease (Denfield, 2010)
BSA/weight-directed dosing:
Loading dose: 3 mg/m2 on day 1 (Balfour, 2006; Denfield, 2010)
Maintenance dose: Evaluate serum trough concentrations and adjust dose to overall target range: 4-12 ng/mL (ISHLT, Costanzo 2010). Some trials report using lower target ranges of 4-10 ng/mL (Chinnock, 2011; Lobach, 2005; Matthews, 2010). In children, a specific maintenance dose has not been reported in the majority of trials. In 16 pediatric patients (age range: 2-18 years), the mean reported dose to reach target serum concentration of 5-10 ng/mL was 7 mg/m2 (or 0.25 mg/kg) (Lobach, 2005). One trial used an initial median dose of 1 mg once daily (range: 0.3-2 mg once daily) and adjusted to achieve target concentration of 4-8 ng/mL (final dosage range 0.3-4 mg once daily) (Matthews, 2010). In adolescents <40 kg, an initial maintenance dose of 1 mg/m2/day in 1-2 divided doses has been suggested (Denfield, 2010).
Alternative fixed dosing: Adolescents with weight ≥40 kg: Loading dose: 6 mg on day 1; then maintenance: 2 mg once daily; evaluate serum trough concentrations and adjust dose to overall target range: 4-12 ng/mL (Denfield, 2010; ISHLT Costanzo, 2010); some suggest higher initial targets when sirolimus therapy initiated and then decrease to 4-8 ng/mL (Balfour, 2005; Chinnock, 2011; Lobach, 2005).
Renal transplantation, prophylaxis of organ rejection (low to moderate immunologic risk): Oral:
Conversion from tacrolimus in patients with stable graft function: Children and Adolescents: Limited data available: Initial maintenance dose: 3 mg/m2/day divided every 12 hours; adjust dose to achieve target sirolimus serum trough concentration (Hymes, 2008; Hymes, 2011). In one trial, a loading dose of 5 mg/m2 on day 1 was used, followed by maintenance doses of 3 mg/m2/day divided every 12 hours (Hymes, 2008).
Manufacturer's recommendations: Adolescents:
Weight <40 kg: Loading dose: 3 mg/m2 on day 1; initial maintenance dose: 1 mg/m2/day divided every 12 hours or once daily; adjust dose to achieve target sirolimus trough blood concentration
Weight ≥40 kg: Loading dose: 6 mg on day 1; maintenance: 2 mg once daily; adjust dose to achieve target sirolimus trough blood concentration.
Dosage adjustment: Sirolimus dosages should be adjusted to maintain trough concentrations within desired range based on risk and concomitant therapy; maximum daily dose: 40 mg/day. Dosage should be adjusted at intervals of 7-14 days to account for the long half-life of sirolimus; in children receiving twice-daily dosing, serum concentrations should be checked earlier due to pharmacokinetic differences. In general, dose proportionality may be assumed. New sirolimus dose equals current dose multiplied by (target concentration/current concentration). Note: If large dose increase is required, consider loading dose calculated as:
Loading dose equals (new maintenance dose minus current maintenance dose) multiplied by 3
Maximum daily dose: 40 mg/day; if required dose is >40 mg (due to loading dose), divide over 2 days. Serum concentrations should not be used as the sole basis for dosage adjustment (monitor clinical signs/symptoms, tissue biopsy, and laboratory parameters).
Maintenance therapy after withdrawal of cyclosporine: Following 2-4 months of combined therapy, withdrawal of cyclosporine may be considered in low to moderate risk patients. Cyclosporine should be discontinued over 4-8 weeks, and a necessary increase in the dosage of sirolimus (up to fourfold) should be anticipated due to removal of metabolic inhibition by cyclosporine and to maintain adequate immunosuppressive effects.
Vascular anomalies/tumors (eg, Kaposiform hemangioendothelioma); refractory: Very limited data available: Infants ≥7 months, Children, and Adolescents ≤14 years: Oral: Oral solution: Initial: 0.8 mg/m2 twice daily (approximately every 12 hours); titrate to a serum trough concentration of 10-15 ng/mL; dosing based on a pilot case series (n=6), the mean response time was 25 days (range: 8-65 days) (Hammill, 2011).
Administration
Administer consistently (either with or without food). Renal transplant: Sirolimus should be taken 4 hours after oral cyclosporine (Neoral or Gengraf).
Solution: Mix (by stirring vigorously) with at least 60 mL of water or orange juice. No other liquids should be used for dilution. Patient should drink diluted solution immediately. The cup should then be refilled with an additional 120 mL of water or orange juice, stirred vigorously, and the patient should drink the contents at once.
Tablet: Do not crush, split, or chew.
Storage
Oral solution: Store at 2°C to 8°C (36°F to 46°F). Protect from light. A slight haze may develop in refrigerated solutions, but the quality of the product is not affected. After opening, solution should be used within 1 month. If necessary, may be stored at temperatures up to 25°C (77°F) for ≤15 days after opening. Product may be stored in amber syringe for a maximum of 24 hours (at room temperature or refrigerated). Discard syringe after single use. Solution should be used immediately following dilution.
Tablet: Store at 20°C to 25°C (68°F to 77°F). Protect from light.
Sirolimus Images
Drug Interactions
Angiotensin-Converting Enzyme Inhibitors: Sirolimus may enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Antihepaciviral Combination Products: May increase the serum concentration of Sirolimus. Avoid combination
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Clotrimazole (Topical): May increase the serum concentration of Sirolimus. Monitor therapy
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Crizotinib: May increase the serum concentration of Sirolimus. Avoid combination
CycloSPORINE (Systemic): Sirolimus may enhance the adverse/toxic effect of CycloSPORINE (Systemic). An increased risk of calcineurin inhibitor-induced hemolytic uremic syndrome/thrombotic thrombocytopenic purpura/thrombotic microangiopathy (HUS/TTP/TMA) has been described. CycloSPORINE (Systemic) may increase the serum concentration of Sirolimus. This is of specific concern with cyclosporine [MODIFIED]. Management: Administer oral doses of sirolimus 4 hours after doses of cyclosporine. Monitor for toxic effects of sirolimus if used with cyclosporine. Consider therapy modification
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Sirolimus. Management: Avoid concomitant use of strong CYP3A4 inducers and sirolimus if possible. If combined, monitor for reduced serum sirolimus concentrations. Sirolimus dose increases will likely be necessary to prevent subtherapeutic sirolimus levels. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Sirolimus. Management: Monitor for increased serum concentrations of sirolimus if combined with a moderate CYP3A4 inhibitor. Lower initial sirolimus doses or sirolimus dose reductions will likely be required. Consider therapy modification
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Sirolimus. Management: Consider avoiding concurrent use of sirolimus with strong CYP3A4 inhibitors in order to minimize the risk for sirolimus toxicity. Concomitant use of sirolimus and voriconazole or posaconazole is contraindicated. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Efavirenz: May decrease the serum concentration of Sirolimus. Management: Closely monitor sirolimus serum concentrations when starting, stopping, or changing doses of efavirenz, particularly during the first 2 weeks after any change. Dose adjustment of sirolimus may be required. Consider therapy modification
Enzalutamide: May decrease the serum concentration of Sirolimus. Avoid combination
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Erythromycin (Systemic): May increase the serum concentration of Sirolimus. Sirolimus may increase the serum concentration of Erythromycin (Systemic). Management: Monitor for increased serum concentrations of sirolimus if combined with erythromycin. Lower initial sirolimus doses or sirolimus dose reductions will likely be required. Consider therapy modification
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Fluconazole: May increase the serum concentration of Sirolimus. Management: Monitor for increased serum concentrations of sirolimus if combined with fluconazole. Lower initial sirolimus doses or sirolimus dose reductions will likely be required. Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Grapefruit Juice: May increase the serum concentration of Sirolimus. Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Itraconazole: May increase the serum concentration of Sirolimus. Management: Sirolimus dose adjustments will likely be needed when starting/stopping any azole antifungal. Clinical data suggest sirolimus (adult) dose reductions of 50-90% will be needed when starting an azole antifungal, but specific guidelines are lacking. Consider therapy modification
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Ketoconazole (Systemic): May increase the serum concentration of Sirolimus. Management: Sirolimus dose adjustments will likely be needed when starting/stopping any azole antifungal. Clinical data suggest sirolimus (adult) dose reductions of 50-90% will be needed when starting an azole antifungal, but specific guidelines are lacking. Consider therapy modification
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Micafungin: May increase the serum concentration of Sirolimus. Monitor therapy
MiFEPRIStone: May increase the serum concentration of Sirolimus. Management: Avoid sirolimus during and 2 weeks following mifepristone for treatment of hyperglycemia in Cushing's syndrome. The interaction magnitude could be lower with single doses used to terminate pregnancy, but neither effect has been studied clinically. Avoid combination
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nelfinavir: May increase the serum concentration of Sirolimus. Management: Carefully monitor the need for sirolimus dosage reductions when coadministered with nelfinavir. Sirolimus dosage reduction will probably be needed. Consider therapy modification
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Posaconazole: May increase the serum concentration of Sirolimus. Avoid combination
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Rifabutin: May decrease the serum concentration of Sirolimus. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tacrolimus (Systemic): Sirolimus may enhance the adverse/toxic effect of Tacrolimus (Systemic). Tacrolimus (Systemic) may enhance the adverse/toxic effect of Sirolimus. Sirolimus may decrease the serum concentration of Tacrolimus (Systemic). Avoid combination
Tacrolimus (Topical): Sirolimus may enhance the adverse/toxic effect of Tacrolimus (Topical). Tacrolimus (Topical) may enhance the adverse/toxic effect of Sirolimus. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Venetoclax: May increase the serum concentration of Sirolimus. Management: Administer sirolimus at least 6 hours before venetoclax when concomitant therapy is required. Consider therapy modification
Voriconazole: May increase the serum concentration of Sirolimus. Avoid combination
Adverse Reactions
Incidence of many adverse effects is dose related. Reported events exclusive to renal transplant patients unless otherwise noted. Frequency not always defined.
Cardiovascular: Peripheral edema (≥20% to 58%, LAM and renal transplants), hypertension (49%), edema (18% to 20%), chest pain (LAM), deep vein thrombosis, pulmonary embolism, tachycardia
Central nervous system: Headache (≥20% to 34%, LAM and renal transplants), pain (29% to 33%), dizziness (LAM)
Dermatologic: Acne vulgaris (≥20% to 22%, LAM and renal transplants), skin rash (10% to 20%)
Endocrine & metabolic: Hypertriglyceridemia (45% to 57%), hypercholesterolemia (≥20% to 46%, LAM and renal transplants), amenorrhea, diabetes mellitus, hypermenorrhea, hypervolemia, hypokalemia, increased lactate dehydrogenase, menstrual disease, ovarian cyst
Gastrointestinal: Constipation (36% to 38%), abdominal pain (≥20% to 36%, LAM and renal transplants), diarrhea (≥20% to 35%, LAM and renal transplants), nausea (≥20% to 31%, LAM and renal transplants), stomatitis (3% to >20%)
Genitourinary: Urinary tract infection (33%)
Hematologic & oncologic: Anemia (23% to 33%), thrombocytopenia (14% to 30%), lymphoproliferative disorder (≤3%; including lymphoma), skin carcinoma (≤3%; includes basal cell carcinoma, squamous cell carcinoma, melanoma), hemolytic-uremic syndrome, leukopenia, lymphocele, thrombotic thrombocytopenic purpura
Infection: Herpes simplex infection, herpes zoster, sepsis
Neuromuscular & skeletal: Arthralgia (25% to 31%), myalgia (LAM), osteonecrosis
Renal: Increased serum creatinine (39% to 40%), pyelonephritis
Respiratory: Nasopharyngitis (LAM), epistaxis, pneumonia, upper respiratory tract infection (LAM)
Miscellaneous: Wound healing impairment
<3%, postmarketing, and/or case reports: Abnormal hepatic function tests, anaphylactoid reaction, anaphylaxis, angioedema, ascites, azoospermia, cardiac tamponade, cytomegalovirus, dehiscence (fascial), Epstein-Barr infection, exfoliative dermatitis, fluid retention, focal segmental glomerulosclerosis, gingival hyperplasia, hepatic necrosis, hepatotoxicity, hyperglycemia, hypersensitivity angiitis, hypersensitivity reaction, hypophosphatemia, incisional hernia, increased serum ALT, increased serum AST, increased susceptibility to infection (including opportunistic), interstitial pulmonary disease (dose related; includes pneumonitis, pulmonary fibrosis, and bronchiolitis obliterans organizing pneumonia with no identified infectious etiology), joint disorders, lymphedema, Merkel cell carcinoma, mycobacterium infection, nephrotic syndrome, neutropenia, pancreatitis, pancytopenia, pericardial effusion, pleural effusion, pneumonia due to Pneumocystis carinii, progressive multifocal leukoencephalopathy, proteinuria, pseudomembranous colitis, pulmonary alveolitis, pulmonary hemorrhage, renal disease (BK virus-associated), reversible posterior leukoencephalopathy syndrome, tuberculosis, weight loss, wound dehiscence
Warnings/Precautions
Concerns related to adverse effects:
- Anaphylactic/hypersensitivity reactions: Hypersensitivity reactions, including anaphylactic/anaphylactoid reactions, angioedema, exfoliative dermatitis, and hypersensitivity vasculitis have been reported.
- Angioedema: Has been reported; risk is increased in patients with elevated sirolimus levels and/or concurrent use with other drugs known to cause angioedema (eg, ACE inhibitors). Angioedema resolved following discontinuation or dose reduction in some cases.
- Infections: [US Boxed Warning]: Immunosuppressive agents, including sirolimus, increase the risk of infection. Immune suppression may also increase the risk of opportunistic infections including activation of latent viral infections (including BK virus-associated nephropathy), fatal infections, and sepsis. Prophylactic treatment for Pneumocystis jirovecii pneumonia (PCP) should be administered for 1 year post-transplant; prophylaxis for cytomegalovirus (CMV) should be taken for 3 months post-transplant in patients at risk for CMV. Progressive multifocal leukoencephalopathy (PML), an opportunistic CNS infection caused by reactivation of the JC virus, has been reported in patients receiving immunosuppressive therapy, including sirolimus. Clinical findings of PML include apathy, ataxia, cognitive deficiency, confusion, and hemiparesis; promptly evaluate any patient presenting with neurological changes; consider decreasing the degree of immunosuppression with consideration to the risk of organ rejection in transplant patients.
- Interstitial lung disease: Cases of interstitial lung disease (ILD) (eg, pneumonitis, bronchiolitis obliterans organizing pneumonia [BOOP], pulmonary fibrosis) have been observed (some fatal); may be associated with pulmonary hypertension (including pulmonary arterial hypertension) and risk may be increased with higher trough levels. ILD may resolve with dose reduction or discontinuation of therapy.
- Hyperlipidemia: May increase serum lipids (cholesterol and triglycerides). Use with caution in patients with hyperlipidemia. Monitor cholesterol/lipids; if hyperlipidemia occurs, follow current guidelines for management (diet, exercise, lipid lowering agents). Antihyperlipidemic therapy may not be effective in normalizing levels.
- Lymphocele/fluid accumulation: Use has been associated with an increased risk of fluid accumulation and lymphocele. Peripheral edema, lymphedema, ascites, and pleural and pericardial effusions (including significant effusions and tamponade) were reported; use with caution in patients in whom fluid accumulation may be poorly tolerated, such as in cardiovascular disease (heart failure or hypertension) and pulmonary disease.
- Malignancy: [US Boxed Warning]: Immunosuppressive agents, including sirolimus, may be associated with the development of lymphoma and other malignancies, including an increased risk of skin cancer; limit sun and ultraviolet light exposure; use appropriate sun protection.
- Proteinuria: Increased urinary protein excretion has been observed when converting renal transplant patients from calcineurin inhibitors to sirolimus during maintenance therapy. A higher level of proteinuria prior to sirolimus conversion correlates with a higher degree of proteinuria after conversion. In some patients, proteinuria may reach nephrotic levels; nephrotic syndrome (new onset) has been reported.
- Renal effects: May increase serum creatinine and decrease GFR with long-term combination use of sirolimus and cyclosporine. Immunosuppressed patients are at an increased risk of BK viral-associated nephropathy which may impair renal function and cause graft loss; consider decreasing immunosuppressive burden if evidence of deteriorating renal function. Use with caution in patients concurrently taking medications which may alter renal function.
- Wound dehiscence/healing: May be associated with wound dehiscence and impaired healing; use caution in the perioperative period. Patients with a body mass index (BMI) >30 kg/m2 are at increased risk for abnormal wound healing.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with hepatic impairment; a reduction in the maintenance dose is recommended.
Concurrent drug therapy issues:
- Calcineurin inhibitors: Concurrent use with a calcineurin inhibitor (cyclosporine, tacrolimus) may increase the risk of calcineurin inhibitor-induced hemolytic uremic syndrome/thrombotic thrombocytopenic purpura/thrombotic microangiopathy (HUS/TTP/TMA).
- Cyclosporine: Safety and efficacy of combination therapy with cyclosporine in high immunologic risk patients have not been studied beyond 12 months of treatment. Monitor renal function closely when combined with cyclosporine; consider dosage adjustment or discontinue in patients with increasing serum creatinine.
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Vaccines: Immunosuppressants may affect response to vaccination. Therefore, during treatment with sirolimus, vaccination may be less effective. The use of live vaccines should be avoided.
Special populations:
- Liver transplants: [US Boxed Warning]: Sirolimus is not recommended for use in liver transplantation; studies indicate an association with an increased risk of hepatic artery thrombosis (HAT), graft failure, and increased mortality (with evidence of infection) in these patients when sirolimus is used in combination with cyclosporine and/or tacrolimus. Most cases of HAT occurred within 30 days of transplant.
- Lung transplants: [US Boxed Warning]: Sirolimus is not recommended for use in lung transplantation. Bronchial anastomotic dehiscence cases have been reported in lung transplant patients when sirolimus was used as part of an immunosuppressive regimen; most of these reactions were fatal.
- Renal transplant: In renal transplant patients, de novo use without cyclosporine has been associated with higher rates of acute rejection. Sirolimus may delay recovery of renal function in patients with delayed allograft function.
Dosage form specific issues:
- Product interchangeability: Sirolimus tablets and oral solution are not bioequivalent, due to differences in absorption. Clinical equivalence was seen using 2 mg tablet and 2 mg solution. It is not known if higher doses are also clinically equivalent. Monitor sirolimus levels if changes in dosage forms are made.
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures, and respiratory depression; use caution (AAP 1997; Zar 2007).
Other warnings/precautions:
- Appropriate use: In renal transplant patients, sirolimus should be used in combination with cyclosporine (and corticosteroids) initially. Cyclosporine may be withdrawn in low-to-moderate immunologic risk patients after 2 to 4 months, in conjunction with an increase in sirolimus dosage. In high immunologic risk patients, use in combination with cyclosporine and corticosteroids is recommended for the first year. Adjustment of immunosuppressive therapy beyond 12 months should be considered based on clinical judgment.
- Experienced physician: [US Boxed Warning]: Should only be used by physicians experienced in immunosuppressive therapy and management of transplant patients. Adequate laboratory and supportive medical resources must be readily available.
- Laboratory monitoring: Sirolimus concentrations are dependent on the assay method (eg, chromatographic and immunoassay) used; assay methods are not interchangeable. Variations in methods to determine sirolimus whole blood concentrations, as well as interlaboratory variations, may result in improper dosage adjustments, which may lead to subtherapeutic or toxic levels. Determine the assay method used to assure consistency (or accommodations if changes occur), and for monitoring purposes, be aware of alterations to assay method or reference range and that values from different assays may not be interchangeable.
Monitoring Parameters
Monitor LFTs and CBC during treatment. Monitor sirolimus levels in all patients (especially in pediatric patients, patients ≥13 years of age weighing <40 kg, patients with hepatic impairment, or on concurrent potent inhibitors or inducers of CYP3A4 or P-gp, and/or if cyclosporine dosing is markedly reduced or discontinued), and when changing dosage forms of sirolimus. Also monitor serum cholesterol and triglycerides, blood pressure, serum creatinine, and urinary protein. Serum drug concentrations should be determined 3 to 4 days after loading doses and 7 to 14 days after dosage adjustments for renal transplant patients; however, these concentrations should not be used as the sole basis for dosage adjustment, especially during withdrawal of cyclosporine (monitor clinical signs/symptoms, tissue biopsy, and laboratory parameters). Monitor serum trough concentration 10 to 20 days after initiating therapy for lymphangioleiomyomatosis and 7 to 14 days after dosage adjustments. Once a stable dose is achieved, trough concentrations should be assessed at least every 3 months. Note: Concentrations and ranges are dependent on and will vary with assay methodology (chromatographic or immunoassay); assay methods are not interchangeable.
Pregnancy
Pregnancy Considerations
Based on the mechanism of action and data from animal reproduction studies, in utero exposure to sirolimus may cause fetal harm. Information related to the use of sirolimus in pregnancy is limited (Chu 2008; Framarino dei Malatesta 2011; Sifontis 2006).
Female patients of reproductive potential should initiate highly effective contraception before therapy with sirolimus, during treatment, and for 12 weeks after sirolimus is discontinued.
Male and female fertility may be impaired during treatment. Amenorrhea and menorrhagia have been reported in females; azoospermia (which may be reversible) has been reported in males.
The Transplant Pregnancy Registry International (TPR) is a registry that follows pregnancies that occur in maternal transplant recipients or those fathered by male transplant recipients. The TPR encourages reporting of pregnancies following solid organ transplant by contacting them at 1-877-955-6877 or https://www.transplantpregnancyregistry.org.
Patient Education
What is this drug used for?
- It is used after a kidney transplant to keep the body from rejecting the kidney.
- It is used to treat a lung disease called lymphangioleiomyomatosis (LAM).
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Abdominal pain
- Constipation
- Diarrhea
- Nausea
- Stuffy nose
- Sore throat
- Acne
- Joint pain
- Mouth irritation
- Mouth sores
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes
- Infection
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Low potassium like muscle pain or weakness, muscle cramps, or an abnormal heartbeat
- Blood clots like numbness or weakness on one side of the body; pain, redness, tenderness, warmth, or swelling in the arms or legs; change in color of an arm or leg; chest pain; shortness of breath; fast heartbeat; or coughing up blood
- Swollen glands
- Excessive weight loss
- Severe dizziness
- Passing out
- Vision changes
- Fast heartbeat
- Night sweats
- Severe headache
- Skin growths
- Mole changes
- Severe loss of strength and energy
- Trouble with wound healing
- Bruising
- Bleeding
- Swelling of arms or legs
- Menstrual changes
- Severe pulmonary disorder like lung or breathing problems like difficulty breathing, shortness of breath, or a cough that is new or worse
- Progressive multifocal leukoencephalopathy like confusion, depression, trouble with memory, behavioral changes, change in strength on one side is greater than the other, difficulty speaking, change in balance, or vision changes
- Thrombotic thrombocytopenic purpura/hemolytic uremic syndrome like bruising or bleeding; loss of strength and energy; dark urine or yellow skin or eyes; pale skin; change in amount of urine passed; vision changes; change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance; or fever
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.