Boxed Warning
Life threatening proarrhythmia:
To minimize the risk of drug-induced arrhythmia, initiate or reinitiate sotalol in a facility that can provide cardiac resuscitation and continuous electrocardiographic (ECG) monitoring. Sotalol can cause life threatening ventricular tachycardia associated with QT interval prolongation. Do not initiate sotalol therapy if the baseline QTc is longer than 450 msec. If the QT interval prolongs to 500 msec or greater, reduce the dose, lengthen the dosing interval, or discontinue the drug. Calculate creatinine clearance to determine appropriate dosing.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Intravenous, as hydrochloride:
Generic: 150 mg/10 mL (10 mL)
Solution, Oral, as hydrochloride:
Sotylize: 5 mg/mL (250 mL, 480 mL) [contains sodium benzoate; grape flavor]
Tablet, Oral, as hydrochloride:
Betapace: 80 mg, 120 mg, 160 mg [scored; contains fd&c blue #2 aluminum lake]
Betapace AF: 80 mg, 120 mg, 160 mg [scored]
Sorine: 80 mg, 120 mg, 160 mg, 240 mg [scored]
Generic: 80 mg, 120 mg, 160 mg, 240 mg
Pharmacology
Mechanism of Action
Beta-blocker which contains both beta-adrenoreceptor-blocking (Vaughan Williams Class II) and cardiac action potential duration prolongation (Vaughan Williams Class III) properties
Class II effects: Increased sinus cycle length, slowed heart rate, decreased AV nodal conduction, and increased AV nodal refractoriness Sotalol has both beta1- and beta2-receptor blocking activity. The beta-blocking effect of sotalol is a noncardioselective (half maximal at about 80 mg/day and maximal at doses of 320 to 640 mg/day). Significant beta-blockade occurs at oral doses as low as 25 mg/day.
Class III effects: Prolongation of the atrial and ventricular monophasic action potentials, and effective refractory prolongation of atrial muscle, ventricular muscle, and atrioventricular accessory pathways in both the antegrade and retrograde directions. Sotalol is a racemic mixture of d- and l-sotalol; both isomers have similar Class III antiarrhythmic effects while the l-isomer is responsible for virtually all of the beta-blocking activity. The Class III effects are seen only at oral doses ≥160 mg/day.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Well absorbed (Hanyok 1993); decreased ~20% by meals compared with fasting
Distribution
Vd: 1.2 to 2.4 L/kg (Hanyok 1993)
Metabolism
None
Excretion
Urine (as unchanged drug)
Clearance (apparent) (Saul 2001b):
Neonates ≤1 month: 11 mL/minute
Infants and Children >1 month to 24 months: 32 mL/minute
Children >2 years to <7 years: 63 mL/minute
Children 7 to 12 years: 95 mL/minute
Onset of Action
Oral: Rapid; at 1 to 2 hours post dosing (steady-state), reductions in heart rate and cardiac index seen (Winters 1993)
IV: When administered IV over 5 minutes for ongoing VT, onset of action is ~5 to 10 minutes (Ho 1994)
Time to Peak
Serum: Oral: Infants and Children 3 days to 12 years: Mean range: 2 to 3 hours; Adults: 2.5 to 4 hours
Half-Life Elimination
Oral:
Neonates ≤1 month: 8.4 hours (Saul 2001b)
Infants and Children >1 month to 24 months: 7.4 hours (Saul 2001b)
Children >2 years to <7 years: 9.1 hours (Saul 2001b)
Children 7 to 12 years: 9.2 hours (Saul 2001b)
Adults: 12 hours
Adults with renal failure (anuric): Up to 69 hours
IV: Pharmacokinetics of the IV formulation (administered over 5 hours) are similar to the oral formulations (Somberg 2010).
Protein Binding
None
Use in Specific Populations
Special Populations: Renal Function Impairment
Terminal half-life increases with renal impairment.
Use: Labeled Indications
Atrial fibrillation/flutter (symptomatic): Maintenance of normal sinus rhythm (delay in time to recurrence of atrial fibrillation/atrial flutter) in patients with symptomatic atrial fibrillation/atrial flutter who are currently in sinus rhythm.
According to the American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS), sotalol is not effective for conversion of atrial fibrillation to sinus rhythm but may be used to prevent atrial fibrillation (AHA/ACC/HRS [January 2014])
Ventricular arrhythmias: Treatment of documented, life-threatening ventricular arrhythmias (ie, sustained ventricular tachycardia)
Use: Off Label
Atrial fibrillation in patients with hypertrophic cardiomyopathy (HCM) (alternative antiarrhythmic)yes
Based on the 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy and the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation (AF), sotalol given as an alternative antiarrhythmic for AF in patients with hypertrophic cardiomyopathy (HCM) is effective and recommended in the management of this condition.
Fetal tachycardia, sustainedcyes
Data from retrospective studies of fetuses with tachycardia with or without hydrops suggest that sotalol via maternal administration may be beneficial for the treatment of fetal tachycardia Alsaied 2017, Hill 2017, Jaeggi 2011, Oudijk 2000, Shah 2012, Sonesson 1998, van der Heijden 2013.
Based on the American Heart Association scientific statement for the diagnosis and treatment of fetal cardiac disease, sotalol may be considered for the in utero management of fetal supraventricular tachycardia (SVT) or atrial flutter with hydrops or ventricular dysfunction. Sotalol may also be considered for SVT without hydrops or ventricular dysfunction if heart rate is ≥200 bpm, atrial flutter, or other rare tachycardias with an average heart rate of ≥200 bpm. In addition, sotalol may be considered for management of fetal ventricular tachycardia (VT) with normal QTc with or without hydrops but is contraindicated for the treatment of fetal VT when long QT syndrome is suspected or confirmed AHA [Donofrio 2014].
Monomorphic ventricular tachycardia (hemodynamically stable)cyes
Data from one randomized double-blind study in a limited number of patients comparing the effectiveness of IV sotalol to IV lidocaine for the treatment of sustained hemodynamically stable ventricular tachycardia (VT) suggest that IV sotalol may be beneficial for the treatment of this condition Ho 1994. Additional data from an open-label electrophysiology study evaluating the effects of IV sotalol as a 1-minute or a 5-minute infusion on the right ventricular effective refractory period in patients with induced sustained VT safely demonstrated a rapid onset of the electrophysiological effects Ho 1995. Additional trials may be necessary to further define the role of IV sotalol in the treatment of this condition.
Based on the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, IV sotalol may be used to treat ongoing hemodynamically stable monomorphic VT.
Supraventricular tachycardiayes
Based on the American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines for the management of patients with supraventricular arrhythmias, sotalol may be a reasonable treatment for a variety of symptomatic supraventricular tachycardias (atrioventricular nodal reentrant tachycardia [AVNRT], atrioventricular reentrant tachycardia [AVRT], and focal atrial tachycardia [AT]) in patients who are not candidates for, or prefer not to undergo catheter ablation and in whom other therapies have failed or are contraindicated. Oral sotalol may be useful for the acute treatment or ongoing management of hemodynamically stable patients with adult congenital heart disease and recurrent atrial flutter or focal atrial tachycardia.
Ventricular premature beatsyes
Based on the American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death, oral sotalol is effective for suppressing premature ventricular contractions. Clinical experts recommend beta blockers other than sotalol as first line pharmacologic therapy due to a safer side effect profile Manolis 2018.
Contraindications
Hypersensitivity to sotalol or any component of the formulation; bronchial asthma or related bronchospastic conditions; sinus bradycardia (<50 bpm during waking hours); second- or third-degree AV block (unless a functioning pacemaker is present); congenital or acquired long QT syndromes; cardiogenic shock; uncontrolled heart failure; sick sinus syndrome; serum potassium <4 mEq/L; when used for atrial fibrillation/flutter sotalol is also contraindicated if baseline QTc interval >450 msec or CrCl <40 mL/minute
Documentation of allergenic cross-reactivity for beta-adrenergic blockers is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Baseline QTc interval and creatinine clearance must be determined prior to initiation. If CrCl ≤60 mL/minute, dosing interval adjustment is necessary. Sotalol should be initiated and doses increased in a hospital for at least 3 days with facilities for cardiac rhythm monitoring and assessment. Proarrhythmic events can occur after initiation of therapy and with each upward dosage adjustment.
Atrial fibrillation/flutter (symptomatic):
IV: Substitution for oral sotalol: Note: The effects of the initial IV dose must be monitored and the dose titrated either upward or downward, if needed, based on clinical effect, QTc interval, or adverse reactions.
Initial dose: 75 mg infused over 5 hours twice daily
Dose adjustment: If the initial dose does not reduce the frequency of relapse and excessive QTc prolongation does not occur (eg, QTc < 500 msec), may increase dosage after at least 3 days to 112.5 mg twice daily. If at steady state this dose still does not control arrhythmia and QTc prolongation does not occur may further increase dose to 150 mg twice daily.
Dose range: Usual therapeutic dose: 112.5 mg twice daily; maximum dose: 150 mg twice daily
Oral: Initial: 80 mg twice daily. If the initial dose does not reduce frequency of relapse and excessive QTc prolongation does not occur (eg, QTc <500 msec) after 3 days, the dose may be increased to 120 mg twice daily; may further increase to a maximum dose of 160 mg twice daily if response is inadequate and QTc prolongation is not excessive.
Fetal tachycardia, sustained (maternal/transplacental administration) (off-label use): Oral: Initial: 80 to 160 mg twice daily; may increase dose as needed up to 480 mg/day in divided doses based on response and tolerability (Alsaied 2017; Jaeggi 2011; Oudijk 2000; Sonesson 1998; van der Heijden 2013).
Ventricular arrhythmias:
IV: Substitution for oral sotalol: Note: The effects of the initial IV dose must be monitored and the dose titrated either upward or downward, if needed, based on clinical effect, QTc interval, or adverse reactions.
Initial dose: 75 mg infused over 5 hours twice daily
Dose adjustment: If the initial dose does not reduce the frequency of relapse and excessive QTc prolongation does not occur (eg, QTc <500 msec); may increase dosage after at least 3 days to 112.5 mg twice daily. May further increase dose in 3 days by 75 mg/day; maximum dose: 300 mg twice daily
Dose range: Usual therapeutic dose: 75 to 150 mg twice daily
Oral:
Initial dose: 80 mg twice daily; dose may be increased gradually (in increments of 80 mg/day) if excessive QTc prolongation does not occur (eg, QTc <500 msec) to 160 to 320 mg/day in 2 divided doses; allow 3 days between dosing increments in order to attain steady-state plasma concentrations and to allow for monitoring of QT intervals (AHA/ACC/HRS [Al-Khatib 2017])
Maximum dose: Some patients, with life-threatening refractory ventricular arrhythmias, may require total daily doses as high as 480 to 640 mg; however, these doses should only be prescribed when the potential benefit outweighs the increased risk of adverse events.
Monomorphic VT (hemodynamically stable) (off-label use): IV: 1.5 mg/kg over 5 minutes (AHA [Neumar 2010]); Note: Clinical trial employed standard dose of 100 mg (Ho 1994).
Ventricular premature beats (off-label use): Oral: Initial: 80 mg twice daily; dose may be increased gradually (in increments of 80 mg/day) to 160 to 320 mg/day in 2 divided doses; maximum dose: 320 mg/day; allow 3 days between dosing increments in order to attain steady-state plasma concentrations and to allow for monitoring of QT intervals (AHA/ACC/HRS [Al-Khatib 2017])
Supraventricular tachycardia (off-label use): Oral: Initial: 40 to 80 mg every 12 hours; maximum maintenance dose: 160 mg every 12 hours (ACC/AHA/HRS [Page 2015])
Conversion from oral sotalol to IV sotalol:
80 mg oral equivalent to 75 mg IV
120 mg oral equivalent to 112.5 mg IV
160 mg oral equivalent to 150 mg IV
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Baseline QTc interval and CrCl must be determined prior to initiation. Dosage must be adjusted to individual response and tolerance; doses should be initiated or increased in a hospital facility that can provide continuous ECG monitoring, recognition and treatment of life-threatening arrhythmias, and CPR:
In pediatric patients, dosing may be based on either BSA (mg/m2) or weight (mg/kg); use extra precaution to verify dosing parameters during calculations. Sotalol is indicated for both the treatment of documented life-threatening ventricular arrhythmias (marketed as Betapace/Sorine/Sotylize) and for the maintenance of normal sinus rhythm in patients with symptomatic atrial fibrillation/flutter who are currently in sinus rhythm (marketed as Betapace AF/Sotylize).
Arrhythmias: Oral: Manufacturer's dosing recommendations are based on doses per m2 (that are equivalent to the doses recommended in adults) and on pediatric pharmacokinetic and pharmacodynamic studies (Saul 2001a; Saul 2001b). BSA, rather than body weight, better predicted apparent clearance of sotalol; however, for a given dose per m2, a larger drug exposure (larger AUC) and greater pharmacologic effects were observed in smaller subjects (ie, those with BSA <0.33 m2 versus those with BSA ≥0.33 m2). For infants and children ≤2 years of age, the manufacturer recommends a dosage reduction based on an age factor determined from a graph (see below).
Manufacturer's labeling: Note: Use with extreme caution if QTc is >500 msec while receiving sotalol; reduce the dose or discontinue drug if QTc >550 msec.
Infants and Children ≤2 years: The manufacturer recommended pediatric dosage of 30 mg/m2/dose every 8 hours must be REDUCED using an age-related factor that is obtained from the graph (see graph). First, obtain the patient's age in months; use the graph to determine where the patient's age (on the logarithmic scale) intersects the age factor curve; read the age factor from the Y-axis; then multiply the age factor by the pediatric dose listed below (ie, the dose for children >2 years); this will result in the proper reduction in dose for age. For example, the age factor for an infant 1 month of age is 0.68, so the initial dosage would be (0.68 x 30 mg/m2/dose) = 20 mg/m2/dose given every 8 hours. Similar calculations should be made for dosage titrations; increase dosage gradually, if needed; allow adequate time between dosage increments to achieve new steady-state and to monitor clinical response, heart rate and QTc intervals; half-life is prolonged with decreasing age (<2 years), so time to reach new steady-state will increase.
Children >2 years and Adolescents: Initial: 30 mg/m2/dose given every 8 hours; increase dosage gradually if needed; allow at least 36 hours between dosage increments to achieve new steady-state and to monitor clinical response, heart rate, and QTc intervals; may increase gradually to a maximum of 60 mg/m2/dose given every 8 hours; not to exceed adult doses (usual maximum adult daily dose: 320 mg/day)
Alternate dosing: Limited data available:
Initial: Infants, Children, and Adolescents: 2 mg/kg/day divided every 8 hours; if needed, increase dosage gradually by 1 to 2 mg/kg/day increments; allow 3 days between dosage increments to achieve new steady-state and to monitor clinical response, heart rate, and QTc intervals; maximum: 10 mg/kg/day (if no limiting side effects occur) (Beaufort-Krol 1997; Colloridi 1992; Läer 2005; Maragnes 1992; Pfammatter 1995; Pfammatter 1997; Tipple 1991); do not exceed adult doses (usual maximum adult daily dose: 320 mg/day)
Proposed target doses: Note: It is not necessary to increase to target dosage if desired clinical effect has been achieved at a lower dosage.
Infants and Children 1 month to 6 years: 6 mg/kg/day divided every 8 hours
Children >6 years and Adolescents: 4 mg/kg/day divided every 8 hours not to exceed adult doses (usual maximum adult daily dose: 320 mg/day)
Dosing adjustment for toxicity: Infants, Children, and Adolescents:
QTc ≥500 msec during initiation period (Betapace AF, Sotylize): Reduce dose, prolong the dosing interval (Sotylize), or discontinue sotalol.
QTc ≥520 msec (or JT interval ≥430 msec if the QRS >100 msec) during maintenance therapy (Betapace AF): Reduce dose and carefully monitor QTc until <520 msec. If QTc interval ≥520 msec on the lowest maintenance dose, discontinue sotalol.
QTc ≥550 msec (Betapace, Sorine): Reduce dose or discontinue sotalol.
Dosing: Adjustment for Toxicity
QTc ≥500 msec:
Tablets, oral solution: Reduce dose, prolong the dosing interval, or discontinue sotalol
Injection: Reduce dose, prolong the infusion time by decreasing the infusion rate, or discontinue sotalol
Reconstitution
To prepare sotalol infusion, see manufacturer's prescribing information. Usually prepared in a volume of 100 to 250 mL; appropriate diluents are NS, D5W, or LR.
Extemporaneously Prepared
Note: Commercial oral solution is available (5 mg/mL)
A 5 mg/mL sotalol syrup may be made with Betapace, Sorine, or Betapace AF tablets and Simple Syrup containing sodium benzoate 0.1% (Syrup, NF). Place 120 mL Syrup, NF in a 6-ounce amber plastic (polyethylene terephthalate) prescription bottle; add five Betapace, Sorine, or Betapace AF 120 mg tablets and shake the bottle to wet the tablets. Allow tablets to hydrate for at least 2 hours, then shake intermittently over ≥2 hours until the tablets are completely disintegrated; a dispersion of fine particles (water-insoluble inactive ingredients) in syrup should be obtained. Note: To simplify the disintegration process, tablets can hydrate overnight; tablets may also be crushed, carefully transferred into the bottle and shaken well until a dispersion of fine particles in syrup is obtained. Label "shake well". Stable for 3 months at 15°C to 30°C (59°F to 86°F) and ambient humidity.
Betapace/Betapace AF prescribing information, Zug, Switzerland: Covis Pharmaceuticals; May 2016.Sorine prescribing information, Upsher-Smith, Minneapolis, MN, 2012.
Administration
Oral: Administer without regard to meals.
When used for the management of fetal tachycardia (maternal/transplacental administration; off-label use), oral doses are administered to the mother.
IV:
Substitution for oral: Administer over 5 hours; may prolong duration of infusion if QT interval prolongs to ≥500 msec.
Hemodynamically stable monomorphic VT: Administer IV push over 5 minutes; use with caution because of increased risk of adverse events (eg, bradycardia, hypotension, torsade de pointes) (ACLS 2010).
Storage
Store at 25°C (77°F); excursions permitted between 15°C and 30°C (59°F and 86°F). Protect injection from freezing and light.
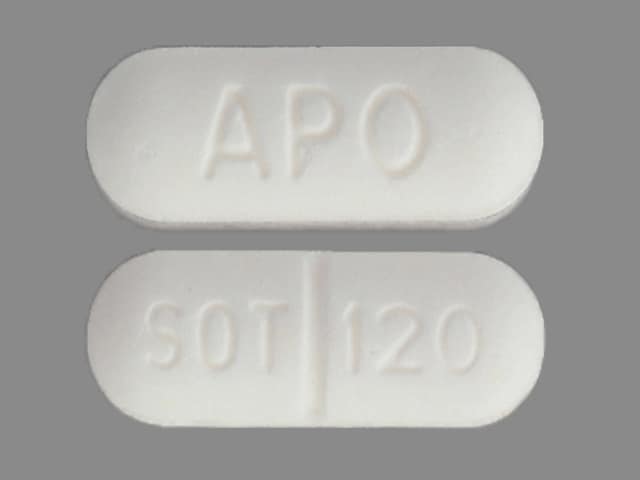
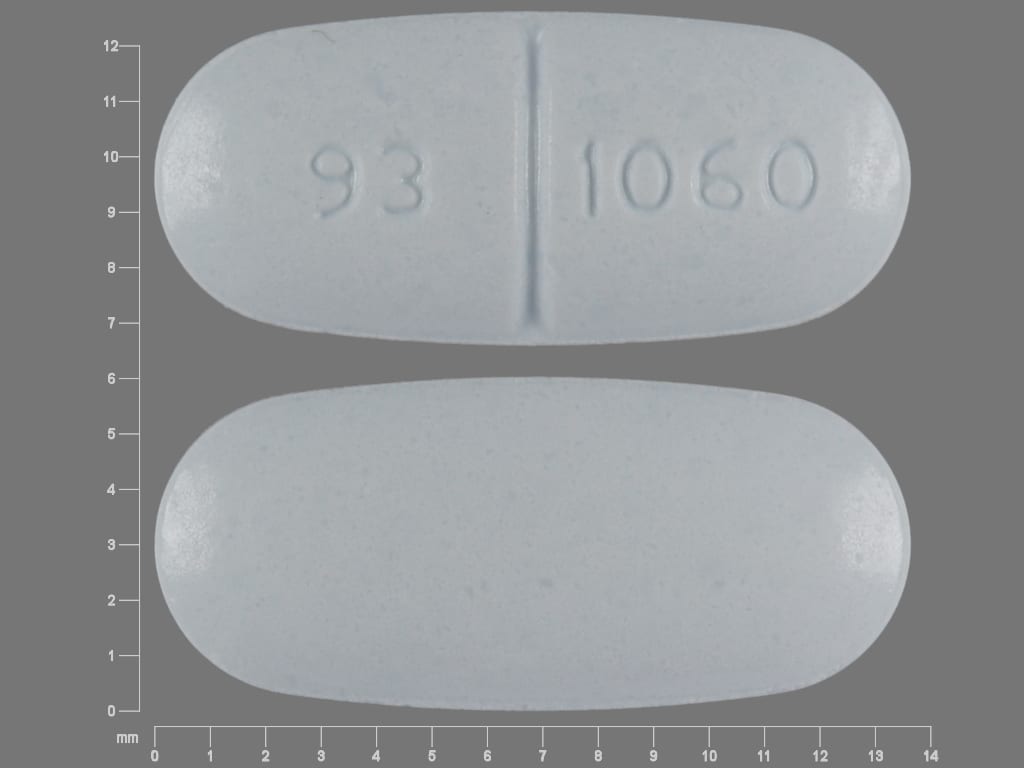
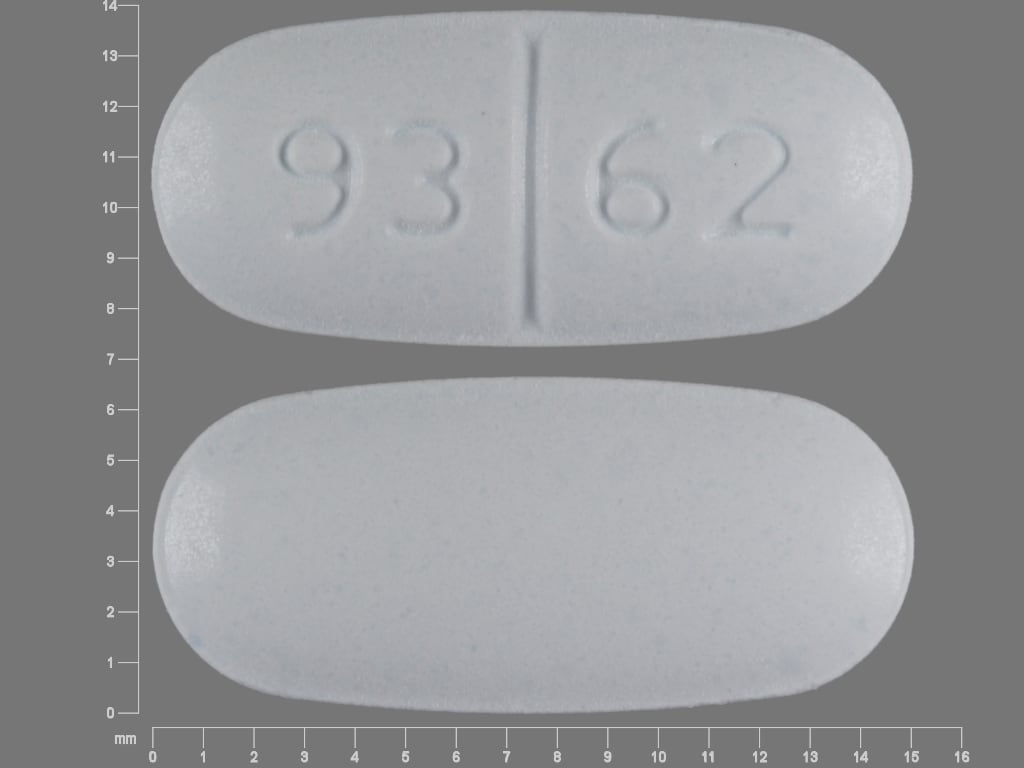
Sotalol Images
Drug Interactions
Acetylcholinesterase Inhibitors: May enhance the bradycardic effect of Beta-Blockers. Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alpha1-Blockers: Beta-Blockers may enhance the orthostatic hypotensive effect of Alpha1-Blockers. The risk associated with ophthalmic products is probably less than systemic products. Monitor therapy
Alpha2-Agonists: May enhance the AV-blocking effect of Beta-Blockers. Sinus node dysfunction may also be enhanced. Beta-Blockers may enhance the rebound hypertensive effect of Alpha2-Agonists. This effect can occur when the Alpha2-Agonist is abruptly withdrawn. Management: Closely monitor heart rate during treatment with a beta blocker and clonidine. Withdraw beta blockers several days before clonidine withdrawal when possible, and monitor blood pressure closely. Recommendations for other alpha2-agonists are unavailable. Exceptions: Apraclonidine. Consider therapy modification
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amiodarone: QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Amiodarone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Amisulpride: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Amisulpride. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Antacids: May decrease the serum concentration of Sotalol. Management: Avoid simultaneous administration of sotalol and antacids. Administer antacids 2 hours after sotalol. Consider therapy modification
Antipsychotic Agents (Phenothiazines): May enhance the hypotensive effect of Beta-Blockers. Beta-Blockers may decrease the metabolism of Antipsychotic Agents (Phenothiazines). Antipsychotic Agents (Phenothiazines) may decrease the metabolism of Beta-Blockers. Monitor therapy
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Azithromycin (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Azithromycin (Systemic). Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Barbiturates: May decrease the serum concentration of Beta-Blockers. Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Beta2-Agonists: Beta-Blockers (Nonselective) may diminish the bronchodilatory effect of Beta2-Agonists. Avoid combination
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Bradycardia-Causing Agents: May enhance the bradycardic effect of other Bradycardia-Causing Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Bupivacaine: Beta-Blockers may increase the serum concentration of Bupivacaine. Monitor therapy
Calcium Channel Blockers (Nondihydropyridine): May enhance the hypotensive effect of Beta-Blockers. Bradycardia and signs of heart failure have also been reported. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Beta-Blockers. Exceptions: Bepridil. Monitor therapy
Cardiac Glycosides: Beta-Blockers may enhance the bradycardic effect of Cardiac Glycosides. Monitor therapy
Ceritinib: May enhance the bradycardic effect of Sotalol. Ceritinib may enhance the QTc-prolonging effect of Sotalol. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Chloroquine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Chloroquine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Cholinergic Agonists: Beta-Blockers may enhance the adverse/toxic effect of Cholinergic Agonists. Of particular concern are the potential for cardiac conduction abnormalities and bronchoconstriction. Monitor therapy
Citalopram: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Citalopram. Avoid combination
Clarithromycin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Clarithromycin. Avoid combination
Clofazimine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Clofazimine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
CloZAPine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of CloZAPine. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Dasatinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Dasatinib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dipyridamole: May enhance the bradycardic effect of Beta-Blockers. Monitor therapy
Domperidone: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Domperidone. Avoid combination
Doxepin-Containing Products: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Doxepin-Containing Products. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Droperidol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Droperidol. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Encorafenib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Entrectinib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Avoid combination
EPINEPHrine (Nasal): Beta-Blockers (Nonselective) may enhance the hypertensive effect of EPINEPHrine (Nasal). Monitor therapy
EPINEPHrine (Oral Inhalation): Beta-Blockers (Nonselective) may enhance the hypertensive effect of EPINEPHrine (Oral Inhalation). Monitor therapy
Epinephrine (Racemic): Beta-Blockers (Nonselective) may enhance the hypertensive effect of Epinephrine (Racemic). Monitor therapy
EPINEPHrine (Systemic): Beta-Blockers (Nonselective) may enhance the hypertensive effect of EPINEPHrine (Systemic). Monitor therapy
Ergot Derivatives: Beta-Blockers may enhance the vasoconstricting effect of Ergot Derivatives. Exceptions: Nicergoline. Consider therapy modification
Erythromycin (Systemic): QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Erythromycin (Systemic). Erythromycin (Systemic) may enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Management: Avoid concomitant use of erythromycin and class III antiarrhythmic agents. Use of erythromycin with dronedarone is specifically contraindicated. Avoid combination
Escitalopram: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Escitalopram. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Avoid combination
Fexinidazole [INT]: Bradycardia-Causing Agents may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Fingolimod: May enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Avoid combination
Flecainide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Flecainide. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Floctafenine: May enhance the adverse/toxic effect of Beta-Blockers. Avoid combination
Flupentixol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Flupentixol. Avoid combination
Gadobenate Dimeglumine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Gadobenate Dimeglumine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Gemifloxacin: May enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Avoid combination
Gilteritinib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Consider alternatives to this combination. If use is necessary, monitor for QTc interval prolongation and arrhythmias. Consider therapy modification
Grass Pollen Allergen Extract (5 Grass Extract): Beta-Blockers may enhance the adverse/toxic effect of Grass Pollen Allergen Extract (5 Grass Extract). More specifically, Beta-Blockers may inhibit the ability to effectively treat severe allergic reactions to Grass Pollen Allergen Extract (5 Grass Extract) with epinephrine. Some other effects of epinephrine may be unaffected or even enhanced (e.g., vasoconstriction) during treatment with Beta-Blockers. Consider therapy modification
Halofantrine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Halofantrine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Haloperidol: QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Inotuzumab Ozogamicin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Inotuzumab Ozogamicin. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Insulins: Beta-Blockers may enhance the hypoglycemic effect of Insulins. Monitor therapy
Ivabradine: Bradycardia-Causing Agents may enhance the bradycardic effect of Ivabradine. Monitor therapy
Lacosamide: Bradycardia-Causing Agents may enhance the AV-blocking effect of Lacosamide. Monitor therapy
Lacosamide: Antiarrhythmic Agents (Class III) may enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Levofloxacin-Containing Products (Systemic): May enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Avoid combination
Lidocaine (Systemic): Beta-Blockers may increase the serum concentration of Lidocaine (Systemic). Monitor therapy
Lidocaine (Topical): Beta-Blockers may increase the serum concentration of Lidocaine (Topical). Monitor therapy
Lidocaine (Topical): May enhance the arrhythmogenic effect of Antiarrhythmic Agents (Class III). Antiarrhythmic Agents (Class III) may increase the serum concentration of Lidocaine (Topical). This mechanism specifically applies to amiodarone and dronedarone. Monitor therapy
Lofexidine: May enhance the QTc-prolonging effect of Sotalol. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Mepivacaine: Beta-Blockers may increase the serum concentration of Mepivacaine. Monitor therapy
Methacholine: Beta-Blockers may enhance the adverse/toxic effect of Methacholine. Monitor therapy
Methadone: QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Methadone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Methoxyflurane: May enhance the hypotensive effect of Beta-Blockers. Monitor therapy
Midodrine: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Midostaurin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Midostaurin. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Moxifloxacin (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Moxifloxacin (Systemic). Avoid combination
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
NIFEdipine: May enhance the hypotensive effect of Beta-Blockers. NIFEdipine may enhance the negative inotropic effect of Beta-Blockers. Monitor therapy
Nilotinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Nilotinib. Avoid combination
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May diminish the antihypertensive effect of Beta-Blockers. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
OLANZapine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of OLANZapine. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Ondansetron: QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Ondansetron. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Opioids (Anilidopiperidine): May enhance the bradycardic effect of Beta-Blockers. Opioids (Anilidopiperidine) may enhance the hypotensive effect of Beta-Blockers. Monitor therapy
Osimertinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Osimertinib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Pentamidine (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pentamidine (Systemic). Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pilsicainide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pilsicainide. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Pimozide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pimozide. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Avoid combination
Piperaquine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Piperaquine. Avoid combination
Probucol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Probucol. Avoid combination
Propafenone: May enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
QT-prolonging Agents (Indeterminate Risk - Avoid): May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Agents (Indeterminate Risk - Caution): May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Class IA Antiarrhythmics (Highest Risk): May enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Avoid combination
QT-prolonging Class III Antiarrhythmics (Highest Risk): May enhance the QTc-prolonging effect of other QT-prolonging Class III Antiarrhythmics (Highest Risk). Avoid combination
QT-prolonging Kinase Inhibitors (Highest Risk): May enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Miscellaneous Agents (Highest Risk): QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Class III Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Erythromycin (Systemic); Nilotinib; Ribociclib. Consider therapy modification
QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk): QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Class III Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Ceritinib; Clarithromycin. Consider therapy modification
QUEtiapine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of QUEtiapine. Avoid combination
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Regorafenib: May enhance the bradycardic effect of Beta-Blockers. Monitor therapy
Reserpine: May enhance the hypotensive effect of Beta-Blockers. Monitor therapy
Ribociclib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Ribociclib. Avoid combination
Rifamycin Derivatives: May decrease the serum concentration of Beta-Blockers. Exceptions: Rifabutin. Monitor therapy
RisperiDONE: QT-prolonging Agents (Highest Risk) may enhance the CNS depressant effect of RisperiDONE. QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of RisperiDONE. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Rivastigmine: May enhance the bradycardic effect of Beta-Blockers. Avoid combination
Ruxolitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Management: Ruxolitinib Canadian product labeling recommends avoiding use with bradycardia-causing agents to the extent possible. Monitor therapy
Siponimod: Bradycardia-Causing Agents may enhance the bradycardic effect of Siponimod. Management: Avoid coadministration of siponimod with drugs that may cause bradycardia. Consider therapy modification
Sodium Stibogluconate: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Sodium Stibogluconate. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Sparfloxacin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Sparfloxacin. Avoid combination
Sulfonylureas: Beta-Blockers may enhance the hypoglycemic effect of Sulfonylureas. Cardioselective beta-blockers (eg, acebutolol, atenolol, metoprolol, and penbutolol) may be safer than nonselective beta-blockers. All beta-blockers appear to mask tachycardia as an initial symptom of hypoglycemia. Ophthalmic beta-blockers are probably associated with lower risk than systemic agents. Monitor therapy
Terlipressin: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Theophylline Derivatives: Beta-Blockers (Nonselective) may diminish the bronchodilatory effect of Theophylline Derivatives. Monitor therapy
Thioridazine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Thioridazine. Avoid combination
Tofacitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Vemurafenib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Vemurafenib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Test Interactions
May falsely increase urinary metanephrine values when fluorimetric or photometric methods are used; does not interact with HPLC assay with solid phase extraction for determination of urinary catecholamines; may lead to false-positive aldosterone/renin ratio (ARR) (Funder 2016)
Adverse Reactions
There is minimal clinical experience with IV sotalol; however, since exposure is similar between IV and oral sotalol, adverse reactions are expected to be similar.
>10%:
Cardiovascular: Bradycardia (dose related; 8% to 16%), chest pain (3% to 16%), palpitations (3% to 14%)
Central nervous system: Fatigue (dose related; 5% to 20%), dizziness (3% to 20%), headache (2% to 12%)
Neuromuscular & skeletal: Weakness (4% to 13%)
Respiratory: Dyspnea (dose related; 5% to 21%)
1% to 10%:
Cardiovascular: Edema (2% to 8%), ECG abnormality (2% to 7%), hypotension (3% to 6%), cardiac failure (1% to 5%; incidence may be higher in patients with risk factors), syncope (1% to 5%), proarrhythmia (<1% to 5%), torsades de pointes (dose related; 1% to 4%), peripheral vascular disorder (1% to 3%), angina pectoris (2%), presyncope (1% to 2%), cardiovascular signs and symptoms (<1% to 2%), worsened ventricular tachycardia (1%), cerebrovascular accident (≤1%), hypertension (≤1%), vasodilation (≤1%), prolonged Q-T interval on ECG (dose related)
Central nervous system: Sleep disorder (1% to 8%), insomnia (3% to 4%), anxiety (2% to 4%), depression (1% to 4%), paresthesia (1% to 4%), sensation of cold (2% to 3%), impaired consciousness (1% to 3%), mood changes (≤1%)
Dermatologic: Hyperhidrosis (5%), skin rash (2% to 5%), diaphoresis (1% to 3%)
Endocrine & metabolic: Weight changes (1%)
Gastrointestinal: Nausea and vomiting (4% to 10%), diarrhea (2% to 7%), abdominal pain (<1% to 4%), dyspepsia (2% to 3%), abdominal distention (<1% to 3%), decreased appetite (2%), change in appetite (1% to 2%), colonic disease (1% to 2%), flatulence (<1% to 2%)
Genitourinary: Sexual disorder (≤3%), genitourinary complaint (≤1%)
Hematologic & oncologic: Hemorrhage (<1% to 2%)
Infection: Infection (1% to 2%), influenza (1% to 2%)
Local: Local pain (1% to 2%)
Neuromuscular & skeletal: Limb pain (2% to 7%), musculoskeletal pain (3% to 4%), musculoskeletal chest pain (2% to 3%), back pain (<1% to 3%)
Ophthalmic: Visual disturbance (1% to 5%)
Respiratory: Upper respiratory complaint (1% to 8%), pulmonary disease (3% to 5%), tracheobronchitis (1% to 3%), asthma (<1% to 2%)
Miscellaneous: Fever (1% to 3%), laboratory test abnormality (1% to 3%), AICD discharge (<1% to 2%)
<1%, postmarketing and/or case reports: Alopecia, clouding of consciousness, emotional lability, eosinophilia, hyperlipidemia, incoordination, increased liver enzymes, leukopenia, myalgia, paralysis, skin photosensitivity, pruritus, pulmonary edema, thrombocytopenia, vertigo
Warnings/Precautions
Concerns related to adverse effects:
- Anaphylactic reactions: Use caution with history of severe anaphylaxis to allergens; patients taking beta-blockers may become more sensitive to repeated challenges. Treatment of anaphylaxis (eg, epinephrine) in patients taking beta-blockers may be ineffective or promote undesirable effects.
- Bradycardia/hypotension: May cause bradycardia (including heart block) and hypotension. Dose adjustments of agents that slow AV nodal conduction may be necessary when sotalol is initiated.
- Proarrhythmic effects: [US Boxed Warning]: To minimize the risk of drug-induced arrhythmia, initiate or reinitiate sotalol in a facility that can provide cardiac resuscitation and continuous electrocardiographic (ECG) monitoring. Sotalol can cause life threatening ventricular tachycardia associated with QT interval prolongation. Do not initiate sotalol therapy if the baseline QTc is longer than 450 msec. If the QT interval prolongs to 500 msec or greater, reduce the dose, lengthen the dosing interval, or discontinue the drug.Calculate creatinine clearance to determine appropriate dosing. Some experts will initiate oral therapy on an outpatient basis if the patient is in sinus rhythm provided the QT interval and serum potassium are normal and the patient is not receiving any other QT-interval prolonging medications but require inpatient hospitalization if the patient is in atrial fibrillation (AHA/ACC/HRS [January 2014]). Calculation of CrCl must occur prior to administration of the first dose. Dosage should be adjusted gradually with 3 days between dosing increments to achieve steady-state concentrations, and to allow time to monitor QT intervals. Monitor and adjust dose to prevent QTc prolongation.
Disease-related concerns:
- Bronchospastic disease: In general, patients with bronchospastic disease should not receive beta-blockers; if used at all, should be used cautiously with close monitoring. Sotalol is contraindicated in patients with bronchial asthma or related bronchospastic conditions.
- Conduction abnormality: Consider preexisting conditions such as sick sinus syndrome before initiating.
- Diabetes: Use with caution in patients with diabetes mellitus; may potentiate hypoglycemia and/or mask signs and symptoms.
- Electrolyte imbalances: Correct electrolyte imbalances before initiating (especially hypokalemia and hypomagnesemia) because these conditions increase the risk of torsades de pointes.
- Heart failure (HF): New onset or worsening heart failure may occur during initiation or titration. Use with caution in patients with compensated heart failure; monitor for a worsening of the condition and discontinue if symptoms of heart failure occur. Use is contraindicated in patients with uncontrolled (or decompensated) heart failure.
- Myasthenia gravis: Use with caution in patients with myasthenia gravis; may worsen disease.
- Myocardial infarction: Use with caution within the first 2 weeks post-MI, especially in patients with markedly impaired ventricular function (experience limited).
- Peripheral vascular disease (PVD) and Raynaud disease: Can precipitate or aggravate symptoms of arterial insufficiency in patients with PVD and Raynaud disease. Use with caution and monitor for progression of arterial obstruction.
- Pheochromocytoma (untreated): Adequate alpha-blockade is required prior to use of any beta-blocker.
- Renal impairment: [US Boxed Warning]: Adjust dosing interval based on CrCl to decrease risk of proarrhythmia; QT interval prolongation is directly related to sotalol concentration. CrCl must be calculated with dose initiation and dose increases. When used for atrial fibrillation/flutter, sotalol is contraindicated in patients with CrCl <40 mL/minute.
- Thyroid disease: May mask signs of hyperthyroidism (eg, tachycardia). If thyrotoxicosis is suspected, carefully manage and monitor; abrupt withdrawal may exacerbate symptoms of hyperthyroidism or precipitate thyroid storm.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Bradycardia may be observed more frequently in elderly patients (>65 years of age); dosage reductions may be necessary.
Other warnings/precautions:
- Abrupt withdrawal: Beta-blocker therapy should not be withdrawn abruptly (particularly in patients with CAD), but gradually tapered to avoid acute tachycardia, hypertension, and/or ischemia. Severe exacerbation of angina, ventricular arrhythmias, and myocardial infarction (MI) have been reported following abrupt withdrawal of beta-blocker therapy. Temporary but prompt resumption of beta-blocker therapy may be indicated with worsening of angina or acute coronary insufficiency. When QTc prolongation occurs, consider weighing the risk of abrupt withdrawal of sotalol with the risk of QTc prolongation. Use of an alternative beta-blocker may be indicated if worsening angina or acute coronary insufficiency occurs when sotalol is withdrawn abruptly due to QTc prolongation.
- Major surgery: Chronic beta-blocker therapy should not be routinely withdrawn prior to major surgery.
Monitoring Parameters
Serum creatinine (creatinine clearance), magnesium, potassium; heart rate, blood pressure; ECG (eg, QTc interval, PR interval).
Oral: During initiation and titration period, monitor QTc interval 2 to 4 hours after each dose. If QTc interval is ≥500 msec, reduce dose, prolong the dosing interval, or discontinue sotalol. If the QTc interval is <500 msec after 3 days (after fifth or sixth dose if patient receiving once-daily dosing), patient may be discharged on current regimen. Monitor QTc interval periodically thereafter.
IV: Measure QTc interval after completion of each infusion.
Consult individual institutional policies and procedures.
Pregnancy
Pregnancy Risk Factor
B
Pregnancy Considerations
Sotalol crosses the placenta.
Adverse fetal/neonatal events have been reported with beta-blockers as a class. If maternal use of a beta-blocker is needed, fetal growth should be monitored during pregnancy and the newborn should be monitored for 48 hours after delivery for bradycardia, hypoglycemia, and respiratory depression (ESC [Regitz-Zagrosek 2018]).
Because sotalol crosses the placenta in concentrations similar to the maternal serum, it has been studied for the treatment of fetal atrial flutter or fetal supraventricular tachycardia (SVT). Sotalol may be considered for the in utero management of fetal SVT or atrial flutter with hydrops or ventricular dysfunction. Sotalol may also be considered for SVT without hydrops or ventricular dysfunction if heart rate is ≥200 bpm, atrial flutter, or other rare tachycardias with an average heart rate of ≥200 bpm. In addition, sotalol may be considered fetal ventricular tachycardia (VT) with normal QTc with or without hydrops but is contraindicated for the treatment of fetal VT when long QT syndrome is suspected or confirmed (AHA [Donofrio 2014]).
The pharmacokinetic properties of sotalol are not significantly altered by pregnancy (O’Hare 1983). Sotalol may be used for the treatment of maternal ventricular arrhythmias, atrial fibrillation/atrial flutter, or supraventricular tachycardia during pregnancy; consult current guidelines for specific recommendations (ACC/AHA/HRS [Page 2015]; ESC [Regitz-Zagrosek 2018]).
Patient Education
What is this drug used for?
- It is used to treat certain types of life-threatening abnormal heartbeats.
- It is used to keep a normal heartbeat in people who have a certain type of abnormal heartbeat (atrial fibrillation or atrial flutter).
Frequently reported side effects of this drug
- Headache
- Diarrhea
- Vomiting
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe dizziness
- Passing out
- Chest pain
- Slow heartbeat
- Fast heartbeat
- Abnormal heartbeat
- Severe loss of strength and energy
- Vision changes
- Injection site pain
- Irritation
- Edema
- Sweating a lot
- Heart problems like cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.