Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Generic: 500 mg
Pharmacology
Mechanism of Action
Interferes with bacterial growth by inhibiting bacterial folic acid synthesis through competitive antagonism of PABA
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed
Distribution
Throughout body tissues and fluids including pleural, peritoneal, synovial, and ocular fluids; throughout total body water; readily diffused into CSF
Metabolism
Via N-acetylation
Excretion
Urine (43% to 60% as unchanged drug, 15% to 40% as metabolites)
Time to Peak
Within 3-6 hours
Half-Life Elimination
10 hours
Protein Binding
38% to 48%
Use: Labeled Indications
Treatment of chancroid, trachoma, inclusion conjunctivitis, nocardiosis, urinary tract infections, toxoplasmosis encephalitis, malaria, meningococcal meningitis, acute otitis media, meningitis (adjunctive); prophylaxis of rheumatic fever
Contraindications
Hypersensitivity to any sulfa drug or any component of the formulation; infants <2 months of age unless indicated for the treatment of congenital toxoplasmosis; pregnancy (at term); breast-feeding
Dosage and Administration
Dosing: Adult
General dosing guidelines: Oral: 2 to 4 g/day in 3 to 6 divided doses
Rheumatic fever prophylaxis (off-label dose) (Gerber [AHA 2009]): Oral:
≤27 kg: 500 mg once daily
>27 kg: 1,000 mg once daily
Toxoplasma gondii encephalitis: Oral:
Treatment of acute infection (duration of therapy: ≥6 weeks): 1,000 mg (<60 kg) or 1,500 mg (≥60 kg) every 6 hours in combination with pyrimethamine plus leucovorin calcium (preferred) or alternatively, may give 1,000 mg (<60 kg) or 1,500 mg (≥60 kg) every 6 hours in combination with atovaquone (HHS [OI adult 2016])
Chronic maintenance: 2,000 to 4,000 mg/day in 2 to 4 divided doses in combination with pyrimethamine and leucovorin calcium (preferred) or alternatively, may give 2,000 to 4,000 mg/day in 2 to 4 divided doses in combination with atovaquone (HHS [OI adult 2016])
Manufacturer’s labeling: Dosing in the prescribing information may not reflect current clinical practice. Initial: 2,000 to 4,000 mg; maintenance: 2,000 to 4,000 mg/day in 3 to 6 divided doses.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
General dosing, susceptible infection: Infants ≥2 months, Children, and Adolescents: Oral: 120 to 150 mg/kg/day in divided doses 4 to 6 times daily; maximum daily dose: 6 g/day (Red Book [AAP 2018])
Manufacturer's labeling: Note: May not be reflective of current clinical practice. Oral: Initial: 75 mg/kg/dose or 2,000 mg/m2/dose once followed by maintenance: 150 mg/kg/day or 4,000 mg/m2/day divided every 4 to 6 hours; maximum daily dose: 6 g/day
Toxoplasmosis:
Congenital: Infants: Oral: 50 mg/kg/dose every 12 hours for 12 months; use in conjunction with pyrimethamine and supplemental leucovorin (HHS [pediatric OI 2016]; Red Book [AAP 2018])
Acquired:
Acute induction therapy: HIV-exposed/-positive or immunocompromised/competent with severe primary toxoplasmosis or reactivation: Infants ≥2 months, Children, and Adolescents: Oral: 25 to 50 mg/kg/dose every 6 hours; maximum dose: 1,500 mg/dose; maximum daily dose: 6 g/day; use in conjunction with pyrimethamine and supplemental leucovorin. Continue acute induction therapy for at least 6 weeks, then follow with chronic suppressive therapy (HHS [pediatric OI 2016]; Red Book [AAP 2018]).
Chorioretinitis: Non-HIV-exposed/-positive: Children and Adolescents: Oral: 75 mg/kg once followed by 50 mg/kg/dose twice daily; maximum daily dose: 4,000 mg/day; use in conjunction with pyrimethamine and supplemental leucovorin; treat for 1 to 2 weeks after resolution of clinical manifestations (typically 4 to 6 weeks total) (Red Book [AAP 2018])
Suppressive therapy (HIV-exposed/-positive): Infants ≥2 months and Children: Oral: 42.5 to 60 mg/kg/dose twice daily; use in conjunction with pyrimethamine and supplemental leucovorin; maximum daily dose: 4,000 mg/day
Encephalitis; Toxoplasma gondii; treatment (HIV-exposed/-positive); preferred (HHS [adult OI 2018]): Adolescents:
Acute therapy: At least 6 weeks of therapy recommended; use in conjunction with pyrimethamine and supplemental leucovorin combination therapy or with atovaquone
Patient weight <60 kg: Oral: 1,000 mg every 6 hours
Patient weight ≥60 kg: Oral: 1,500 mg every 6 hours
Chronic maintenance therapy: Oral: 2,000 to 4,000 mg/day in divided doses 2 to 4 times daily in conjunction with pyrimethamine and supplemental leucovorin or with atovaquone; begin after completion of acute therapy
Rheumatic fever; secondary prophylaxis: Infants ≥2 months, Children, and Adolescents:
AHA Recommendations (AHA [Gerber 2009]; Red Book [AAP 2018]):
Patient weight ≤27 kg: Oral: 500 mg once daily
Patient weight >27 kg: Oral: 1,000 mg once daily
Manufacturer's labeling: Note: May not be reflective of current clinical practice:
≤30 kg: Oral: 500 mg once daily
≥30 kg: Oral: 1,000 mg once daily
Extemporaneously Prepared
A 200 mg/mL oral suspension may be made with sulfadiazine powder and sterile water. Place 50 g sulfadiazine powder in a glass mortar. Add small portions of sterile water and mix to a uniform paste; mix while incrementally adding sterile water to almost 250 mL; transfer to a calibrated bottle, rinse mortar with sterile water, and add sufficient quantity of sterile water to make 250 mL. Label "shake well" and "refrigerate". Stable for 3 days refrigerated. Note: Suspension may also be prepared by crushing one-hundred 500 mg tablets; however, it is stable for only 2 days.
Pathmanathan U, Halgrain D, Chiadmi F, et al, "Stability of Sulfadiazine Oral Liquids Prepared From Tablets and Powder," J Pharm Pharm Sci, 2004, 7(1):84-7.15144740
Administration
Administer with at least 8 ounces of water and around-the-clock to promote less variation in peak and trough serum levels. Oral sodium bicarbonate may be used to alkalinize the urine of patients unable to maintain adequate fluid intake (in order to prevent crystalluria, azotemia, oliguria) (Lerner, 1996).
Dietary Considerations
Supplemental leucovorin calcium should be administered to reverse symptoms or prevent problems due to folic acid deficiency.
Storage
Store at controlled room temperature of 20°C to 25°C (68°F to 77°F). Protect from light.
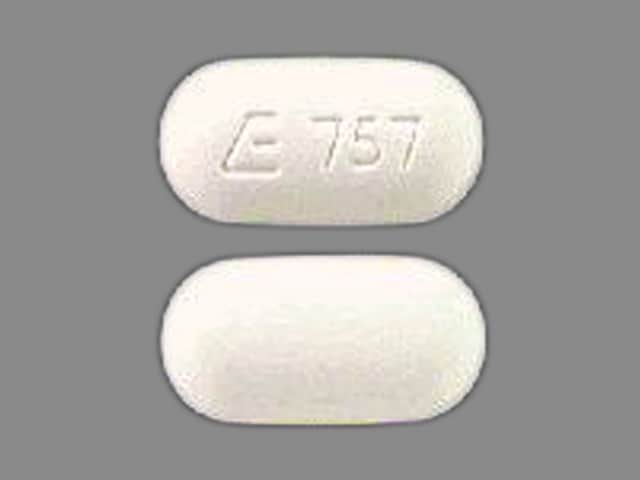
SulfADIAZINE Images
Drug Interactions
Ajmaline: Sulfonamides may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Alpelisib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Androgens: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Exceptions: Danazol. Monitor therapy
Antidiabetic Agents: May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Chloroprocaine: May diminish the therapeutic effect of Sulfonamide Antibiotics. Management: Avoid concurrent use of chloroprocaine and systemic sulfonamide-based antimicrobials whenever possible. Consider therapy modification
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
CycloSPORINE (Systemic): Sulfonamide Antibiotics may enhance the nephrotoxic effect of CycloSPORINE (Systemic). Sulfonamide Antibiotics may decrease the serum concentration of CycloSPORINE (Systemic). Monitor therapy
CYP2C9 Inducers (Moderate): May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
CYP2C9 Inhibitors (Moderate): May decrease the metabolism of CYP2C9 Substrates (High risk with Inhibitors). Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C9 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Dexketoprofen: May enhance the adverse/toxic effect of Sulfonamides. Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP2C9 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C9 substrate should be performed with caution and close monitoring. Consider therapy modification
Fosphenytoin-Phenytoin: SulfADIAZINE may increase the serum concentration of Fosphenytoin-Phenytoin. Monitor therapy
Herbs (Hypoglycemic Properties): May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Hypoglycemia-Associated Agents: May enhance the hypoglycemic effect of other Hypoglycemia-Associated Agents. Monitor therapy
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C9 Substrates (High Risk with Inhibitors or Inducers). Lumacaftor and Ivacaftor may increase the serum concentration of CYP2C9 Substrates (High Risk with Inhibitors or Inducers). Monitor therapy
Maitake: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Mecamylamine: Sulfonamides may enhance the adverse/toxic effect of Mecamylamine. Avoid combination
Methenamine: May enhance the adverse/toxic effect of Sulfonamide Antibiotics. Specifically, the combination may result in the formation of an insoluble precipitate in the urine. Avoid combination
Methotrexate: Sulfonamide Antibiotics may enhance the adverse/toxic effect of Methotrexate. Management: Consider avoiding concomitant use of methotrexate and therapeutic doses of sulfonamides (eg, trimethoprim/sulfamethoxazole). Patients receiving prophylactic doses of trimethoprim/sulfamethoxazole and methotrexate should be carefully monitored. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of CYP2C9 Substrates (High risk with Inhibitors). Management: Use CYP2C9 substrates at the lowest recommended dose, and monitor closely for adverse effects, during and in the 2 weeks following mifepristone treatment. Consider therapy modification
Monoamine Oxidase Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Pegvisomant: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Potassium P-Aminobenzoate: May diminish the therapeutic effect of Sulfonamide Antibiotics. Avoid combination
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Procaine: May diminish the therapeutic effect of Sulfonamide Antibiotics. Avoid combination
Prothionamide: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Pyrimethamine: May enhance the adverse/toxic effect of Sulfonamide Antibiotics. Monitor therapy
Quinolones: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Quinolones may diminish the therapeutic effect of Blood Glucose Lowering Agents. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
Rifapentine: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Salicylates: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Sulfonylureas: Sulfonamide Antibiotics may enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Sulfonamide Antibiotics may enhance the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Adverse Reactions
Frequency not defined.
Cardiovascular: Allergic myocarditis, periarteritis nodosa
Central nervous system: Ataxia, chills, depression, hallucination, headache, insomnia, peripheral neuritis, seizure, vertigo
Dermatologic: Erythema multiforme, exfoliative dermatitis, pruritus, skin photosensitivity, skin rash, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Endocrine & metabolic: Hypoglycemia, thyroid dysfunction
Gastrointestinal: Abdominal pain, anorexia, diarrhea, nausea, pancreatitis, stomatitis, vomiting
Genitourinary: Crystalluria, diuresis, toxic nephrosis (with anuria and oliguria)
Hematologic & oncologic: Agranulocytosis, aplastic anemia, hemolytic anemia, hypoprothrombinemia, leukopenia, methemoglobinemia, purpura, thrombocytopenia
Hepatic: Hepatitis
Hypersensitivity: Anaphylactoid reaction
Immunologic: Serum sickness-like reaction
Neuromuscular & skeletal: Arthralgia, lupus erythematosus
Ophthalmic: Conjunctival injection, injected sclera, periorbital edema
Otic: Tinnitus
Renal: Nephrolithiasis
Miscellaneous: Fever
Warnings/Precautions
Concerns related to adverse effects:
- Blood dyscrasias: Fatalities associated with severe reactions including agranulocytosis, aplastic anemia and other blood dyscrasias have occurred; discontinue use at first sign of rash or signs of serious adverse reactions.
- Dermatologic reactions: Fatalities associated with severe reactions including Stevens-Johnson syndrome and toxic epidermal necrolysis have occurred; discontinue use at first sign of rash.
- Hepatic necrosis: Fatalities associated with hepatic necrosis have occurred; discontinue use at first sign of rash.
- Sulfonamide (“sulfa”) allergy: Traditionally, concerns for cross-reactivity have extended to all compounds containing the sulfonamide structure (SO2NH2). An expanded understanding of allergic mechanisms indicates cross-reactivity between antibiotic sulfonamides and nonantibiotic sulfonamides may not occur, or at the very least this potential is extremely low (Brackett 2004; Johnson 2005; Slatore 2004; Tornero 2004). In particular, mechanisms of cross-reaction due to antibody production (anaphylaxis) are unlikely to occur with nonantibiotic sulfonamides and antibiotic sulfonamides. A nonantibiotic sulfonamide compound which contains the arylamine structure and therefore may cross-react with antibiotic sulfonamides is sulfasalazine (Zawodniak 2010). T-cell-mediated (type IV) reactions (eg, maculopapular rash) are less understood and it is not possible to completely exclude this potential based on current insights. In cases where prior reactions were severe (Stevens-Johnson syndrome/TEN), some clinicians choose to avoid exposure to these classes.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Allergies/asthma: Use with caution in patients with allergies or asthma.
- Glucose 6-phosphate dehydrogenase (G6PD) deficiency: Use with caution in patients with G6PD deficiency; hemolysis may occur.
- Hepatic impairment: Use with caution in patients with hepatic impairment.
- Renal impairment: Use with caution in patients with renal impairment; dosage modification required. Maintain adequate hydration to prevent crystalluria.
Special populations:
- Neonates: Sulfa antibiotics have been shown to displace bilirubin from protein binding sites which may potentially lead to hyperbilirubinemia and kernicterus in neonates and young infants; do not use in neonates; avoid use in infants <2 months unless other options are not available.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC, 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors, 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
Other warnings/precautions:
- Appropriate use: Not for the treatment of group A beta-hemolytic streptococcal infections.
Monitoring Parameters
Perform culture and sensitivity testing prior to initiating therapy; frequent CBC and urinalysis during therapy; signs of serious blood disorders (sore throat, fever, pallor, purpura, dark urine, jaundice); CD4+ count in HIV-exposed/-positive patients treated for toxoplasmosis
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Sulfadiazine crosses the placenta (Speert 1943).
Current studies evaluating maternal use of sulfonamides during pregnancy and the development of birth defects have had mixed results (ACOG 717 2017).
Sulfadiazine is recommended for use in pregnant women to prevent T gondii infection of the fetus, for the maternal treatment of Toxoplasmic gondii encephalitis, and as an alternative agent for the secondary prevention of rheumatic fever (AHA [Gerber 2009]; HHS OI adult 2017). Sulfonamides may be used to treat other infections in pregnant women when clinically appropriate for confirmed infections caused by susceptible organisms; use during the first trimester should be limited to situations where no alternative therapies are available. Alternative antibiotics should be used in pregnant patients with G6PD deficiency (ACOG 717 2017).
Due to the theoretical increased risk for hyperbilirubinemia and kernicterus, sulfadiazine is contraindicated by the manufacturer for use near term. Neonatal health care providers should be informed if maternal sulfonamide therapy is used near the time of delivery (HHS OI adult 2017).
Patient Education
What is this drug used for?
- It is used to treat or prevent bacterial infections.
Frequently reported side effects of this drug
- Headache
- Dizziness
- Nausea
- Vomiting
- Diarrhea
- Lack of appetite
- Trouble sleeping
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Methemoglobinemia like blue or gray color of the lips, nails, or skin; abnormal heartbeat; seizures; severe dizziness or passing out; severe headache; fatigue; loss of strength and energy; or shortness of breath
- Severe sulfonamide reaction like rash; red, swollen, blistered, or peeling skin; red or irritated eyes; mouth, throat, nose, or eye sores; fever, chills, or sore throat; cough that is new or worse; loss of strength and energy; any bruising or bleeding; or signs of liver problems like dark urine, fatigue, lack of appetite nausea or abdominal pain, light-colored stools, vomiting, or yellow skin
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting
- Kidney stone like back pain, abdominal pain, or blood in the urine
- Unable to pass urine
- Change in amount of urine passed
- Pale skin
- Chest pain
- Sensing things that seem real but are not
- Joint pain
- Burning or numbness feeling
- Depression
- Noise or ringing in the ears
- Seizures
- Change in balance
- Purple patches on skin or mouth
- Clostridioides (formerly Clostridium) difficile-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.