Boxed Warning
Uterine malignancies and thromboembolic events:
Serious and life-threatening events from the use of tamoxifen include uterine malignancies, stroke, and pulmonary embolism. Fatal cases of each type of event have occurred.
Incidence rates per 1,000 woman-years for these events were estimated from the National Surgical Adjuvant Breast and Bowel Project (NSABP) P-1 trial in women at high risk for breast cancer:
-
Endometrial adenocarcinoma: 2.20 for tamoxifen versus 0.71 for placebo
-
Uterine sarcoma: 0.17 for tamoxifen versus 0.04 for placebo
-
Stroke: 1.43 for tamoxifen versus 1.00 for placebo.
-
Pulmonary embolism: 0.75 for tamoxifen versus 0.25 for placebo
Discuss the potential benefits of tamoxifen versus the potential risks of these serious events with women at high risk for breast cancer and women with ductal carcinoma in situ (DCIS) considering tamoxifen to reduce the risk of developing breast cancer. For most patients already diagnosed with breast cancer, the benefits of tamoxifen outweigh its risks.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Oral:
Soltamox: 10 mg/5 mL (150 mL) [sugar free; contains alcohol, usp, propylene glycol; licorice-aniseed flavor]
Tablet, Oral:
Generic: 10 mg, 20 mg
Pharmacology
Mechanism of Action
Tamoxifen is a selective estrogen receptor modulator (SERM) that competitively binds to estrogen receptors on tumors and other tissue targets, producing a nuclear complex that decreases DNA synthesis and inhibits estrogen effects; nonsteroidal agent with potent antiestrogenic properties which compete with estrogen for binding sites in breast and other tissues; cells accumulate in the G0 and G1 phases; therefore, tamoxifen is cytostatic rather than cytocidal.
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed
Distribution
Widely distributed to most tissues, particularly tissues that inhibit estrogen receptors (Perry 2012)
Metabolism
Hepatic; via CYP2D6 to 4-hydroxytamoxifen and via CYP3A4/5 to N-desmethyl-tamoxifen. Each is then further metabolized into endoxifen (4-hydroxy-tamoxifen via CYP3A4/5 and N-desmethyl-tamoxifen via CYP2D6); both 4-hydroxy-tamoxifen and endoxifen are 30- to 100-fold more potent than tamoxifen
Excretion
~65% (primarily fecal); <30% as unchanged drug and unconjugated metabolites
Clearance: Higher (~2.3-fold) in female pediatric patients (2 to 10 years) compared to adult breast cancer patients; within pediatric population, clearance faster in children 2 to 6 years compared to older children
Time to Peak
Serum: Children 2 to 10 years (female): ~8 hours; Adults: ~5 hours
Half-Life Elimination
Tamoxifen: ~5 to 7 days; N-desmethyl tamoxifen: ~14 days
Protein Binding
Highly protein bound (Perry 2012)
Use: Labeled Indications
Breast cancer, risk reduction: Risk reduction in females at high risk: To reduce the incidence of breast cancer in adult females at high risk for breast cancer
Breast cancer, treatment:
Adjuvant treatment: Adjuvant treatment of adult patients with early stage estrogen receptor-positive breast cancer; to reduce the incidence of contralateral breast cancer in adult patients when used as adjuvant therapy for the treatment of breast cancer
Ductal carcinoma in situ: To reduce the risk of invasive breast cancer in adult females with ductal carcinoma in situ (following breast surgery and radiation)
Metastatic breast cancer: Treatment of adult patients with estrogen receptor-positive metastatic breast cancer
Use: Off Label
Desmoid tumors, progressive or recurrentc
Data from a study evaluating the use of tamoxifen (in combination with sulindac) suggest that tamoxifen may be beneficial for the treatment of this condition Hansmann 2004.
Endometrial carcinoma, recurrent, metastatic, or high-risk (endometrioid histologies only)b
Data from two phase II trials in patients with advanced or recurrent endometrial carcinoma support the use of tamoxifen for the treatment of this condition Fiorica 2004, Thigpen 2001.
Gynecomastiaa
Data from controlled trials support the use of tamoxifen for preventing or treating antiandrogen-associated gynecomastia in prostate cancer patients
Idiopathic male infertilitycyes
In meta-analyses of randomized controlled trials evaluating the treatment of idiopathic male infertility, tamoxifen may improve semen parameters in some patients; an increase in pregnancy rates was not observed in all studies Chua 2013, Omar 2019.
Based on the European Academy of Andrology guideline, management of oligo-astheno-teratozoospermia, a recommendation cannot be made for or against the use of tamoxifen in the treatment of idiopathic male infertility based on the currently available evidence Colpi 2018.
Induction of ovulation (in breast cancer patients)b
Data from a prospective controlled study in women with breast cancer support the use of tamoxifen (in combination with low-dose follicle-stimulating hormone [FSH]) for ovarian stimulation, although letrozole in combination with FSH may be preferred due to lower peak estradiol levels with this combination Cakmak 2013, Oktay 2005.
Mastalgia, severeb
Data from a small controlled trial suggest that tamoxifen may be beneficial for the treatment of severe mastalgia
Ovarian cancer, advanced and/or recurrentc
Data from two studies evaluating the use of tamoxifen for the treatment of advanced ovarian cancer suggest that tamoxifen may be beneficial for the treatment of this condition Hatch 1991, Markman 1996.
Contraindications
Known hypersensitivity (eg, angioedema, serious skin reactions) to tamoxifen or any component of the formulation; concurrent warfarin therapy or history of deep vein thrombosis or pulmonary embolism (when tamoxifen is used for breast cancer risk reduction in women at high risk for breast cancer or risk reduction of invasive breast cancer after treatment of ductal carcinoma in situ [DCIS])
Dosage and Administration
Dosing: Adult
Note: For the treatment of breast cancer, patients receiving both tamoxifen and chemotherapy should receive treatment sequentially, with tamoxifen following completion of chemotherapy.
Breast cancer, risk reduction (pre- and postmenopausal high-risk females): Oral: 20 mg once daily for 5 years.
Breast cancer, treatment: Oral:
Adjuvant therapy: 20 mg once daily
Duration of therapy: The American Society of Clinical Oncology (ASCO) guidelines for Adjuvant Endocrine Therapy of Hormone-Receptor Positive Breast Cancer (Focused Update) recommend the following durations of therapy based on menopausal status (Burstein 2014):
Pre- or perimenopausal at endocrine therapy initiation: Tamoxifen for an initial duration of 5 years; if pre- or perimenopausal (or status cannot be determined) after 5 years of therapy, may continue tamoxifen for a total duration of 10 years. If postmenopausal after 5 years of tamoxifen therapy, may continue tamoxifen for a total duration of 10 years, or switch to an aromatase inhibitor (AI) for up to a total duration of 10 years of endocrine therapy.
Postmenopausal at endocrine therapy initiation: Tamoxifen for a total duration of 10 years or tamoxifen for an initial duration of 5 years, followed by an AI for up to 5 years (for a total duration of 10 years of endocrine therapy) or tamoxifen for 2 to 3 years, followed by an AI for up to 5 years (for a total duration of 7 to 8 years of endocrine therapy) or an AI for 5 years.
Ductal carcinoma in situ (DCIS) (females), to reduce the risk for invasive breast cancer: 20 mg once daily for 5 years.
Metastatic: 20 mg once daily. Although the manufacturer's labeling recommends dosing of 20 to 40 mg daily (with doses >20 mg administered in 2 divided doses), clinical benefit has not been demonstrated with doses above 20 mg daily (Bratherton 1984).
Guideline recommendations: The American Society of Clinical Oncology (ASCO) guidelines for Endocrine Therapy for Hormone-Receptor Positive Metastatic Breast Cancer recommend the following based on menopausal status (Rugo 2016):
Premenopausal: Tamoxifen (in combination with ovarian suppression) may be offered as first-line therapy in patients with no prior endocrine therapy or in those who have received prior treatment with ovarian suppression and an AI; tamoxifen (with continued ovarian suppression) may also be offered as second-line therapy. Tamoxifen alone may be considered, but combination therapy is preferred.
Postmenopausal: Tamoxifen may be offered as second-line therapy in patients with no prior endocrine therapy. In patients who have received prior endocrine therapy with tamoxifen, tamoxifen may be offered first- or second-line in patients with late relapse (>12 months since adjuvant therapy). In patients who have received prior endocrine therapy with an AI, tamoxifen may be offered as first- or second-line therapy.
Duration of therapy: Continue tamoxifen treatment until documented disease progression (documented by imaging, clinical examination, or disease-related symptoms).
Endometrial carcinoma, recurrent, metastatic, or high-risk (endometrioid histologies only) (off-label use): Oral:
Monotherapy: 20 mg twice daily until disease progression or unacceptable toxicity (Thigpen 2001).
Combination therapy: 20 mg twice daily for 3 weeks (alternating with megestrol acetate every 3 weeks); continue alternating until disease progression or unacceptable toxicity) (Fiorica 2004).
Gynecomastia (off-label use): Oral: 20 mg once daily for up to 12 months (Boccardo 2005; Fradet 2007). The majority of published experiences have been in adult males with prostate cancer receiving bicalutamide. Use has also been reported in patients with idiopathic gynecomastia.
Idiopathic male infertility (off label use): Oral: 20 to 30 mg once daily for 3 to 6 months, then proceed to assisted reproductive therapy if pregnancy has not been achieved (Chua 2013; Colpi 2018).
Induction of ovulation (in breast cancer patients) (off-label use): Oral: 60 mg daily starting on the second or third day of the menstrual cycle (in combination with low-dose follicle-stimulating hormone [FSH]), and continued until the day of hCG administration (Oktay 2005).
Mastalgia, severe (off-label use): Oral: 10 mg once daily for 3 months; may consider further treatment if relapse occurs (Fentiman 1988).
Ovarian cancer, advanced and/or recurrent (off-label use): Oral: 20 mg twice daily (Hatch 1991; Markman 1996).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
McCune-Albright syndrome; precocious puberty: Limited data available: Children 2 to 10 years: Oral: 20 mg once daily; dosing based on a trial of 25 girls ≤10 years of age (range: 2.9 to 10.9 years) who received treatment for 1 year; frequency of vaginal bleeding episodes were decreased; growth velocity was significantly decreased prior to pretreatment rates as was skeletal maturation; ovarian and uterine volumes were increased; further studies are needed (Eugester 2003)
Extemporaneously Prepared
A 0.5 mg/mL oral suspension may be prepared with tablets. Place two 10 mg tablets into 40 mL purified water and let stand ~2 to 5 minutes. Stir until tablets are completely disintegrated (dispersion time for each 10 mg tablet is ~2 to 5 minutes). Administer immediately after preparation. To ensure the full dose is administered, rinse glass several times with water and administer residue.
Lam MS, "Extemporaneous Compounding of Oral Liquid Dosage Formulations and Alternative Drug Delivery Methods for Anticancer Drugs," Pharmacotherapy, 2011, 31(2):164-92.21275495
Administration
Oral: Administer tablets or oral solution orally with or without food. Use supplied dosing cup for oral solution.
Storage
Oral solution: Store at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C to 30°C (59°F to 86°F). Do not freeze or refrigerate. Protect from light. Discard opened bottle after 3 months.
Tablets: Store at 20°C to 25°C (68°F to 77°F). Protect from light. Avoid excessive heat.
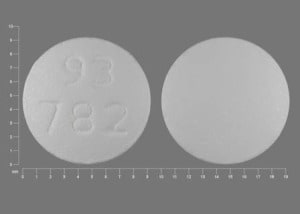
Tamoxifen Images
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Ajmaline: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Alpelisib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Anastrozole: Tamoxifen may decrease the serum concentration of Anastrozole. Consider therapy modification
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Asunaprevir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Bexarotene (Systemic): May decrease the serum concentration of Tamoxifen. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Chloroquine: Tamoxifen may enhance the adverse/toxic effect of Chloroquine. Specifically, concomitant use of tamoxifen and chloroquine may increase the risk of retinal toxicity. Monitor therapy
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP2C9 Inhibitors (Moderate): May decrease the metabolism of CYP2C9 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Moderate): May decrease serum concentrations of the active metabolite(s) of Tamoxifen. Specifically, CYP2D6 inhibitors may decrease the metabolic formation of highly potent active metabolites. Management: Consider alternatives with less of an inhibitory effect on CYP2D6 activity when possible. Consider therapy modification
CYP2D6 Inhibitors (Strong): May decrease serum concentrations of the active metabolite(s) of Tamoxifen. Specifically, strong CYP2D6 inhibitors may decrease the metabolic formation of highly potent active metabolites. Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease serum concentrations of the active metabolite(s) of Tamoxifen. CYP3A4 Inducers (Strong) may decrease the serum concentration of Tamoxifen. Management: Consider alternatives to concomitant use of strong CYP3A4 inducers and tamoxifen. If the combination cannot be avoided, monitor for reduced therapeutic effects of tamoxifen. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C9 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP2C9 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C9 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Hydroxychloroquine: Tamoxifen may enhance the adverse/toxic effect of Hydroxychloroquine. Specifically, concomitant use of tamoxifen and hydroxychloroquine may increase the risk of retinal toxicity. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Letrozole: Tamoxifen may decrease the serum concentration of Letrozole. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lumefantrine: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP2C9 Substrates (High risk with Inhibitors). Management: Use CYP2C9 substrates at the lowest recommended dose, and monitor closely for adverse effects, during and in the 2 weeks following mifepristone treatment. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mipomersen: Tamoxifen may enhance the hepatotoxic effect of Mipomersen. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Ospemifene: Selective Estrogen Receptor Modulators may enhance the adverse/toxic effect of Ospemifene. Ospemifene may also enhance adverse/toxic effects of other Selective Estrogen Receptor Modulators. Selective Estrogen Receptor Modulators may diminish the therapeutic effect of Ospemifene. Ospemifene may also diminish the therapeutic effects of other Selective Estrogen Receptor Modulators. Avoid combination
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
QuiNINE: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Ribociclib: May increase the serum concentration of Tamoxifen. Management: Concurrent use of ribociclib with tamoxifen is not indicated. Use of this combination may increase the effects and toxicities of tamoxifen. Consider therapy modification
Rifamycin Derivatives: May increase the metabolism of Tamoxifen. Consider therapy modification
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Vitamin K Antagonists (eg, warfarin): Tamoxifen may increase the serum concentration of Vitamin K Antagonists. Avoid combination
Test Interactions
T4 elevations (which may be explained by increases in thyroid-binding globulin) have been reported; not accompanied by clinical hyperthyroidism.
Variations in the vagina smear karyopyknotic index and various degrees of Pap smear estrogen effect have been observed in postmenopausal women taking tamoxifen.
Adverse Reactions
>10%:
Cardiovascular: Vasodilation (41%), flushing (33%), hypertension (11%), peripheral edema (11%)
Dermatologic: Skin changes (6% to 19%), skin rash (13%)
Endocrine & metabolic: Hot flash (3% to 80%), fluid retention (32%), weight loss (23%), amenorrhea (16%)
Gastrointestinal: Nausea (5% to 26%), nausea and vomiting (12%)
Genitourinary: Vaginal discharge (12% to 55%), irregular menses (13% to 25%), vaginal hemorrhage (2% to 23%)
Hematologic & oncologic: Lymphedema (11%)
Nervous system: Fatigue (≤18%), mood changes (12% to 18%), pain (3% to 16%), depression (2% to 12%)
Neuromuscular & skeletal: Asthenia (≤18%), arthritis (14%), arthralgia (11%)
Respiratory: Pharyngitis (14%)
1% to 10%:
Cardiovascular: Chest pain (5%), venous thrombosis (5%), edema (4%), ischemic heart disease (3%), deep vein thrombosis (≤2%)
Dermatologic: Diaphoresis (6%), alopecia (≤5%)
Endocrine & metabolic: Infrequent uterine bleeding (9%), weight gain (9%), menstrual disease (6%), hypercholesterolemia (3%), ovarian cyst (3%)
Gastrointestinal: Abdominal pain (9%), constipation (4% to 8%), diarrhea (7%), dyspepsia (6%), abdominal cramps (1%), anorexia (1%)
Genitourinary: Urinary tract infection (10%), leukorrhea (9%), mastalgia (6%), vaginitis (5%), vulvovaginitis (5%)
Hematologic & oncologic: Thrombocytopenia (2% to 10%), anemia (5%), breast neoplasm (5%), neoplasm (5%; second primary)
Hepatic: Increased serum aspartate aminotransferase (5%), increased serum bilirubin (2%)
Hypersensitivity: Hypersensitivity reaction (3%)
Infection: Infection (≤9%), sepsis (≤6%)
Nervous system: Insomnia (9%), dizziness (8%), headache (8%), anxiety (6%), paresthesia (5%)
Neuromuscular & skeletal: Back pain (10%), bone fracture (7%), osteoporosis (7%), ostealgia (6%), arthropathy (5%), myalgia (5%), musculoskeletal pain (3%)
Ophthalmic: Cataract (7%)
Renal: Increased serum creatinine (2%)
Respiratory: Cough (4% to 9%), dyspnea (8%), flu-like symptoms (6%), bronchitis (5%), sinusitis (5%), throat irritation (oral solution: 5%)
Miscellaneous: Cyst (5%)
Frequency not defined:
Cardiovascular: Cerebrovascular accident
Dermatologic: Pruritus vulvae
Endocrine & metabolic: Hypercalcemia
Gastrointestinal: Cholestasis, dysgeusia
Genitourinary: Vaginal dryness
Hematologic & oncologic: Tumor flare (during treatment of metastatic breast cancer; generally resolves with continuation; includes increased lesion size and erythema)
Hepatic: Hepatic necrosis, hepatitis, liver steatosis
Nervous system: Tumor pain (during treatment of metastatic breast cancer; generally resolves with continuation)
<1%: Hepatic neoplasm, superficial thrombophlebitis
Postmarketing: Angioedema, bullous pemphigoid, corneal changes, cutaneous lupus erythematosus (Andrew 2014), endometrial carcinoma, endometrial hyperplasia, endometrial polyps, endometriosis, erythema multiforme, hypertriglyceridemia, impotence, interstitial pneumonitis, leukopenia, loss of libido (males), malignant neoplasm of uterus, neutropenia, pancreatitis, pancytopenia, pulmonary embolism, retinal thrombosis, retinopathy, Stevens-Johnson syndrome, subacute cutaneous lupus erythematosus (Andrew 2014), uterine carcinoma, uterine fibroids, vision color changes, visual disturbance
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: Thrombocytopenia (usually grade 1 or 2) and/or leukopenia may occur; neutropenia and pancytopenia have been reported rarely. Although the relationship to tamoxifen therapy is uncertain, rare hemorrhagic episodes have occurred in patients with significant thrombocytopenia. Monitor blood counts periodically.
- Gynecologic effects/malignancies: [US Boxed Warning]: Serious and life-threatening events from the use of tamoxifen include uterine malignancies (including fatal cases). The incidence rates are per 1,000 woman-years and were estimated from the National Surgical Adjuvant Breast and Bowel Project (NSABP) P-1 trial in females at high risk for breast cancer. For endometrial adenocarcinoma, the incidence was 2.20 for tamoxifen versus 0.71 for placebo; for uterine sarcoma, the incidence was 0.17 for tamoxifen versus 0.04 for placebo. Assess potential benefits of tamoxifen versus potential risks of serious events in females at high risk for breast cancer and in ductal carcinoma in situ (DCIS) when considering tamoxifen to reduce the risk of developing breast cancer. For most patients already diagnosed with breast cancer, the benefits of tamoxifen outweigh its risks. Most uterine malignancies seen with tamoxifen are classified as endometrial adenocarcinoma, although uterine sarcomas have also been reported. Uterine sarcoma associated with tamoxifen use was generally associated with a higher FIGO stage (III/IV) at diagnosis, poor prognosis, and short survival. Uterine sarcomas are more frequently associated with a tamoxifen duration of ≥2 years. Endometrial hyperplasia, polyps, endometriosis, uterine fibroids, and ovarian cysts have occurred. Amenorrhea and menstrual irregularities have been reported with tamoxifen use. Monitor and promptly evaluate any report of abnormal vaginal bleeding, menstrual irregularities, changes in vaginal discharge, or pelvic pain/pressure. Patients receiving or who have received tamoxifen in the past should have annual gynecological examinations.
- Hepatotoxicity: Hepatocellular carcinoma has been reported in patients receiving adjuvant tamoxifen at doses of 40 mg twice daily (twice the recommended dose). Tamoxifen has also been associated with elevated transaminases, as well as other less common (and occasionally fatal) hepatic abnormalities including fatty liver, cholestasis, hepatitis, and hepatic necrosis. Monitor liver function periodically.
- Ocular effects: Visual disturbances, including retinal vein thrombosis, retinopathy, corneal changes, color perception changes and increased incidence of cataracts (and the need for cataract surgery) have been reported. Promptly evaluate any visual disturbance.
- Thromboembolic events: [US Boxed Warning]: Serious and life-threatening events from tamoxifen include stroke and pulmonary embolism (PE), including fatal cases. The incidence rates are per 1,000 woman-years and were estimated from the NSABP P-1 trial in women at high risk for breast cancer. For stroke, the incidence was 1.43 for tamoxifen versus 1.00 for placebo; for PE, the incidence was 0.75 for tamoxifen versus 0.25 for placebo. Assess potential benefits of tamoxifen versus potential risks of serious events in females at high risk for breast cancer and in females with DCIS when considering tamoxifen to reduce the risk of developing breast cancer. For most patients already diagnosed with breast cancer, the benefits of tamoxifen outweigh its risks. PE events occurred at an average of 27 months from tamoxifen initiation (range: 2 to 60 months), Deep vein thrombosis events occurred at an average of 19 months (range: 2 months to 57 months) into therapy, and stroke occurred at an average of 30 months (range: 1 to 63 months) after tamoxifen initiation. Tamoxifen is contraindicated in women with DCIS and for the reduction in breast cancer incidence in women at high risk who require warfarin or have a history of deep vein thrombosis or pulmonary embolism. An increased incidence of thromboembolic events has been associated with use; risk is increased with concomitant chemotherapy. Use with caution in individuals with a history of thromboembolic events. Advise patients to immediately report signs/symptoms of thromboembolism.
Disease-related concerns:
- Bone mineral density: Tamoxifen use may be associated with changes in bone mineral density (BMD) and the effects may be dependent upon menstrual status. In postmenopausal women, tamoxifen use is associated with a protective effect on BMD, preventing loss of BMD which lasts over the 5-year treatment period. In premenopausal women, a decline (from baseline) in BMD mineral density has been observed in women who continued to menstruate; may be associated with an increased risk of fractures.
- Hyperlipidemia: Hypercholesterolemia and postmarketing cases of hyperlipidemias have been reported. Periodic monitoring of cholesterol and triglycerides may be indicated in patients with preexisting hyperlipidemias.
- Metastatic breast cancer: Local disease flare and increased bone and tumor pain may occur; may be associated with (good) tumor response; onset is shortly after therapy initiation and usually resolves rapidly. In some patients with bone metastasis, hypercalcemia has occurred, usually within a few weeks of therapy initiation. Institute appropriate hypercalcemia management; discontinue tamoxifen if hypercalcemia is severe.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Selective serotonin reuptake inhibitors (SSRI): Concomitant use with select SSRIs may result in decreased tamoxifen efficacy. Strong CYP2D6 inhibitors (eg, fluoxetine, paroxetine) are reported to interfere with transformation to the active metabolite endoxifen; when possible, select alternative medications with minimal or no impact on endoxifen levels (Sideras 2010). Weak CYP2D6 inhibitors (eg, venlafaxine, citalopram) have minimal effect on the conversion to endoxifen (Jin 2005); escitalopram is also a weak CYP2D6 inhibitor. In a retrospective analysis of breast cancer patients taking tamoxifen and SSRIs, concomitant use of paroxetine and tamoxifen was associated with an increased risk of death due to breast cancer (Kelly 2010).
Special populations:
- CYP2D6 poor metabolizers: Lower plasma concentrations of endoxifen (active metabolite) have been observed in patients with reduced CYP2D6 activity (Jin 2005; Schroth 2009) and may be associated with reduced efficacy, although data is conflicting. Routine CYP2D6 testing is not recommended at this time in order to determine optimal endocrine therapy (Visvanathan 2009).
Dosage form specific issues:
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures, and respiratory depression; use caution (AAP 1997; Zar 2007).
Monitoring Parameters
CBC with platelets, serum calcium, liver function tests; triglycerides and cholesterol (in patients with preexisting hyperlipidemias); INR and PT (in patients on vitamin K antagonists); pregnancy test (prior to treatment in females of reproductive potential); monitor for abnormal vaginal bleeding, menstrual irregularities, pelvic pain/pressure; breast and gynecologic exams (baseline and routine), mammogram (baseline and routine); signs/symptoms of DVT (leg swelling, tenderness) or PE (shortness of breath); ophthalmic exam (if vision problem or cataracts); bone mineral density (premenopausal women). Monitor adherence.
Pregnancy
Pregnancy Considerations
Based on the mechanism of action, and data from animal reproduction studies, in utero exposure to tamoxifen may cause fetal harm. However, available data are insufficient to establish a causal relationship; no pattern of birth defects has been observed, and the long term effects of tamoxifen on development are not known (Braems 2011; Schuurman 2019). There have been reports of vaginal bleeding, birth defects, spontaneous abortions and fetal death following use in pregnancy. Tamoxifen use during pregnancy may have a potential long-term risk to the fetus of a diethylstilbestrol (DES)-like syndrome (based on animal data).
Tamoxifen may induce ovulation (Steiner 2005) or cause menstrual cycle irregularities. Based on animal data, tamoxifen may impair embryo implantation in females of reproductive potential, but may not reliably cause infertility, even if menstrual cycles are irregular.
Confirm a negative pregnancy test in females of reproductive potential prior to initiating tamoxifen therapy. Females of reproductive potential should use effective nonhormonal contraception during tamoxifen therapy and for 2 months following the last tamoxifen dose.
Patient Education
What is this drug used for?
- It is used to treat breast cancer.
- It is used to lower the chance of breast cancer in women with a higher chance of getting it. It may lower the chance of getting cancer in the other breast after one has cancer.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Hot flashes
- Nausea
- Vomiting
- Weight loss
- Constipation
- Diarrhea
- Trouble sleeping
- Anxiety
- Weight gain
- Back pain
- Bone pain
- Dizziness
- Muscle pain
- Joint pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- High calcium like weakness, confusion, fatigue, headache, nausea and vomiting, constipation, or bone pain.
- Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain.
- Severe cerebrovascular disease like change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes.
- Bruising
- Bleeding
- Severe loss of strength and energy
- Swelling of arms or legs
- Burning or numbness feeling
- Pelvic pain or pressure
- Menstrual changes
- No menstrual periods
- Abnormal vaginal bleeding
- Vaginal discharge
- Vision changes
- Lump in breast
- Breast soreness or pain
- Decreased sex drive
- Sexual dysfunction
- Depression
- Skin changes
- Severe headache
- Painful urination
- Blood clots like numbness or weakness on one side of the body; pain, redness, tenderness, warmth, or swelling in the arms or legs; change in color of an arm or leg; chest pain; shortness of breath; fast heartbeat; or coughing up blood.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.