Boxed Warning
Pregnancy:
If thalidomide is taken during pregnancy, it may cause severe birth defects or embryo-fetal death. Thalidomide should never be used by females who are pregnant or who could become pregnant while taking thalidomide. Even a single dose (1 capsule [regardless of strength]) taken by a pregnant woman during pregnancy may cause severe birth defects.
Because of this toxicity and in an effort to make the chance of embryo-fetal exposure to thalidomide as negligible as possible, thalidomide is approved for marketing only through a special restricted distribution program: Thalomid REMS program, approved by the Food and Drug Administration. Information about Thalomid and the Thalomid REMS program is available at https://www.celgeneriskmanagement.com or by calling the manufacturer's toll-free number 1-888-423-5436.
Thromboembolic events:
The use of thalidomide in multiple myeloma results in an increased risk of venous thromboembolism, such as deep venous thrombosis and pulmonary embolism. This risk increases significantly when thalidomide is used in combination with standard chemotherapeutic agents including dexamethasone. In 1 controlled trial, the rate of venous thromboembolism was 22.5% in patients receiving thalidomide in combination with dexamethasone compared with 4.9% in patients receiving dexamethasone alone (P = 0.002). Patients and physicians are advised to be observant for the signs and symptoms of thromboembolism. Instruct patients to seek medical care if they develop symptoms such as shortness of breath, chest pain, or arm or leg swelling. Consider thromboprophylaxis based on an assessment of individual patients' underlying risk factors.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Thalomid: 50 mg, 100 mg
Thalomid: 150 mg, 200 mg [contains fd&c blue #2 (indigotine)]
Pharmacology
Mechanism of Action
Thalidomide exhibits immunomodulatory and antiangiogenic characteristics; immunologic effects may vary based on conditions. Thalidomide may suppress excessive tumor necrosis factor-alpha production in patients with erythema nodosum leprosum, yet may increase plasma tumor necrosis factor-alpha levels in HIV-positive patients. In multiple myeloma, thalidomide is associated with an increase in natural killer cells and increased levels of interleukin-2 and interferon gamma. Other proposed mechanisms of action include suppression of angiogenesis, prevention of free-radical-mediated DNA damage, increased cell mediated cytotoxic effects, and altered expression of cellular adhesion molecules.
Pharmacokinetics/Pharmacodynamics
Absorption
Slow, good
Distribution
Vd: 1.1 L/kg
Metabolism
Minimal (unchanged drug is the predominant circulating component)
Excretion
Urine (~92%; <4% of the dose as unchanged drug); feces (<2%)
Time to Peak
Plasma: ~2 to 5 hours
Half-Life Elimination
5.5 to 7.3 hours
Protein Binding
55% to 66%
Use in Specific Populations
Special Populations Note
Hansen disease:
Based on data from a small study, in relation to healthy subjects, patients with Hansen disease may have increased thalidomide bioavailability, manifested as increased area under the curve and peak plasma levels.
Use: Labeled Indications
Erythema nodosum leprosum: Acute treatment of cutaneous manifestations of moderate to severe erythema nodosum leprosum; maintenance treatment for prevention and suppression of cutaneous manifestations of erythema nodosum leprosum recurrence
Limitation of use: Thalidomide is not indicated as monotherapy for erythema nodosum leprosum treatment in the presence of moderate to severe neuritis.
Multiple myeloma: Treatment of newly diagnosed multiple myeloma (in combination with dexamethasone)
Use: Off Label
AIDS-related aphthous stomatitisa
Data from a double-blind, randomized, placebo-controlled trial in HIV-infected patients with oral aphthous ulcers support the use of thalidomide for this condition Jacobson 1997.
Chronic graft-versus-host disease, refractorybyes
Data from 2 trials evaluating the use of thalidomide for the treatment of patients with high-risk or refractory chronic graft-versus-host disease (GVHD) suggest that thalidomide may be beneficial for the treatment of this condition Parker 1995, Vogelsang 1992. Data from a prospective trial evaluating patients with refractory acute or chronic GVHD support the use of thalidomide in the treatment of chronic GVHD; no activity was seen in patients with acute GVHD Kulkarni 2003.
Based on the American Society for Blood and Marrow Transplant Consensus Conference on Clinical Practice in Chronic GVHD: Second-Line Treatment of Chronic Graft-versus-Host Disease, thalidomide is an effective and suitable second-line treatment for this condition.
Multiple myeloma, maintenancea
Data from a large, randomized, phase 3 trial and a retrospective analysis support the use of thalidomide for maintenance therapy after autologous stem cell transplantation Brinker 2006, Spencer 2009.
Multiple myeloma, salvagea
Multiple clinical studies have supported the use of thalidomide (alone or in combination with dexamethasone or other cytotoxic chemotherapy) in the treatment of relapsed/refractory multiple myeloma Garderet 2012, Lee 2003, Palumbo 2001, Singhal 1999.
Systemic light chain amyloidosisc
Data from a trial evaluating the use of thalidomide in patients with advanced systemic light chain amyloidosis suggest that thalidomide may be beneficial for the treatment of this condition Wechalekar 2007.
Waldenström macroglobulinemiac
Data from a phase 2 study in patients with symptomatic Waldenström macroglobulinemia suggest that thalidomide may be beneficial in the treatment of this condition Treon 2008.
Contraindications
Hypersensitivity to thalidomide or any component of the formulation; pregnancy
Canadian labeling: Additional contraindications (not in the US labeling): Hypersensitivity to lenalidomide or pomalidomide; females at risk of becoming pregnant and male patients who are unable to follow or comply with conditions for use (refer to manufacturer labeling); breastfeeding
Dosage and Administration
Dosing: Adult
AIDS-related aphthous stomatitis (off-label use): Oral: 200 mg once daily at bedtime for up to 8 weeks; if no response, then 200 mg twice daily for 4 weeks (Jacobson 1997).
Chronic graft-versus-host disease (refractory), treatment (off-label, second-line use; optimum dose not determined): Oral: Initial: 100 mg once daily at bedtime, with dose escalation up to 400 mg daily in 3 to 4 divided doses (Wolff 2011) or Initial: 50 to 100 mg 3 times daily; maximum dose: 600 to 1,200 mg daily (Kulkarni 2003) or 200 mg 4 times daily (dose adjusted to goal thalidomide concentration of ≥5 mcg/mL 2 hours postdose) (Vogelsang 1992) or 100 to 300 mg 4 times daily (Parker 1995).
Erythema nodosum leprosum, acute cutaneous: Oral: Initial: 100 to 300 mg once daily at bedtime, continue until signs/symptoms subside (usually ~2 weeks), then taper off in 50 mg decrements every 2 to 4 weeks. For severe cases with moderate to severe neuritis, corticosteroids may be initiated with thalidomide (taper off and discontinue corticosteroids when neuritis improves).
Patients weighing <50 kg: Initiate at lower end of the dosing range.
Severe cutaneous reaction or patients previously requiring high doses: May be initiated at up to 400 mg once daily at bedtime or in divided doses.
Erythema nodosum leprosum, maintenance (prevention/suppression, or with flares during tapering attempts): Oral: Maintain on the minimum dosage necessary to control the reaction; efforts to taper off should be attempted every 3 to 6 months, in decrements of 50 mg every 2 to 4 weeks.
Multiple myeloma, newly diagnosed: Oral: 200 mg once daily at bedtime (in combination with dexamethasone).
Multiple myeloma (off-label dosing or combinations):
In combination with bortezomib and dexamethasone (off-label combination): Induction therapy: 100 mg once daily for the first 14 days, then 200 mg once daily for 3 (21-day) cycles (Cavo 2010) or 100 mg once daily for up to 8 (21-day) cycles (Kaufman 2010).
In combination with daratumumab, bortezomib, and dexamethasone (off-label combination): DVTd regimen (in newly diagnosed transplant-eligible patients): 100 mg once daily for up to 4 pretransplant induction cycles and 2 posttransplant consolidation cycles; each cycle is 28 days (Moreau 2019).
In combination with melphalan and prednisone (off-label combination): 200 to 400 mg once daily (Facon 2007) or 100 mg once daily (Palumbo 2008) or 50 to 100 mg once daily, depending on patient tolerance (Hulin 2009).
Multiple myeloma, maintenance (following autologous stem cell transplant; off-label use): Oral: 200 mg once daily starting 3 to 6 months after transplant; continue until disease progression or unacceptable toxicity (Brinker 2006) or 100 mg once daily starting 42 to 60 days following transplant; increase to 200 mg once daily after 2 weeks if tolerated; continue for up to 12 months (in combination with prednisolone) (Spencer 2009).
Multiple myeloma, salvage therapy: Initial: 200 mg once daily at bedtime; may increase daily dose by 200 mg every 2 weeks for 6 weeks (if tolerated) to a maximum of 800 mg once daily at bedtime (Singhal 1999) or 100 mg once daily (in combination with dexamethasone) (Palumbo 2001) or 200 mg once daily (in combination with bortezomib and dexamethasone) for 1 year (Garderet 2012) or 400 mg once daily at bedtime (in combination with dexamethasone, cisplatin, doxorubicin, cyclophosphamide and etoposide) (Lee 2003).
Systemic light chain amyloidosis (off-label use): Oral: 200 mg once daily (starting dose 50 to 100 mg once daily; titrate at 4-week intervals) in combination with cyclophosphamide and dexamethasone (Wechalekar 2007).
Waldenström macroglobulinemia (off-label use): Oral: ≤200 mg once daily for up to 52 weeks (in combination with rituximab) (Treon 2008).
Dosing: Geriatric
Refer to adult dosing. A reduced initial dose may be appropriate (depending on patient tolerance) in patients ≥75 years (Hulin 2009).
Dosing: Pediatric
AIDS-related aphthous stomatitis: Limited data available: Adolescents ≥13 years: Oral: 200 mg once daily at bedtime for 4 weeks or sooner if resolution. May be increased to 200 mg twice daily if no improvement after 4 weeks. Dosing based on double-blind, placebo-controlled trial by AIDS Clinical Trials Group (n=57, age: ≥13 years) which showed 55% healing in treatment group vs 7% in placebo (Jacobson 1997).
Chronic graft-versus-host disease (refractory), treatment: Limited data available: Children ≥2 years and Adolescents: Oral: Initial: 3 to 6 mg/kg/day (maximum initial daily dose: 100 mg/day) at bedtime or in 2 to 4 divided doses before meals; may be adjusted at ≥2 week intervals based on patient response up to 12 mg/kg/day in 3 to 4 divided doses (maximum daily dose: 800 mg/day) (Browne 2000; Rovelli 1998; Wolff 2011); one trial using initial doses of 3 mg/kg/dose every 6 hours (dose adjusted to attain goal thalidomide concentration of ≥5 mcg/mL 2 hours postdose) (Vogelsang 1992)
Crohn's disease/ulcerative colitis (refractory), treatment: Limited data available: Children ≥1 year and Adolescents: Oral: 0.5 to 3 mg/kg/day (maximum daily dose: 300 mg/day), usually dosed once daily in the evening; titrate to lowest effective dose after remission is achieved (Facchini 2001; Lazzerini 2007; Martelossi 2004; Zheng 2011)
Erythema nodosum leprosum (ENL), cutaneous: Children ≥12 years and Adolescents: Oral:
Acute: Initial: 100 to 300 mg once daily at bedtime; continue until signs/symptoms subside (usually ~2 weeks), then taper off in 50 mg decrements every 2 to 4 weeks. For severe cases with moderate to severe neuritis, corticosteroids may be initiated with thalidomide (taper off and discontinue corticosteroids when neuritis improves).
Patients weighing <50 kg: Initiate at lower end of dosage range
Severe cutaneous reaction or patients previously requiring high doses: May be initiated or increased to 400 mg/day at bedtime or in divided doses
Maintenance (prevention/suppression, or with flares during tapering attempts): Maintain on the minimum dosage necessary to control the reaction; efforts to taper should be repeated every 3 to 6 months, in decrements of 50 mg every 2 to 4 weeks
Systemic juvenile idiopathic arthritis (SJIA): Limited data available: Children ≥3 years and Adolescents: Oral: Initial 2 mg/kg/day, if necessary may increase at 2-week intervals to 3 to 5 mg/kg/day. Data based on a multicenter, open-labeled prospective study (n=13, age: 3 to 23 years); within 4 weeks, 11 of 13 patients showed improvement in JRA scores, significant decreases in ESR, and significant increase in hemoglobin (Lehman 2004)
Dosing adjustment for toxicity: Children and Adolescents: ANC ≤750/mm3: Withhold treatment if clinically appropriate
For other observed toxicities, the following have been used in adult patients with multiple myeloma:
Constipation, oversedation: Temporarily withhold or continue with a reduced dose
Peripheral neuropathy: The manufacturer recommends to temporarily withhold or continue with a reduced dose. The following adjustments have also been recommended (Richardson 2012):
Grade 1: Reduce dose by 50%
Grade 2: Temporarily interrupt therapy; once resolved to ≤ grade 1, resume therapy with a 50% dosage reduction (if clinically appropriate)
Grade 3 or higher: Discontinue therapy
Dosing: Adjustment for Toxicity
ANC ≤750/mm3: Withhold treatment if clinically appropriate.
Dermatologic reactions:
Grade 2 or 3 rash: Consider interruption or discontinuation of therapy.
Grade 4 rash, skin exfoliation, bullae, or any severe dermatologic reaction: Permanently discontinue therapy.
Grade 3 or 4 adverse reactions: Consider dose reduction, delay or discontinuation (based on clinical judgment).
Other reactions:
Angioedema or anaphylaxis: Permanently discontinue therapy.
Constipation, oversedation: Temporarily withhold and consider a reduced dose with resumption of therapy.
Peripheral neuropathy:
The manufacturer recommends to temporarily withhold and consider a reduced dose with resumption of therapy.
The following adjustments have also been recommended (Richardson 2012):
Grade 1: Reduce dose by 50%.
Grade 2: Temporarily interrupt therapy; once resolved to ≤ grade 1, resume therapy with a 50% dosage reduction (if clinically appropriate).
Grade 3 or higher: Discontinue therapy.
Extemporaneously Prepared
A 20 mg/mL oral suspension may be prepared with capsules and a 1:1 mixture of Ora-Sweet and Ora-Plus. Empty the contents of twelve 100 mg capsules into a glass mortar. Add small portions of the vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 60 mL; transfer to an amber calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 60 mL. Label “shake well,” “protect from light,” and “refrigerate”. Stable for 35 days refrigerated.
Kraft S, Johnson CE, and Tyler RP, "Stability of an Extemporaneously Prepared Thalidomide Suspension," Am J Health Syst Pharm, 2011, 69(1):56-8.22180553
Administration
Administer orally, preferably at bedtime once daily, at least 1 hour after the evening meal. Doses >400 mg/day may be given in divided doses at least 1 hour after meals. Swallow capsules whole with water. Capsules should not be opened or crushed.
Capsules should remain in blister pack until ingestion. If exposed to the powder content from broken capsules or body fluids from patients receiving thalidomide, the exposed area should be washed immediately and thoroughly with soap and water.
Missed doses: For missed doses, if <12 hours patient may receive dose; if >12 hours wait until next dose due.
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Protect from light. Keep in original package.
Drug Interactions
Abatacept: Anti-TNF Agents may enhance the adverse/toxic effect of Abatacept. An increased risk of serious infection during concomitant use has been reported. Avoid combination
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Anakinra: Anti-TNF Agents may enhance the adverse/toxic effect of Anakinra. An increased risk of serious infection during concomitant use has been reported. Avoid combination
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bisphosphonate Derivatives: Angiogenesis Inhibitors (Systemic) may enhance the adverse/toxic effect of Bisphosphonate Derivatives. Specifically, the risk for osteonecrosis of the jaw may be increased. Monitor therapy
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Canakinumab: Anti-TNF Agents may enhance the adverse/toxic effect of Canakinumab. Specifically, the risk for serious infections and/or neutropenia may be increased. Avoid combination
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Certolizumab Pegol: Anti-TNF Agents may enhance the immunosuppressive effect of Certolizumab Pegol. Avoid combination
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
CNS Depressants: May enhance the CNS depressant effect of Thalidomide. Avoid combination
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
DexAMETHasone (Systemic): May enhance the dermatologic adverse effect of Thalidomide. DexAMETHasone (Systemic) may enhance the thrombogenic effect of Thalidomide. Consider therapy modification
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Erythropoiesis-Stimulating Agents: May enhance the thrombogenic effect of Thalidomide. Monitor therapy
Estrogen Derivatives: May enhance the thrombogenic effect of Thalidomide. Monitor therapy
Estrogen Derivatives (Contraceptive): May enhance the thrombogenic effect of Thalidomide. Monitor therapy
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Pamidronate: Thalidomide may enhance the nephrotoxic effect of Pamidronate. Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Pembrolizumab: May enhance the adverse/toxic effect of Thalidomide Analogues. Specifically, mortality may be increased when this combination is used for treatment of refractory multiple myeloma. Avoid combination
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Progestins (Contraceptive): May enhance the thrombogenic effect of Thalidomide. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Rilonacept: Anti-TNF Agents may enhance the adverse/toxic effect of Rilonacept. Avoid combination
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tocilizumab: May enhance the immunosuppressive effect of Anti-TNF Agents. Avoid combination
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Vedolizumab: Anti-TNF Agents may enhance the adverse/toxic effect of Vedolizumab. Avoid combination
Zoledronic Acid: Thalidomide may enhance the adverse/toxic effect of Zoledronic Acid. Monitor therapy
Adverse Reactions
Incidences of adverse reactions may include combination therapy.
>10%: Central nervous system: Drowsiness (≤38%), headache (≤13%), peripheral neuropathy (≥10%)
1% to 10%:
Cardiovascular: Facial edema (≤4%), peripheral edema (≤4%)
Central nervous system: Malaise (≤8%), pain (≤8%), vertigo (≤8%), dizziness (≤4%)
Dermatologic: Pruritus (≤8%), fungal dermatitis (≤4%), maculopapular rash (≤4%), nail disease (≤4%)
Gastrointestinal: Constipation (≤4%), nausea (≤4%), oral candidiasis (≤4%), toothache (≤4%)
Genitourinary: Impotence (≤8%)
Neuromuscular & skeletal: Weakness (≤8%), back pain (≤4%), neck pain (≤4%), neck stiffness (≤4%), tremor (≤4%)
Miscellaneous: Accidental injury (≤4%)
<1%, postmarketing, and/or case reports: Acute renal failure, amenorrhea, aphthous stomatitis, auditory impairment, biliary obstruction, bradycardia, carpal tunnel syndrome, cerebrovascular accident, change in prothrombin time, chronic myelocytic leukemia, cytomegalovirus disease, diplopia, ECG abnormality, erythema multiforme, erythema nodosum, erythroleukemia, febrile neutropenia, foot-drop, galactorrhea, gastric ulcer, gynecomastia, hangover effect, Hodgkin lymphoma, hypercalcemia, hypersensitivity reaction, hypomagnesemia, hyponatremia, hypothyroidism, increased serum alkaline phosphatase, interstitial pulmonary disease, intestinal perforation, lethargy, loss of consciousness, lymphedema, lymphocytopenia, mental status changes, migraine, myocardial infarction, myxedema, neutropenia, nystagmus, oliguria, orthostatic hypotension, pancytopenia, Parkinson disease, petechia, pleural effusion, pulmonary embolism, pulmonary hypertension, purpura, Raynaud phenomenon, reactivation of HBV, renal failure, seizure, sepsis, septic shock, sexual disorder, sick sinus syndrome, status epilepticus, Stevens-Johnson syndrome, stupor, suicidal tendencies, syncope, thrombocytopenia, tonic-clonic seizures, toxic epidermal necrolysis, tumor lysis syndrome, urinary incontinence, uterine hemorrhage, varicella zoster infection
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: May cause leukopenia and neutropenia; avoid initiating therapy if ANC <750/mm3. Persistent neutropenia may require treatment interruption. Thrombocytopenia (including grades 3 and 4) has been reported; may require dose reduction, treatment delay, or discontinuation. Monitor for signs and symptoms of bleeding (including petechiae, epistaxis, and GI bleeding), especially if concomitant medication may increase the risk of bleeding. Monitor CBC with differential and platelets. Anemia has also been observed.
- Bradycardia: May cause bradycardia; use with caution when administering concomitantly with medications that may also decrease heart rate. May require thalidomide dose reduction or discontinuation.
- CNS effects: May cause dizziness, drowsiness, and/or somnolence; caution patients about performing tasks which require mental alertness (eg, operating machinery or driving). Avoid ethanol and concomitant medications that may exacerbate these symptoms; dose reductions may be necessary for excessive drowsiness or somnolence.
- Constipation: Constipation may commonly occur. May require treatment interruption or dosage reduction.
- Dermatologic reactions: Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and drug reaction with eosinophilia and systemic symptoms (DRESS) have been reported (may be fatal). Withhold or discontinue therapy for grade 2 or 3 rash. Permanently discontinue for grade 4 rash or if rash is exfoliative, bullous, or severe (eg, SJS, TEN, DRESS).
- Hepatotoxicity: Abnormal liver function tests, hepatitis, and cholestatic jaundice have been reported. Hepatotoxicity (including hepatocellular and cholestatic injury) has been observed rarely (case reports), with a mean time to development of 46 days; most events resolved after discontinuing thalidomide (Vilas-Boas 2012).
- Hypersensitivity: Hypersensitivity, including angioedema, anaphylactic reaction, and erythematous macular rash, possibly associated with fever, tachycardia, and hypotension, have been reported. Permanently discontinue for angioedema or anaphylaxis. May require treatment interruption for other severe reactions; discontinue if recurs with rechallenge.
- Orthostatic hypotension: May cause orthostatic hypotension; use with caution in patients who would not tolerate transient hypotensive episodes. When arising from a recumbent position, advise patients to sit upright for a few minutes prior to standing.
- Peripheral neuropathy: Thalidomide is commonly associated with peripheral neuropathy; may be irreversible. Neuropathy generally occurs following chronic use (over months), but may occur with short-term use; onset may be delayed. Use caution with other medications that may also cause peripheral neuropathy. Monitor for signs/symptoms of neuropathy monthly for the first 3 months of therapy and regularly thereafter. Electrophysiological testing may be considered at baseline and every 6 months to detect asymptomatic neuropathy. To limit further damage, immediately discontinue (if clinically appropriate) in patients who develop neuropathy. Reinitiate therapy only if neuropathy returns to baseline; may require dosage reduction or permanent discontinuation.
- Secondary malignancy: Increased incidence of second primary malignancies (SPMs), including acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS), has been observed in previously untreated multiple myeloma patients receiving thalidomide in combination with melphalan, and prednisone. In addition to AML and MDS, solid tumors have been reported with thalidomide maintenance treatment for multiple myeloma (Usmani 2012). Carefully evaluate patients for SPMs prior to and during treatment and manage as clinically indicated.
- Seizures: Seizures (including grand mal convulsions) have been reported in postmarketing data; monitor closely for clinical changes indicating potential seizure activity in patients with a history of seizures, concurrent therapy with drugs that alter seizure threshold, or conditions that predispose to seizures.
- Thromboembolic events: [US Boxed Warning]: Thalidomide use for the treatment of multiple myeloma is associated with an increased risk for venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE); the risk is increased when used in combination with standard chemotherapy agents, including dexamethasone. In one controlled study, the incidence of VTE was 22.5% in patients receiving thalidomide in combination with dexamethasone, compared to 4.9% for dexamethasone alone. Monitor for signs and symptoms of thromboembolism (shortness of breath, chest pain, or arm or leg swelling) and instruct patients to seek prompt medical attention with development of these symptoms. Consider thromboprophylaxis based on risk factors. Ischemic heart disease, including MI and stroke, also occurred at a higher rate (compared to placebo) in myeloma patients receiving thalidomide plus dexamethasone who had not received prior treatment. Assess individual risk factors for thromboembolism and consider thromboprophylaxis. The American Society of Clinical Oncology guidelines for VTE prophylaxis and treatment recommend thromboprophylaxis for patients receiving thalidomide in combination with chemotherapy and/or dexamethasone; either aspirin or low molecular weight heparin (LMWH) is recommended for lower risk patient and LMWH is recommended for higher-risk patients (Lyman 2013; Lyman 2015). Anticoagulant prophylaxis should be individualized and selected based on the venous thromboembolism risk of the combination treatment regimen, using the safest and easiest to administer (Palumbo 2008). Monitor for signs/symptoms of thromboembolism and advise patients to seek immediate care if symptoms (shortness of breath, chest pain, arm/leg swelling) develop. Other medications that are also associated with thromboembolism should be used with caution.
- Tumor lysis syndrome: Patients with a high tumor burden may be at risk for tumor lysis syndrome; monitor closely; institute appropriate management for hyperuricemia.
Disease-related concerns:
- Heart failure: In a scientific statement from the American Heart Association, thalidomide has been determined to be an agent that may exacerbate underlying myocardial dysfunction (magnitude: minor) (AHA [Page 2016]).
- Multiple myeloma: An increase in mortality was noted in 2 clinical studies in patients with multiple myeloma who received pembrolizumab in combination with a thalidomide analogue and dexamethasone. Causes of death in the experimental arm (containing pembrolizumab, dexamethasone, and a thalidomide analogue [pomalidomide or lenalidomide]) included myocarditis, SJS, MI, pericardial hemorrhage, cardiac failure, respiratory tract infection, neutropenic sepsis, sepsis, multiple organ dysfunction, respiratory failure, intestinal ischemia, cardiopulmonary arrest, suicide, pulmonary embolism, cardiac arrest, pneumonia, sudden death, and large intestine perforation. Multiple myeloma is not an approved indication for PD-1 or PD-L1 blocking antibodies; pembrolizumab should not be used to treat multiple myeloma in combination with a thalidomide analogue and dexamethasone unless as part of a clinical trial.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Certain adverse reactions (constipation, fatigue, weakness, nausea, hypokalemia, hyperglycemia, DVT, pulmonary embolism, atrial fibrillation) are more likely in elderly patients.
- HIV-infected patients: Thalidomide is associated with increased viral loads in studies conducted prior to the use of antiretroviral therapy. Monitor viral load after the first and third months of therapy, and every 3 months thereafter.
- Pregnancy: [US Boxed Warning]: Thalidomide is contraindicated in pregnant females. Thalidomide may cause severe birth defects or embryo-fetal death if taken during pregnancy. Thalidomide cannot be used in females who are pregnant or may become pregnant during therapy as even a single dose may cause severe birth defects. In order to decrease the risk of fetal exposure, thalidomide is available only through a special restricted distribution program (Thalomid REMS). Use is also contraindicated in females who may become pregnant. Pregnancy must be excluded prior to therapy initiation with 2 negative pregnancy tests. Females of reproductive potential must avoid pregnancy beginning 4 weeks prior to therapy, during therapy, during therapy interruptions, and for ≥4 weeks after therapy is discontinued; 2 reliable methods of birth control, or abstinence from heterosexual intercourse, must be used. Males taking thalidomide (even those vasectomized) must use a latex or synthetic condom during any sexual contact with females of childbearing potential and for up to 28 days following discontinuation of therapy. Males taking thalidomide must not donate sperm. Some forms of contraception may not be appropriate in certain patients. An intrauterine device or implantable contraceptive may increase the risk of infection or bleeding; estrogen-containing products may increase the risk of thromboembolism.
Other warnings/precautions:
- Blood donation: Patients should not donate blood during thalidomide treatment and for 4 weeks after therapy discontinuation.
- REMS program: Due to the embryo-fetal risk, thalidomide is only available through a restricted program under the Thalomid REMS program. Prescribers and pharmacies must be certified with the program to prescribe or dispense thalidomide. Patients must sign an agreement and comply with the REMS program requirements.
Monitoring Parameters
CBC with differential, platelets; thyroid function tests (TSH at baseline then every 2 to 3 months during thalidomide treatment [Hamnvik 2011]). Hepatic function tests (periodic; particularly with preexisting hepatic dysfunction or concomitant use of drugs associated with hepatotoxicity). In HIV-seropositive patients: viral load after 1 and 3 months, then every 3 months. Pregnancy testing (sensitivity of at least 50 milliunits/mL) is required 10 to 14 days prior to therapy, within 24 hours prior to initiation of therapy, weekly during the first 4 weeks, then every 4 weeks in females with regular menstrual cycles or every 2 weeks in females with irregular menstrual cycles. Signs of neuropathy monthly for the first 3 months, then periodically during treatment; consider monitoring of sensory nerve application potential amplitudes (at baseline and every 6 months) to detect asymptomatic neuropathy. Monitor for signs and symptoms of thromboembolism (shortness of breath, chest pain, arm/leg swelling), tumor lysis syndrome, bradycardia, and syncope; monitor for clinical changes indicating potential seizure activity (in patients with a history of seizure). Monitor adherence.
Pregnancy
Pregnancy Considerations
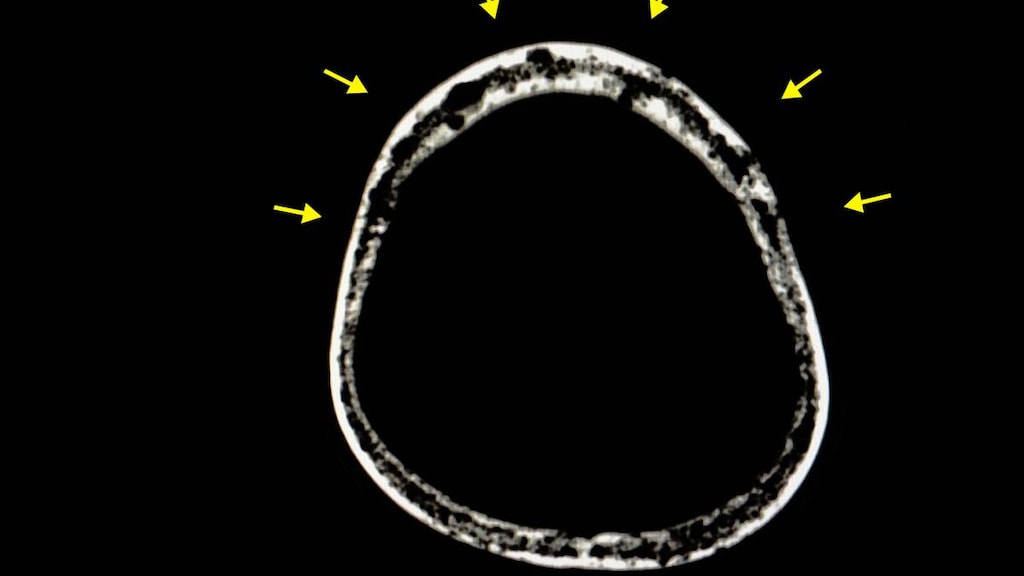
Use is contraindicated in pregnant females. [US Boxed Warning]: If thalidomide is taken during pregnancy, it can cause severe birth defects or embryo-fetal death. Thalidomide should never be used by females who are pregnant or who could become pregnant while taking thalidomide. Even a single dose (1 capsule [regardless of strength]) taken by a pregnant woman during pregnancy may cause severe birth defects. Thalidomide induces a high frequency of severe and life-threatening birth defects. Anomalies observed in humans include amelia, phocomelia, bone defects, ear and eye abnormalities, facial palsy, congenital heart defects, urinary and genital tract malformations; mortality in ~40% of infants at or shortly after birth has also been reported. Discontinue thalidomide immediately if pregnancy occurs during treatment and refer patient to a reproductive toxicity specialist.
When alternative treatments are not available, females of reproductive potential may be treated when adequate precautions are taken to avoid pregnancy. [US Boxed Warning]: In an effort to make the chance of embryo-fetal exposure to thalidomide as negligible as possible, thalidomide is approved for marketing only through a special restricted distribution program: Thalomid REMS program, approved by the Food and Drug Administration. Information about Thalomid and the Thalomid REMS program is available at https://www.celgeneriskmanagement.com or by calling the manufacturer's toll-free number 1-888-423-5436. Females of reproductive potential must avoid pregnancy beginning 4 weeks prior to therapy, during therapy, during therapy interruptions, and for ≥4 weeks after therapy is discontinued. A negative pregnancy test (sensitivity of ≥50 milliunits/mL) 10 to 14 days prior to therapy, within 24 hours prior to beginning therapy, weekly during the first 4 weeks, and every 4 weeks (every 2 weeks for females with irregular menstrual cycles) thereafter is required for women of childbearing potential. Two forms of reliable contraception must be used simultaneously in females of reproductive potential (unless they commit to total abstinence from heterosexual intercourse): One highly effective method (eg, tubal ligation, IUD, hormonal birth control methods) or partner’s vasectomy; plus one additional effective method (eg, male latex or synthetic condom, diaphragm, or cervical cap). Contraception is required even in cases of infertility (unless due to hysterectomy). Thalidomide must be immediately discontinued for a missed period, abnormal pregnancy test, or abnormal menstrual bleeding; refer patient to a reproductive toxicity specialist if pregnancy occurs during treatment.
Females of reproductive potential (including health care workers and caregivers) must also avoid contact with thalidomide capsules.
Thalidomide is also present in the semen of males. Males taking thalidomide (even those vasectomized) must use a latex or synthetic condom during any sexual contact with women of childbearing potential and for up to 28 days following discontinuation of therapy. Males taking thalidomide must not donate sperm.
A pregnancy exposure registry has been created to monitor outcomes in females exposed to thalidomide during pregnancy and female partners of male patients and to understand the root cause for the pregnancy. The pregnancy exposure registry may be contacted at 1-888-423-5436. If pregnancy occurs during treatment, thalidomide must be immediately discontinued and the patient referred to a reproductive toxicity specialist. Any suspected fetal exposure to thalidomide must be reported to the FDA via the MedWatch program (1-800-FDA-1088) and to Celgene Corporation (1-888-423-5436).
Patient Education
What is this drug used for?
- It is used to treat multiple myeloma.
- It is used to treat skin signs of leprosy.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Constipation
- Headache
- Lack of appetite
- Nausea
- Dry mouth
- Dry skin
- Fatigue
- Anxiety
- Tremors
- Weight gain or loss
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding
- Low calcium like muscle cramps or spasms, numbness and tingling, or seizures
- Blood clots like numbness or weakness on one side of the body; pain, redness, tenderness, warmth, or swelling in the arms or legs; change in color of an arm or leg; chest pain; shortness of breath; fast heartbeat; or coughing up blood
- Burning or numbness feeling
- Seizures
- Severe dizziness
- Passing out
- Fast heartbeat
- Slow heartbeat
- Severe loss of strength and energy
- Swelling
- Swollen glands
- Tumor lysis syndrome like fast heartbeat or abnormal heartbeat; any passing out; unable to pass urine; muscle weakness or cramps; nausea, vomiting, diarrhea or lack of appetite; or feeling sluggish
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Heart attack like chest pain; pain in arms, back, neck, jaw, or abdomen; shortness of breath; cold sweats; severe dizziness; passing out; severe nausea; or vomiting
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or vision changes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.