Boxed Warning
Proarrhythmic effects:
Thioridazine has been shown to prolong the QTc interval in a dose-related manner. Drugs with this potential, including thioridazine, have been associated with torsades de pointes–type arrhythmias and sudden death. Because of its potential for significant, possibly life-threatening, proarrhythmic effects, reserve thioridazine use for the treatment of schizophrenic patients who fail to show an acceptable response to adequate courses of treatment with other antipsychotic drugs, either because of insufficient effectiveness or the inability to achieve an effective dose because of intolerable adverse effects from those drugs.
Increased mortality in elderly patients with dementia-related psychosis:
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of 17 placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 and 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was approximately 4.5% compared with a rate of approximately 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (eg, heart failure, sudden death) or infectious (eg, pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. Thioridazine is not approved for the treatment of patients with dementia-related psychosis.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
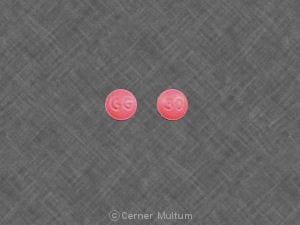
Tablet, Oral, as hydrochloride:
Generic: 10 mg, 25 mg, 50 mg, 100 mg
Pharmacology
Mechanism of Action
Thioridazine is a piperidine phenothiazine which blocks postsynaptic mesolimbic dopaminergic receptors in the brain; also has activity at serotonin, noradrenaline, and histamine receptors (Fenton, 2007).
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid (Vanderheeren 1977)
Distribution
Vd: 1.8 to 6.7 L/kg (Vanderheeren 1977)
Metabolism
Hepatic metabolism by sulphoxidation (primarily), demethylation (2%), and hydroxylation (limited); active metabolites mesoridazine and sulphoridazine (Vanderheeren 1977).
Time to Peak
Serum: ~1 to 4 hours (Mårtensson 1973)
Half-Life Elimination
5 to 27 hours (Mårtensson 1973; Muusze 1977; Vanderheeren 1977)
Protein Binding
96% to 99.3% (Cooper, 1978)
Use: Labeled Indications
Schizophrenia: Treatment of patients with schizophrenia who fail to respond adequately to treatment with other antipsychotic drugs, either because of insufficient effectiveness or the inability to achieve an effective dose because of intolerable adverse effects from those medications. Before initiating treatment with thioridazine, it is strongly recommended that a patient be given at least 2 trials, each with a different antipsychotic drug product, at an adequate dose and for an adequate duration.
Contraindications
Severe CNS depression; severe hyper-/hypotensive heart disease; coma; in combination with other drugs that are known to prolong the QTc interval, CYP2D6 inhibitors (fluoxetine, paroxetine), and/or fluvoxamine, propranolol, or pindolol; in patients with congenital long QT syndrome or a history of cardiac arrhythmias; patients known to have genetic defect leading to reduced levels of activity of CYP2D6
Dosage and Administration
Dosing: Adult
Schizophrenia: Oral: Initial: 50 to 100 mg 3 times daily; dosage may be increased at gradual increments based on response and tolerability; usual dosage: 300 to 800 mg/day in 2 to 4 divided doses (APA [Lehman, 2004]); maximum: 800 mg/day.
Discontinuation of therapy: Gradual dose reduction is advised to avoid withdrawal symptoms (ie, insomnia, headache, GI symptoms), unless discontinuation is due to significant adverse effects. When discontinuing chronic antipsychotic therapy in patients with schizophrenia or bipolar disorder, decreasing the dose very gradually over months to years with close monitoring is suggested to allow for detection of prodromal symptoms of disease recurrence (APA [Lehman 2004]; CPA 2005).
Switching antipsychotics: Limited data available; optimal universal strategy is unknown. Strategies include: cross-titration (gradually discontinuing the first antipsychotic while gradually increasing the new antipsychotic) and abrupt change (abruptly discontinuing the first antipsychotic and either increasing the new antipsychotic gradually or starting it at a treatment dose). In patients with schizophrenia at high risk of relapse, the current medication may be maintained at full dose as the new medication is increased (ie, overlap); once the new medication is at therapeutic dose, the first medication is gradually decreased and discontinued over 1 to 2 weeks (Cerovecki 2013; Remington 2005; Takeuchi 2017). Based upon clinical experience, some experts generally prefer cross-titration and overlap approaches rather than abrupt change (Post 2019; Stroup 2019).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: In the management of pediatric patients with schizophrenia or severe behavioral problems, use has generally been replaced by second-generation antipsychotics (AACAP [McClellan 2013])
Schizophrenia, refractory: Note: Before initiating treatment with thioridazine, it is strongly recommended that a patient be given at least 2 trials, each with a different antipsychotic drug product, at an adequate dose and for an adequate duration. Dosage should be individualized; use lowest effective dose and shortest effective duration; periodically reassess the need for continued treatment.
Children ≥6 years and Adolescents: Oral: Initial: 0.5 mg/kg/day in 2 to 3 divided doses; maximum initial dose: 50 mg/dose based on adult experience; gradually titrate to clinical response up to a maximum daily dose: 3 mg/kg/day
Storage
Store at 20°C to 25°C (68°F to 77°F). Protect from light.
Thioridazine Images
Drug Interactions
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Acetylcholinesterase Inhibitors (Central): May enhance the neurotoxic (central) effect of Antipsychotic Agents. Severe extrapyramidal symptoms have occurred in some patients. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Amisulpride: Antipsychotic Agents may enhance the adverse/toxic effect of Amisulpride. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
Amisulpride: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Avoid combination
Amphetamines: Antipsychotic Agents may diminish the stimulatory effect of Amphetamines. Monitor therapy
Amphetamines: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Amphetamines. Monitor therapy
Antacids: May decrease the absorption of Antipsychotic Agents (Phenothiazines). Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Antimalarial Agents: May increase the serum concentration of Antipsychotic Agents (Phenothiazines). Monitor therapy
Anti-Parkinson Agents (Dopamine Agonist): Antipsychotic Agents (First Generation [Typical]) may diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Anti-Parkinson Agents (Dopamine Agonist) may diminish the therapeutic effect of Antipsychotic Agents (First Generation [Typical]). Management: Avoid concomitant therapy if possible and monitor for decreased effects of both agents when these combinations cannot be avoided. Atypical antipsychotics such as clozapine and quetiapine may be less likely to reduce the effects of anti-Parkinson agents. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
ARIPiprazole: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Asunaprevir: May increase the serum concentration of Thioridazine. Avoid combination
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Beta-Blockers: Antipsychotic Agents (Phenothiazines) may enhance the hypotensive effect of Beta-Blockers. Beta-Blockers may decrease the metabolism of Antipsychotic Agents (Phenothiazines). Antipsychotic Agents (Phenothiazines) may decrease the metabolism of Beta-Blockers. Exceptions: Atenolol; Levobunolol; Metipranolol; Nadolol. Monitor therapy
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brexpiprazole: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Brexpiprazole. Management: If brexpiprazole is to be used together with both a moderate CYP2D6 inhibitor and a strong or moderate CYP3A4 inhibitor, the brexpiprazole dose should be reduced to 25% of the usual dose. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromopride: May enhance the adverse/toxic effect of Antipsychotic Agents. Avoid combination
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Ceritinib: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of Antipsychotic Agents (Phenothiazines). Monitor therapy
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Chlorpheniramine: May enhance the arrhythmogenic effect of Thioridazine. Thioridazine may increase the serum concentration of Chlorpheniramine. Management: Avoid this combination when possible. If used, monitor closely for arrhythmia as well as general toxicity of chlorpheniramine. Consider therapy modification
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Clarithromycin: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Clarithromycin. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CloZAPine: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of CloZAPine. Monitor therapy
CloZAPine: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of CloZAPine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Cobicistat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors: May increase the serum concentration of Thioridazine. Avoid combination
CYP2D6 Substrates (High risk with Inhibitors): CYP2D6 Inhibitors (Moderate) may decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Exceptions: Tamoxifen. Monitor therapy
Dapoxetine: May enhance the arrhythmogenic effect of Thioridazine. Dapoxetine may increase the serum concentration of Thioridazine. Avoid combination
Deutetrabenazine: May enhance the adverse/toxic effect of Antipsychotic Agents. Specifically, the risk for akathisia, parkinsonism, or neuroleptic malignant syndrome may be increased. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Domperidone: QT-prolonging Agents (Moderate Risk) may enhance the QTc-prolonging effect of Domperidone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
DOXOrubicin (Conventional): CYP2D6 Inhibitors (Moderate) may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to moderate CYP2D6 inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Dronedarone: Thioridazine may enhance the QTc-prolonging effect of Dronedarone. Avoid combination
Droperidol: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Droperidol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Eliglustat: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Eliglustat. Management: Reduce the eliglustat dose to 84 mg daily. Avoid use of eliglustat in combination with a moderate CYP2D6 inhibitor and a strong or moderate CYP3A4 inhibitor. Consider therapy modification
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Fesoterodine: CYP2D6 Inhibitors may increase serum concentrations of the active metabolite(s) of Fesoterodine. Monitor therapy
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
FLUoxetine: May enhance the QTc-prolonging effect of Thioridazine. FLUoxetine may increase the serum concentration of Thioridazine. Avoid combination
Flupentixol: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Flupentixol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
FluvoxaMINE: May increase the serum concentration of Thioridazine. Avoid combination
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Guanethidine: Antipsychotic Agents may diminish the therapeutic effect of Guanethidine. Monitor therapy
Haloperidol: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Indoramin: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Indoramin. Monitor therapy
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Letermovir: Thioridazine may diminish the therapeutic effect of Letermovir. Avoid combination
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Lithium: May enhance the neurotoxic effect of Antipsychotic Agents. Lithium may decrease the serum concentration of Antipsychotic Agents. Specifically noted with chlorpromazine. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Lumefantrine: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Melatonin: May enhance the adverse/toxic effect of Thioridazine. Monitor therapy
Mequitazine: Antipsychotic Agents may enhance the arrhythmogenic effect of Mequitazine. Management: Consider alternatives to one of these agents when possible. While this combination is not specifically contraindicated, mequitazine labeling describes this combination as discouraged. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Methylphenidate: Antipsychotic Agents may enhance the adverse/toxic effect of Methylphenidate. Methylphenidate may enhance the adverse/toxic effect of Antipsychotic Agents. Monitor therapy
Metoclopramide: May enhance the adverse/toxic effect of Antipsychotic Agents. Avoid combination
Metoprolol: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Metoprolol. Monitor therapy
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
MetyroSINE: May enhance the adverse/toxic effect of Antipsychotic Agents. Monitor therapy
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Moclobemide: May increase the serum concentration of Thioridazine. Avoid combination
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nebivolol: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Nebivolol. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
OLANZapine: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of OLANZapine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Ondansetron: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Pentamidine (Systemic): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pimozide: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Piribedil: Antipsychotic Agents may diminish the therapeutic effect of Piribedil. Piribedil may diminish the therapeutic effect of Antipsychotic Agents. Management: Use of piribedil with antiemetic neuroleptics is contraindicated, and use with antipsychotic neuroleptics, except for clozapine, is not recommended. Avoid combination
Pitolisant: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Pitolisant. Monitor therapy
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
QT-prolonging Agents (Highest Risk): May enhance the QTc-prolonging effect of Thioridazine. Exceptions: Dronedarone; QuiNIDine. Avoid combination
QT-prolonging Antidepressants (Moderate Risk): QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Antidepressants (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Class IC Antiarrhythmics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Kinase Inhibitors (Moderate Risk): QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Miscellaneous Agents (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Domperidone. Monitor therapy
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Quinolone Antibiotics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QUEtiapine: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of QUEtiapine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Quinagolide: Antipsychotic Agents may diminish the therapeutic effect of Quinagolide. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
QuiNIDine: Thioridazine may enhance the QTc-prolonging effect of QuiNIDine. QuiNIDine may increase the serum concentration of Thioridazine. Avoid combination
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
RisperiDONE: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of RisperiDONE. QT-prolonging Antipsychotics (Moderate Risk) may increase the serum concentration of RisperiDONE. Specifically, thioridazine may increase concentrations of risperidone. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Rolapitant: May increase the serum concentration of Thioridazine. Avoid combination
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Saquinavir: May enhance the QTc-prolonging effect of Thioridazine. Avoid combination
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Serotonergic Agents (High Risk): May enhance the adverse/toxic effect of Antipsychotic Agents. Specifically, serotonergic agents may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotic Agents may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Monitor therapy
Serotonin Reuptake Inhibitor/Antagonists: Antipsychotic Agents (Phenothiazines) may enhance the adverse/toxic effect of Serotonin Reuptake Inhibitor/Antagonists. Specifically, this may be manifest as symptoms consistent with serotonin syndrome or neuroleptic malignant syndrome. Serotonin Reuptake Inhibitor/Antagonists may enhance the hypotensive effect of Antipsychotic Agents (Phenothiazines). Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Sulpiride: Antipsychotic Agents may enhance the adverse/toxic effect of Sulpiride. Avoid combination
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tamoxifen: CYP2D6 Inhibitors (Moderate) may decrease serum concentrations of the active metabolite(s) of Tamoxifen. Specifically, CYP2D6 inhibitors may decrease the metabolic formation of highly potent active metabolites. Management: Consider alternatives with less of an inhibitory effect on CYP2D6 activity when possible. Consider therapy modification
Tamsulosin: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Tamsulosin. Monitor therapy
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrabenazine: May enhance the adverse/toxic effect of Antipsychotic Agents. Monitor therapy
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Thiopental: Antipsychotic Agents (Phenothiazines) may enhance the adverse/toxic effect of Thiopental. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Voriconazole: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Test Interactions
May interfere with urine detection of methadone and phencyclidine (false-positives) (Lancelin 2005; Long 1996).
Adverse Reactions
Frequency not defined.
Cardiovascular: ECG changes, hypotension, orthostatic hypotension, peripheral edema, prolonged QT Interval on ECG, torsades de pointes
Central nervous system: Confusion (sundowning), disruption of temperature regulation (Martinez 2002), drowsiness, drug-induced Parkinson disease, extrapyramidal reaction, headache, hyperactive behavior, lethargy, psychotic reaction, restlessness, seizure, tardive dyskinesia (Lehman 2004)
Dermatologic: Dermatitis, hyperpigmentation (Lehman 2004), pallor, skin photosensitivity, skin rash, urticaria
Endocrine & metabolic: Amenorrhea, galactorrhea not associated with childbirth, weight gain (Lehman 2004)
Gastrointestinal: Constipation, diarrhea, nausea, parotid gland enlargement, vomiting, xerostomia
Genitourinary: Breast engorgement, inhibited ejaculation, priapism, sexual difficulty (La Torre 2013), sexual disorder (La Torre 2013)
Hematologic & oncologic: Agranulocytosis, leukopenia
Ophthalmic: Blurred vision, corneal opacity (Lehman 2004), retinitis pigmentosa
Respiratory: Nasal congestion
Warnings/Precautions
Concerns related to adverse effects:
- Arrhythmias: [US Boxed Warning]: Has been shown to prolong the QTc interval in a dose-related manner; this may potentially cause Torsades de Pointes and sudden death. Therefore, thioridazine should be reserved for patients with schizophrenia who have failed to respond to adequate levels of other antipsychotic drugs. Risk of torsades de pointes and/or sudden death may be higher with in patients with bradycardia, hypokalemia, the presence of congenital prolongation of the QTc interval, reduced activity of cytochrome P450 (CYP-450) 2D6, or concomitant use of other drugs that prolong the QTc interval, inhibit CYP2D6, or interfere with the clearance of thioridazine. Consider a cardiac evaluation (including Holter monitoring) in patients who experience symptoms that may be associated with Torsades de Pointes (dizziness, palpitations, syncope). Discontinue therapy in patients with a QTc >500 msec.
- Anticholinergic effects: May cause anticholinergic effects (constipation, xerostomia, blurred vision, urinary retention); use with caution in patients with decreased gastrointestinal motility, paralytic ileus, urinary retention, BPH, xerostomia, or visual problems. Relative to other neuroleptics, thioridazine has a high potency of cholinergic blockade (Richelson 1999).
- Blood dyscrasias: Leukopenia, neutropenia, and/or agranulocytosis (sometimes fatal) have been reported in clinical trials and postmarketing reports with antipsychotic use; presence of risk factors (eg, preexisting low WBC or history of drug-induced leuko-/neutropenia) should prompt periodic blood count assessment. Discontinue therapy at first signs of blood dyscrasias or if absolute neutrophil count <1,000/mm3.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving).
- Esophageal dysmotility/Aspiration: Antipsychotic use has been associated with esophageal dysmotility and aspiration; risk increases with age. Use with caution in patients at risk for aspiration pneumonia (ie, Alzheimer disease), particularly in patients >75 years (Herzig 2017; Maddalena 2004).
- Extrapyramidal symptoms: May cause extrapyramidal symptoms (EPS), including pseudoparkinsonism, acute dystonic reactions, akathisia, and tardive dyskinesia. Risk of dystonia (and possibly other EPS) may be greater with increased doses, use of conventional antipsychotics, males, and younger patients. Factors associated with greater vulnerability to tardive dyskinesia include older in age, female gender combined with postmenopausal status, Parkinson disease, pseudoparkinsonism symptoms, affective disorders (particularly major depressive disorder), concurrent medical diseases such as diabetes, previous brain damage, alcoholism, poor treatment response, and use of high doses of antipsychotics (APA [Lehman 2004]; Soares-Weiser 2007). Consider therapy discontinuation with signs/symptoms of tardive dyskinesia.
- Hyperprolactinemia: Use associated with increased prolactin levels; clinical significance of hyperprolactinemia in patients with breast cancer or other prolactin-dependent tumors is unknown.
- Neuroleptic malignant syndrome (NMS): May be associated with NMS; monitor for mental status changes, fever, muscle rigidity, and/or autonomic instability. Following recovery from NMS, reintroduction of drug therapy should be carefully considered; if an antipsychotic agent is resumed, monitor closely for NMS.
- Ocular effects: May cause pigmentary retinopathy, characterized by diminution of visual acuity, brownish coloring of vision, and impairment of night vision, in patients exceeding recommended doses. Periodic eye examinations are recommended in patients receiving 600 mg/day or more (Oshika 1995).
- Orthostatic hypotension: May cause orthostatic hypotension; use with caution in patients at risk of this effect or in those who would not tolerate transient hypotensive episodes (cerebrovascular disease, cardiovascular disease, hypovolemia, or concurrent medication use which may predispose to hypotension/bradycardia).
- Temperature regulation: Impaired core body temperature regulation may occur; caution with strenuous exercise, heat exposure, dehydration, and concomitant medication possessing anticholinergic effects (Kwok 2005; Martinez 2002).
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with severe cardiovascular disease. Do not initiate therapy in patients with a QTc interval >450 msec.
- Dementia: [US Boxed Warning]: Elderly patients with dementia-related psychosis treated with antipsychotics are at an increased risk of death compared to placebo. Most deaths appeared to be either cardiovascular (eg, heart failure, sudden death) or infectious (eg, pneumonia) in nature. Use with caution in patients with Lewy body dementia or Parkinson disease dementia due to greater risk of adverse effects, increased sensitivity to extrapyramidal effects, and association with irreversible cognitive decompensation or death. The APA recommends giving preference to second generation antipsychotics over first generation antipsychotics in elderly patients with dementia-related psychosis due to a potentially greater risk of harm relative to second generation antipsychotics (APA [Reus 2016]). Thioridazine is not approved for the treatment of dementia-related psychosis.
- Hepatic impairment: Use with caution in patients with hepatic impairment.
- Seizure disorder: Use with caution in patients at risk of seizures; first-generation antipsychotics may lower the seizure threshold (APA [Lehman 2004]).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Avoid use; potent anticholinergic agent with potential to cause QT-interval prolongation.
Other warnings/precautions:
- Discontinuation of therapy: When discontinuing antipsychotic therapy, gradual dose reduction is advised to avoid withdrawal symptoms (ie, insomnia, headache, GI symptoms), unless discontinuation is due to significant adverse effects. The risk of withdrawal symptoms is highest following abrupt discontinuation of highly anticholinergic or dopaminergic antipsychotics (Cerovecki 2013). Additional factors, such as duration of antipsychotic exposure, indication for use, medication half-life, and risk for relapse, should be considered. In schizophrenia, there is no reliable indicator to differentiate the minority who will not from the majority who will relapse with drug discontinuation. However, studies in which the medications of well-stabilized patients were discontinued indicate that 75% of patients relapse within 6 to 24 months. Indefinite maintenance antipsychotic medication is generally recommended, especially for patients who have had multiple prior episodes or 2 episodes within 5 years (APA [Lehman 2004]).
Monitoring Parameters
Mental status; vital signs (as clinically indicated); ECG (baseline, then periodic; do not initiate if QTc >450 msec); weight, height, BMI, waist circumference (baseline; at every visit for the first 6 months; quarterly with stable antipsychotic dose); CBC (as clinically indicated; monitor frequently during the first few months of therapy in patients with preexisting low WBC or history of drug-induced leukopenia/neutropenia); electrolytes (baseline potassium; annually and as clinically indicated); liver function (annually and as clinically indicated); fasting plasma glucose level/HbA1c (baseline, then yearly; in patients with diabetes risk factors or if gaining weight, repeat 4 months after starting antipsychotic, then yearly); lipid panel (baseline; repeat every 2 years if LDL level is normal; repeat every 6 months if LDL level is >130 mg/dL); changes in menstruation, libido, development of galactorrhea, erectile and ejaculatory function (at each visit for the first 12 weeks after the antipsychotic is initiated or until the dose is stable, then yearly); abnormal involuntary movements or parkinsonian signs (baseline; repeat weekly until dose stabilized for at least 2 weeks after introduction and for 2 weeks after any significant dose increase); tardive dyskinesia (every 6 months; high-risk patients every 3 months); visual changes (inquire yearly); ocular examination (yearly in patients >40 years; every 2 years in younger patients) (ADA, 2004; Lehman, 2004; Marder, 2004).
Pregnancy
Pregnancy Considerations
Although outcome information has been published in case reports following maternal use of thioridazine in pregnancy, most information is available for phenothiazines as a class (Erkkola 1983; Heinonen 1977; Scanlan 1972; Slone 1977; Vince 1969). Jaundice or hyper- or hyporeflexia have been reported in newborn infants following maternal use of phenothiazines. Antipsychotic use during the third trimester of pregnancy has a risk for abnormal muscle movements (extrapyramidal symptoms [EPS]) and withdrawal symptoms in newborns following delivery. Symptoms in the newborn may include agitation, feeding disorder, hypertonia, hypotonia, respiratory distress, somnolence, and tremor; these effects may be self-limiting or require hospitalization.
When use in pregnancy is needed, the minimum effective maternal dose should be used to decrease the risk of EPS (ACOG 2008).
Because thioridazine increases prolactin concentrations, amenorrhea in women and impotence in men have been reported. False pregnancy tests may also occur with thioridazine use.
Patient Education
What is this drug used for?
- It is used to treat schizophrenia.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Constipation
- Diarrhea
- Dry mouth
- Stuffy nose
- Vomiting
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Abnormal movements
- Twitching
- Change in balance
- Trouble swallowing
- Trouble speaking
- Abnormal heartbeat
- Dizziness
- Passing out
- Chest pain
- Fast heartbeat
- Tremors
- Trouble moving
- Rigidity
- Confusion
- Mood changes
- Seizures
- Swelling of arms or legs
- Vision changes
- Severe fatigue
- Severe loss of strength and energy
- Agitation
- Pale skin
- Enlarged breasts
- Nipple discharge
- Sexual dysfunction
- No menstrual periods
- Neuroleptic malignant syndrome like fever, muscle cramps or stiffness, dizziness, severe headache, confusion, change in thinking, fast heartbeat, abnormal heartbeat, or sweating a lot
- Tardive dyskinesia like unable to control body movements; tongue, face, mouth, or jaw sticking out; mouth puckering; or puffing cheeks
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.