Boxed Warning
Carcinogenic:
Carcinogenicity has been seen in mice and rats treated chronically with metronidazole, another nitroimidazole agent. Although such data have not been reported for tinidazole, the two drugs are structurally related and have similar biologic effects. Limit use to approved indications only. Avoid chronic use.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
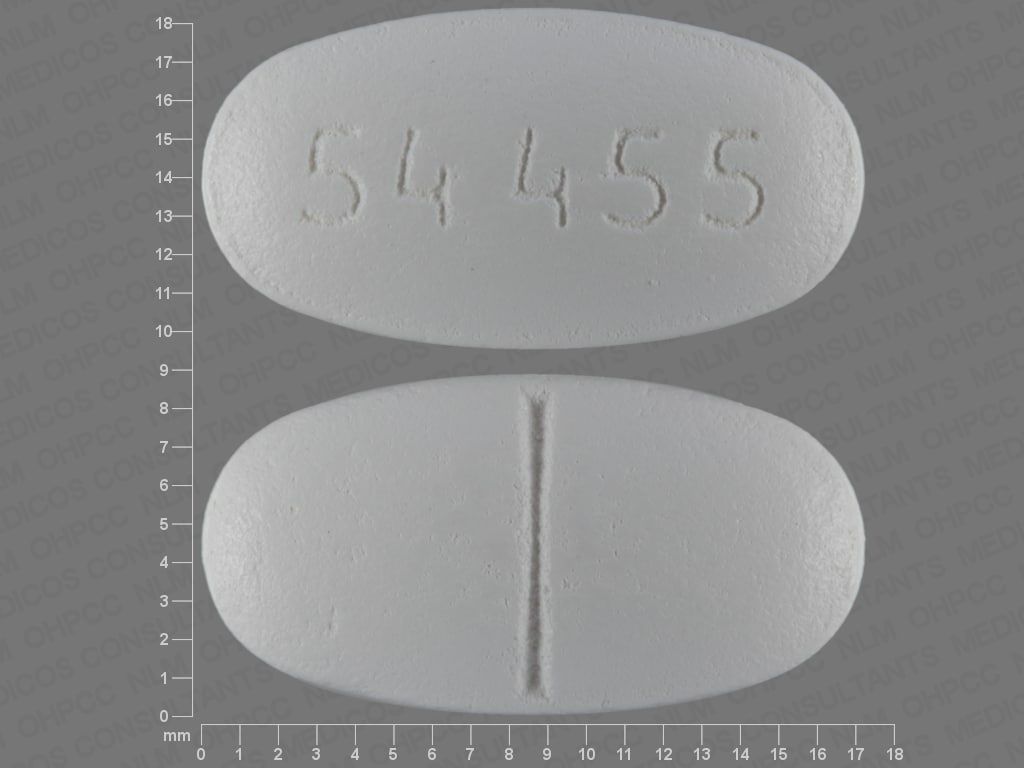
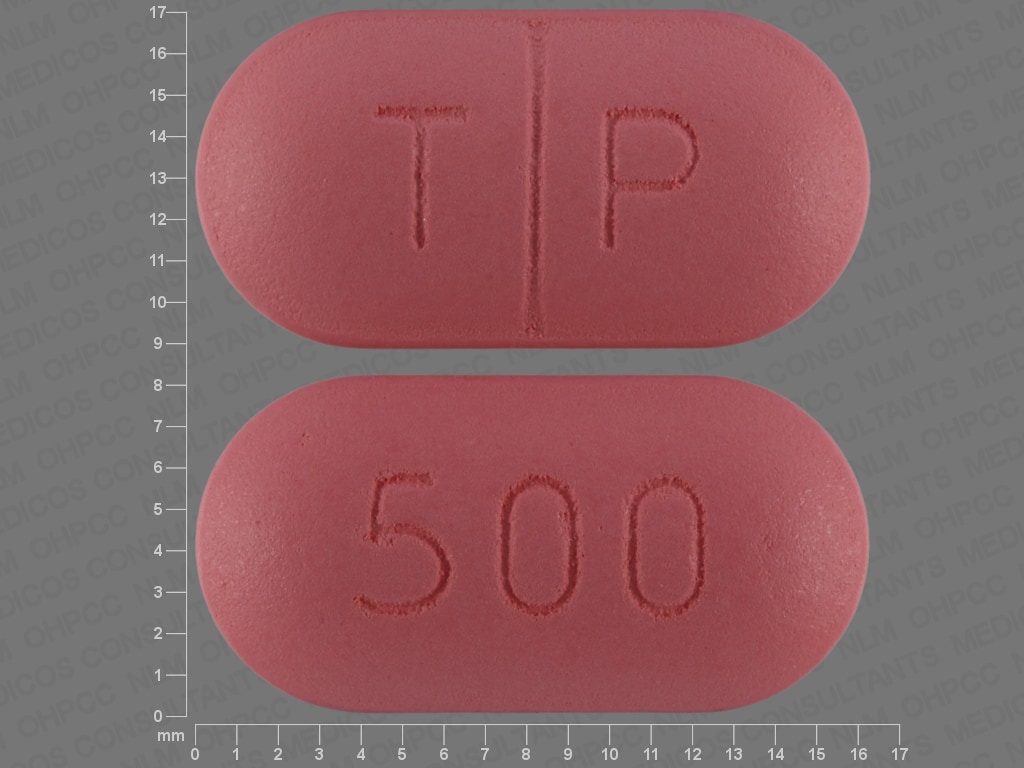
Tablet, Oral:
Tindamax: 250 mg [DSC] [contains fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake]
Tindamax: 500 mg [DSC] [scored; contains fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake]
Generic: 250 mg, 500 mg
Pharmacology
Mechanism of Action
After diffusing into the organism, it is proposed that tinidazole causes cytotoxicity by damaging DNA and preventing further DNA synthesis.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and complete
Distribution
Vd: ~50 L; distributes to most body tissues and fluids; crosses the blood-brain barrier
Metabolism
Hepatic via CYP3A4 (primarily); undergoes oxidation, hydroxylation and conjugation; forms a metabolite
Excretion
Urine (~20% to 25%); feces (~12%)
Time to Peak
1.6 hours (fasting, delayed ~2 hours when given with food)
Half-Life Elimination
13.2 hours
Protein Binding
12%
Use: Labeled Indications
Amebiasis: Treatment of intestinal amebiasis and amebic liver abscess caused by Entamoeba histolytica in adults and pediatric patients older than 3 years.
Limitations of use: Not indicated for the treatment of asymptomatic cyst passage.
Bacterial vaginosis: Treatment of bacterial vaginosis (formerly referred to as Haemophilus vaginitis, Gardnerella vaginitis, nonspecific vaginitis, or anaerobic vaginosis) in adult women.
Giardiasis: Treatment of giardiasis caused by Giardia duodenalis (also termed Giardia lamblia) in adults and pediatric patients older than 3 years.
Trichomoniasis: Treatment of trichomoniasis caused by Trichomonas vaginalis; treat partners of infected patients simultaneously to prevent reinfection.
Use: Off Label
Helicobacter pylori eradicationyes
Based on the American College of Gastroenterology Clinical Guideline for the Treatment of Helicobacter pylori Infection, tinidazole is an effective and recommended component of a multiple-drug regimen for the treatment of this condition.
Prophylaxis against sexually transmitted diseases following sexual assaultyes
Based on the Centers for Disease Control and Prevention (CDC) sexually transmitted diseases treatment guidelines, tinidazole, in combination with ceftriaxone and azithromycin, is a recommended regimen for prophylaxis against sexually transmitted diseases following sexual assault in adolescents and adults.
Urethritis, nongonococcal (persistent and recurrent)yes
Based on the CDC sexually transmitted diseases treatment guidelines, tinidazole is effective and recommended as treatment for recurrent and persistent urethritis for men who have sex with women and who live in areas where T. vaginalis is prevalent. Compliance with initial regimen and lack of reexposure to an untreated sex partner should be excluded prior to use. Sex partners should be referred for evaluation and appropriate treatment.
Contraindications
Hypersensitivity to tinidazole, nitroimidazole derivatives, or any component of the formulation.
Dosage and Administration
Dosing: Adult
Amebiasis, intestinal: Oral: 2 g once daily for 3 days
Amebiasis, liver abscess: Oral: 2 g once daily for 3 to 5 days
Bacterial vaginosis: Oral: 2 g once daily for 2 days or 1 g once daily for 5 days
Bacterial vaginosis, recurrent (off-label dose): Oral: 500 mg twice daily for 7 days followed by intravaginal therapy with boric acid, followed by intravaginal metronidazole suppressive therapy (CDC [Workowski 2015])
Giardiasis: Oral: 2 g as a single dose
Helicobacter pylori eradication (off-label use): Oral:
American College of Gastroenterology guidelines (Chey 2007; Chey 2017):
Concomitant regimen: 500 mg twice daily in combination with clarithromycin 500 mg twice daily, amoxicillin 1 g twice daily, and a standard-dose proton pump inhibitor twice daily; continue regimen for 10 to 14 days.
Sequential regimen: Amoxicillin 1 g twice daily plus a standard-dose proton pump inhibitor twice daily for 5 to 7 days; then follow with clarithromycin 500 mg twice daily, tinidazole 500 mg twice daily, and a standard-dose proton pump inhibitor daily for 5 to 7 days.
Hybrid regimen: Amoxicillin 1 g twice daily plus a standard-dose proton pump inhibitor twice daily for 7 days; then follow with amoxicillin 1 g twice daily, clarithromycin 500 mg twice daily, tinidazole 500 mg twice daily, and a standard-dose proton pump inhibitor twice daily for 7 days.
Prophylaxis against sexually transmitted diseases following sexual assault (off-label use): Oral: 2 g as a single dose in combination with azithromycin plus ceftriaxone (CDC [Workowski 2015])
Trichomoniasis: Oral: 2 g as a single dose; sexual partners should be treated at the same time
Trichomoniasis, persistent or recurrent (ie, treatment failure of nitroimidazole [eg, metronidazole]) (index case; treatment of sex partner; off-label dose): Oral: 2 g once daily for 7 days (CDC [Workowski 2015])
Urethritis, nongonococcal (recurrent or persistent urethritis in men who have sex with women and who live in regions where T. vaginalis is prevalent; off-label use): Oral: 2 g as a single dose. Note: Compliance with initial regimen and lack of reexposure to an untreated sex partner should be excluded prior to use (CDC [Workowski 2015])
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Amebiasis, intestinal: Children >3 years and Adolescents: Oral: 50 mg/kg/day for 3 days; maximum daily dose: 2000 mg/day; for patients with severe and extraintestinal disease, administer for 5 days (Red Book [AAP], 2012)
Amebiasis, liver abscess: Children >3 years and Adolescents: Oral: 50 mg/kg/day for 3 to 5 days; maximum daily dose: 2000 mg/day
Bacterial vaginosis: Adolescents: Oral: 2000 mg once daily for 2 days or 1000 mg once daily for 5 days (CDC, 2010)
Giardiasis: Children >3 years and Adolescents: Oral: 50 mg/kg as a single dose; maximum dose: 2000 mg
Helicobacter pylori infection: Limited data available: Children >3 years and Adolescents: Oral: 20 mg/kg/day in 1 to 2 divided doses for 5 to 7 days in combination with other agents; some studies have used a longer duration of 2 to 6 weeks; maximum daily dose: 1000 mg/day (Francavilla, 2005; Moshkowitz, 1998; Nijevitch, 2000; Oderda, 1992)
Nongonococcal urethritis, recurrent/persistent: Adolescents: Oral: 2000 mg as a single dose in combination with azithromycin (CDC, 2010)
Trichomoniasis:
Children >3 years: Oral: 50 mg/kg as a single dose; maximum dose: 2000 mg (Red Book [AAP], 2012)
Adolescents: Oral: 2000 mg as a single dose; sexual partners should be treated at the same time; if treatment failure, can consider extended regimen of 2000 mg once daily for 5 days (CDC, 2010; Red Book [AAP], 2012)
Extemporaneously Prepared
A 67 mg/mL suspension may be made with tablets and cherry syrup. Crush four 500 mg tablets in a mortar and reduce to a fine powder. Add 10 mL cherry syrup and mix to a uniform paste; mix while adding cherry syrup in incremental proportions to almost 30 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 30 mL. Label "shake well". Stable for 7 days.
Tindamax® prescribing information, Mission Pharmacal Company, San Antonio, TX, 2007. Available at http://www.accessdata.fda.gov/drugsatfda_docs/label/2007/021618s003lbl.pdf
Administration
Administer with food.
Dietary Considerations
The manufacturer recommends that ethanol be avoided during treatment and for 3 days after therapy is complete.
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light.
Tinidazole Images
Drug Interactions
Alcohol (Ethyl): Tinidazole may enhance the adverse/toxic effect of Alcohol (Ethyl). A disulfiram-like reaction may occur. Avoid combination
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Disulfiram: Tinidazole may enhance the adverse/toxic effect of Disulfiram. Avoid combination
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Test Interactions
May interfere with AST, ALT, triglycerides, glucose, and LDH testing
Adverse Reactions
1% to 10%:
Central nervous system: Fatigue (≤2%), malaise (≤2%), dizziness (≤1%), headache (≤1%)
Dermatologic: Body odor (vaginal: >2%)
Endocrine & metabolic: Hypermenorrhea (>2%)
Gastrointestinal: Dysgeusia (bitter taste, metallic taste: 4% to 6%), nausea (3% to 5%), anorexia (2% to 3%), decreased appetite (>2%), flatulence (>2%), dyspepsia (≤2%), abdominal cramps (≤2%), epigastric distress (≤2%), vomiting (1% to 2%), constipation (≤1%)
Genitourinary: Vulvovaginal candidiasis (5%), dysuria (>2%), pelvic pain (>2%), urine abnormality (>2%), vulvovaginal disease (discomfort) (>2%)
Neuromuscular & skeletal: Weakness (1% to 2%)
Renal: Urinary tract infection (>2%)
Respiratory: Upper respiratory tract infection (>2%)
Frequency not defined:
Cardiovascular: Flushing, palpitations
Central nervous system: Ataxia, burning sensation, drowsiness, insomnia, peripheral neuropathy (transient; includes numbness and paresthesia), seizure, vertigo
Dermatologic: Diaphoresis, pruritus, skin rash, urticaria
Endocrine & metabolic: Increased thirst
Gastrointestinal: Abdominal pain, diarrhea, oral candidiasis, salivation, stomatitis, tongue discoloration, xerostomia
Genitourinary: Dark urine, vaginal discharge
Hematologic & oncologic: Leukopenia (transient), neutropenia (transient)
Hepatic: Increased serum transaminases
Hypersensitivity: Angioedema
Infection: Candidiasis (overgrowth)
Neuromuscular & skeletal: Arthralgia, arthritis, myalgia
Miscellaneous: Fever
<1%, postmarketing, and/or case reports: Bronchospasm, coma, confusion, depression, dyspnea, erythema multiforme, hairy tongue, hypersensitivity reaction (acute, severe), pharyngitis, Stevens-Johnson syndrome, thrombocytopenia (reversible)
Warnings/Precautions
Concerns related to adverse effects:
- Carcinogenic: [US Boxed Warning]: Carcinogenicity has been observed with another nitroimidazole derivative (metronidazole) in animal studies; use should be reserved for approved indications only. Avoid chronic use.
- CNS effects: Seizures and peripheral neuropathy (eg, extremity numbness and paresthesia) have been reported with tinidazole and other nitroimidazole derivatives; discontinue treatment if abnormal neurologic signs or symptoms occur.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD), pseudomembranous colitis, and/or vaginal candidiasis. CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Blood dyscrasias: Use with caution in patients with current or a history of blood dyscrasias.
- Hepatic impairment: Use with caution in patients with hepatic impairment.
Pregnancy
Pregnancy Considerations
Tinidazole crosses the human placenta and enters the fetal circulation (Karhunen 1984).
The safety of tinidazole for the treatment of bacterial vaginosis or trichomoniasis in pregnant women has not been well evaluated. Other agents are preferred for use during pregnancy (CDC [Workowski 2015]).
Patient Education
What is this drug used for?
- It is used to treat infections.
Frequently reported side effects of this drug
- Nausea
- Bad taste
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Burning or numbness feeling
- Seizures
- Vaginal pain, itching, and discharge
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.