Boxed Warning
Experienced physician:
Patients with acute promyelocytic leukemia (APL) are at high risk in general and can have severe adverse reactions to tretinoin. Therefore, administer tretinoin only to patients with APL under the strict supervision of a health care provider who is experienced in the management of patients with acute leukemia, and in a facility with laboratory and supportive services sufficient to monitor drug tolerance and protect and maintain a patient compromised by drug toxicity, including respiratory compromise. Use of tretinoin requires that the health care provider conclude the possible benefit to the patient outweighs the following known adverse reactions in therapy.
APL differentiation syndrome:
Approximately 25% of patients with APL treated with tretinoin have experienced the retinoic acid-APL (RA-APL) syndrome, characterized by fever, dyspnea, acute respiratory distress, weight gain, radiographic pulmonary infiltrates, pleural and pericardial effusions, edema, and hepatic, renal, and multiorgan failure. This syndrome occasionally has been accompanied by impaired myocardial contractility and episodic hypotension. It has been observed with or without concomitant leukocytosis. Endotracheal intubation and mechanical ventilation have been required in some cases due to progressive hypoxemia, and several patients have expired with multiorgan failure. The syndrome generally occurs during the first month of treatment, with some cases reported following the first dose of tretinoin.
The management of the syndrome has not been defined rigorously, but high-dose steroids given at the first suspicion of the RA-APL syndrome appear to reduce morbidity and mortality. At the first signs suggestive of the syndrome (eg, unexplained fever, dyspnea and/or weight gain, abnormal chest auscultatory findings, radiographic abnormalities), initiate high-dose steroids (dexamethasone 10 mg intravenous [IV] administered every 12 hours for 3 days or until the resolution of symptoms) immediately, irrespective of the leukocyte count. The majority of patients do not require termination of tretinoin therapy during treatment of the RA-APL syndrome. However, in cases of moderate and severe RA-APL syndrome, consider temporary interruption of tretinoin therapy.
Leukocytosis:
During tretinoin treatment, approximately 40% of patients will develop rapidly evolving leukocytosis. Patients who present with high white blood cell (WBC) at diagnosis (more than 5 × 109/L) have an increased risk of a further rapid increase in WBC counts. Rapidly evolving leukocytosis is associated with a higher risk of life-threatening complications.
If signs and symptoms of the RA-APL syndrome are present together with leukocytosis, immediately initiate treatment with high-dose steroids. Some investigators routinely add chemotherapy to tretinoin treatment in the case of patients presenting with a WBC count of more than 5 × 109/L or in the case of a rapid increase in WBC count for patients leukopenic at start of treatment, and have reported a lower incidence of the RA-APL syndrome. Consider adding full-dose chemotherapy (including an anthracycline if not contraindicated) to tretinoin therapy on day 1 or 2 for patients presenting with a WBC count of more than 5 × 109/L; immediately add for patients presenting with a WBC count of less than 5 x 109/L, if the WBC count reaches greater than or equal to 6 × 109/L by day 5, greater than or equal to 10 × 109/L by day 10, or greater than or equal to 15 × 109/L by day 28.
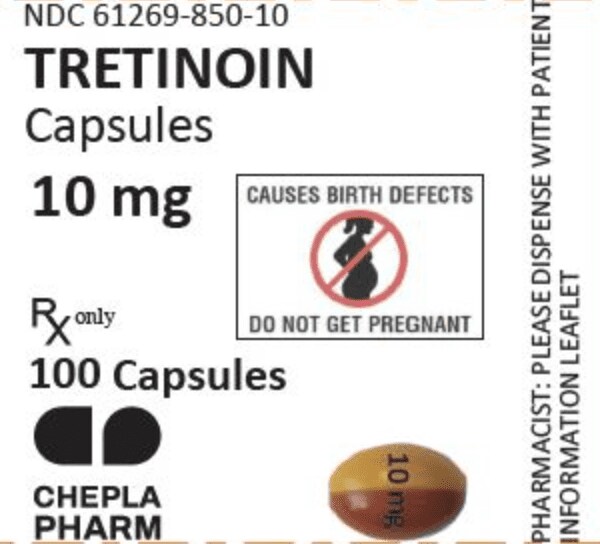
Pregnancy:
Pregnancy (Category D): There is a high risk that a severely deformed infant will result if tretinoin is administered during pregnancy. If, nonetheless, it is determined that tretinoin represents the best available treatment for a pregnant woman or a woman of childbearing potential, it must be assured that the patient has received full information and warnings of the risk to the fetus if she were to be pregnant and of the risk of possible contraception failure. Instruct the patient to use 2 reliable forms of contraception simultaneously during therapy and for 1 month following discontinuation of therapy, and emphasize the need for using dual contraception, unless abstinence is the chosen method.
Within 1 week prior to the institution of tretinoin therapy, collect blood or urine from the patient for a serum or urine pregnancy test with a sensitivity of at least 50 milliunits/mL. When possible, delay tretinoin therapy until a negative result from this test is obtained. When a delay is not possible, place the patient on 2 reliable forms of contraception. Repeat pregnancy testing and contraception counseling monthly throughout the period of tretinoin treatment.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Generic: 10 mg
Pharmacology
Mechanism of Action
Tretinoin appears to bind one or more nuclear receptors and decreases proliferation and induces differentiation of APL cells; initially produces maturation of primitive promyelocytes and repopulates the marrow and peripheral blood with normal hematopoietic cells to achieve complete remission
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed
Metabolism
Hepatic via CYP; primary metabolite: 4-oxo-all-trans-retinoic acid; displays autometabolism
Excretion
Urine (63%); feces (30%)
Time to Peak
Serum: 1 to 2 hours
Half-Life Elimination
Terminal: Parent drug: 0.5 to 2 hours
Protein Binding
>95%, predominantly to albumin
Use: Labeled Indications
Acute promyelocytic leukemia (remission induction): Induction of remission in patients with acute promyelocytic leukemia, French American British (FAB) classification M3 (including the M3 variant) characterized by t(15;17) translocation and/or PML/RARα gene presence
Use: Off Label
Acute promyelocytic leukemia (consolidation therapy)a
Data from studies of combination chemotherapy in adults with acute promyelocytic leukemia (APL) support the use of tretinoin as part of the consolidation phase of treatment Lo-Coco 2010, Sanz 2010. Data from a study of tretinoin in combination with arsenic trioxide in adults with APL supports the use of tretinoin as a part of the consolidation phase of treatment Ravandi 2009.
Acute promyelocytic leukemia (maintenance therapy in intermediate- and high-risk patients)a
Data from studies of combination chemotherapy in adult patients with acute promyelocytic leukemia (APL) support the use of tretinoin as part of the maintenance phase of treatment Ades 2008, Powell 2010, Sanz 2004.
Data from a multicenter study of combination chemotherapy in pediatrics with APL supports the use of tretinoin as part of the maintenance phase of treatment Ortega 2005.
Contraindications
Hypersensitivity to tretinoin, other retinoids, parabens, or any component of the formulation
Dosage and Administration
Dosing: Adult
Note: Induction treatment of APL with tretinoin should be initiated early; discontinue if pending cytogenetic analysis does not confirm t(15;17) translocation or the presence of the PML/RARα fusion protein.
Acute promyelocytic leukemia (APL): Oral:
Remission induction (manufacturer’s labeling): 45 mg/m2/day in 2 equally divided doses until documentation of complete remission (CR); discontinue 30 days after CR or after 90 days of treatment, whichever occurs first
Remission induction (in combination with an anthracycline ± cytarabine): 45 mg/m2/day in 2 equally divided doses until complete remission or 90 days (Powell 2010) or until complete hematologic remission (Ades 2008; Sanz 2008; Sanz 2010)
Remission induction (in combination with arsenic trioxide; off-label combination): 45 mg/m2/day in 2 equally divided doses until <5% blasts in marrow and no abnormal promyelocytes or up to 85 days (Estey 2006; Ravandi 2009)
Consolidation therapy (off-label use): 45 mg/m2/day in 2 equally divided doses for 15 days each month for 3 months (in combination with chemotherapy) (Lo-Coco 2010; Sanz 2010) or 45 mg/m2/day for 14 days every 4 weeks for 7 cycles (in combination with arsenic trioxide) (Ravandi 2009)
Maintenance therapy, intermediate- and high-risk patients (off-label use): 45 mg/m2/day in 2 equally divided doses for 15 days every 3 months for 2 years (Ades 2008; Sanz 2004) or 45 mg/m2/day in 2 equally divided doses for 7 days every other week for 1 year (Powell 2010)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Refer to individual protocols: Induction treatment of APL with tretinoin should be initiated early; discontinue if pending cytogenetic analysis does not confirm t(15;17) translocation or the presence of the PML/RARα fusion protein.
Acute promyelocytic leukemia (APL): Oral:
Children and Adolescents: Limited data available (de Botton, 2004; Gregory, 2009; Mann, 2001; Ortega, 2005; Sanz, 2009; Testi, 2005):
Remission induction: 45 mg/m2/day in two equally divided doses until documentation of complete remission (CR); discontinue after CR or after 90 days of treatment, whichever occurs first
Remission induction (in combination with an anthracycline): 25 mg/m2/day in two equally divided doses until complete remission or 90 days
Consolidation therapy, intermediate- and high-risk patients: 25 mg/m2/day in two equally divided doses for 15 days each month for 3 months
Maintenance therapy, intermediate- and high-risk patients: 25 mg/m2/day in two equally divided doses for 15 days every 3 months for 2 years
Dosing: Adjustment for Toxicity
APL differentiation syndrome: Initiate dexamethasone 10 mg IV every 12 hours for 3 to 5 days; consider interrupting tretinoin until resolution of hypoxia
Liver function tests >5 times the upper limit of normal: Consider temporarily withholding treatment
Extemporaneously Prepared
Although the manufacturer does not recommend the use of the capsule contents to extemporaneously prepare a suspension of tretinoin (due to reports of low plasma levels) (Vesanoid data on file), there are limited case reports of use in patients who are unable to swallow the capsules whole. In a patient with a nasogastric (NG) tube, tretinoin capsules were cut open, with partial aspiration of the contents aspirated into a glass syringe. The residual capsule contents were mixed with soybean oil, aspirated into the syringe, and administered (Shaw 1995). Tretinoin capsules have also been mixed with sterile water (~20 mL) and heated in a water bath to melt the capsules and create an oily suspension for NG tube administration (Bargetzi 1996). Tretinoin has also been administered sublingually by squeezing the capsule contents beneath the tongue (Kueh 1999).
Bargetzi MJ, Tichelli A, Gratwohl A, et al, "Oral All-Transretinoic Acid Administration in Intubated Patients With Acute Promyelocytic Leukemia," Schweiz Med Wochenschr, 1996, 126(45):1944-5.8946598Kueh YK, Liew PP, Ho PC, et al, "Sublingual Administration of All-Trans-Retinoic Acid to a Comatose Patient With Acute Promyelocytic Leukemia," Ann Pharmacother, 1999, 33(4):503-5.10332546Shaw PJ, Atkins MC, Nath CE, et al, "ATRA Administration in the Critically Ill Patient," Leukemia, 1995, 9(7):1288.7630206Vesanoid data on file, Roche Pharmaceuticals
Administration
Administer orally with a meal; do not crush capsules.
Tretinoin has also been administered sublingually by squeezing the capsule contents beneath the tongue (Kueh 1999).
Low plasma concentrations have been reported when tretinoin has been administered through a feeding tube, although patient-specific impaired absorption or a lack of excipient (eg, soybean oil) may have been a contributing factor (Takitani 2004).
Dietary Considerations
The absorption of retinoids (as a class) is enhanced when taken with food. Capsule contains soybean oil.
Storage
Store capsule at 20°C to 25°C (68°F to 77°F). Protect from light.
Tretinoin (Systemic) Images
Drug Interactions
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Antifibrinolytic Agents: Tretinoin (Systemic) may enhance the thrombogenic effect of Antifibrinolytic Agents. Monitor therapy
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Multivitamins/Fluoride (with ADE): May enhance the adverse/toxic effect of Retinoic Acid Derivatives. Avoid combination
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the adverse/toxic effect of Retinoic Acid Derivatives. Avoid combination
Multivitamins/Minerals (with AE, No Iron): May enhance the adverse/toxic effect of Retinoic Acid Derivatives. Avoid combination
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Progestins (Contraceptive): Retinoic Acid Derivatives may diminish the therapeutic effect of Progestins (Contraceptive). Retinoic Acid Derivatives may decrease the serum concentration of Progestins (Contraceptive). Management: Two forms of effective contraception should be used in patients receiving retinoic acid derivatives. Microdosed progesterone-only preparations (ie, minipills that do not contain estrogen) are considered an inadequate method of contraception. Consider therapy modification
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tetracyclines: May enhance the adverse/toxic effect of Retinoic Acid Derivatives. The development of pseudotumor cerebri is of particular concern. Avoid combination
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Vitamin A: May enhance the adverse/toxic effect of Retinoic Acid Derivatives. Avoid combination
Adverse Reactions
Most patients will experience drug-related toxicity, especially headache, fever, weakness and fatigue. These are seldom permanent or irreversible and do not typically require therapy interruption.
>10%:
Cardiovascular: Peripheral edema (52%), chest discomfort (32%), edema (29%), cardiac arrhythmia (23%), flushing (23%), hypotension (14%), hypertension (11%), localized phlebitis (11%)
Central nervous system: Headache (86%), malaise (66%), shivering (63%), pain (37%), dizziness (20%), anxiety (17%), paresthesia (17%), depression (14%), insomnia (14%), confusion (11%)
Dermatologic: Xeroderma (≤77%), skin rash (54%), diaphoresis (20%), pruritus (20%), alopecia (14%), skin changes (14%)
Endocrine & metabolic: Hypercholesterolemia (≤60%), hypertriglyceridemia (≤60%), weight gain (23%), weight loss (17%)
Gastrointestinal: Dry mucous membranes (≤77%), nausea (≤57%), vomiting (≤57%), gastrointestinal hemorrhage (34%), abdominal pain (31%), mucositis (26%), diarrhea (23%), anorexia (17%), constipation (17%), dyspepsia (14%), abdominal distention (11%)
Hematologic & oncologic: Hemorrhage (60%), leukocytosis (40%), disseminated intravascular coagulation (26%)
Hepatic: Increased liver enzymes (50% to 60%)
Infection: Infection (58%)
Neuromuscular & skeletal: Ostealgia (77%), APL differentiation syndrome (≤25%), myalgia (14%)
Ophthalmic: Eye disease (17%), visual disturbance (17%)
Otic: Otalgia (23%; ear fullness)
Renal: Renal insufficiency (11%)
Respiratory: Upper respiratory complaint (63%), dyspnea (60%), respiratory insufficiency (26%), pleural effusion (20%), pneumonia (14%), rales (14%), wheezing (expiratory: 14%)
Miscellaneous: Fever (83%)
1% to 10%:
Cardiovascular: Cardiac failure (6%), facial edema (6%), cardiomegaly (3%), cardiomyopathy (3%), cerebrovascular accident (3%), heart murmur (3%), ischemia (3%), myocardial infarction (3%), myocarditis (3%), pericarditis (3%)
Central nervous system: Agitation (9%), cerebral hemorrhage (9%), flank pain (9%), intracranial hypertension (9%), hallucination (6%), abnormal gait (3%), agnosia (3%), aphasia (3%), asterixis (3%), ataxia (3%), brain disease (3%), cerebral edema (cerebellar: 3%), central nervous system depression (3%), coma (3%), dementia (3%), drowsiness (3%), dysarthria (3%), facial paralysis (3%), forgetfulness (3%), hemiplegia (3%), hyporeflexia (3%), hypothermia (3%), loss of consciousness (3%), seizure (3%), speech disturbance (3%)
Dermatologic: Cellulitis (8%), pallor (6%)
Endocrine & metabolic: Disturbance in fluid balance (6%), acidosis (3%)
Gastrointestinal: Gastrointestinal ulcer (3%)
Genitourinary: Dysuria (9%), benign prostatic hypertrophy (3%), urinary frequency (3%)
Hematologic & oncologic: Lymphatic disease (6%)
Hepatic: Hepatosplenomegaly (9%), ascites (3%), hepatitis (3%)
Local: Local inflammation (bone: 3%)
Neuromuscular & skeletal: Lower extremity weakness (3%), myelopathy (3%), tremor (3%)
Ophthalmic: Decreased visual acuity (6%), decreased pupillary reflex (3%), visual field defect (3%)
Otic: Hearing loss (6%; may be irreversible)
Renal: Acute renal failure (3%), renal tubular necrosis (3%)
Respiratory: Lower respiratory signs and symptoms (9%), pulmonary infiltrates (6%), asthma (3%), laryngeal edema (3%), pulmonary hypertension (3%)
<1%, postmarketing, and/or case reports: Arterial thrombosis, basophilia, erythema nodosum, histamine release (hyperhistaminemia), hypercalcemia, hypersensitivity angiitis, myositis, pancreatitis, pseudotumor cerebri, renal infarction, Sweet's syndrome, thrombocythemia, ulcer (genital), venous thrombosis
Warnings/Precautions
Concerns related to adverse effects:
- APL differentiation syndrome: [US Boxed Warning]: About 25% of patients with APL treated with tretinoin have experienced APL differentiation syndrome (formerly called retinoic-acid-APL [RA-APL] syndrome), which is characterized by fever, dyspnea, acute respiratory distress, weight gain, radiographic pulmonary infiltrates, and pleural or pericardial effusions, edema, and hepatic, renal, and/or multiorgan failure. The syndrome may be accompanied by impaired myocardial contractility and episodic hypotension. It has been observed with or without concomitant leukocytosis. Intubation and mechanical ventilation have been required in some cases due to progressive hypoxemia; fatalities due to multiorgan failure have occurred. The syndrome generally occurs during the first month of treatment, with some cases reported following the first dose. Management has not been defined, although high-dose steroids given at the first suspicion appear to reduce morbidity and mortality. Regardless of the leukocyte count, at the first signs suggestive of APL differentiation syndrome (eg, unexplained fever, dyspnea and/or weight gain, abnormal chest auscultatory findings, radiographic abnormalities), immediately initiate corticosteroid therapy with dexamethasone 10 mg IV every 12 hours for 3 to 5 days (or until the symptoms resolve); taper off over 2 weeks. Most patients do not require termination of tretinoin therapy during treatment of the APL differentiation syndrome.
- Cardiovascular effects: Venous thrombosis and MI have been reported in patient without risk factors for thrombosis or MI. The risk for thrombosis (arterial and venous) is increased during the first month of treatment. Use with caution with antifibrinolytic agents; thrombotic complications have been reported (rarely) with concomitant use.
- CNS effects: May cause headache, malaise, and/or dizziness; caution patients about performing tasks which require mental alertness (eg, operating machinery or driving).
- Leukocytosis: [US Boxed Warning]: During treatment, ~40% of patients will develop rapidly evolving leukocytosis. Patients who present with a high WBC at diagnosis (>5,000/mm3) are at increased risk of further rapid increase in WBC counts. Rapidly evolving leukocytosis is associated with a higher risk of life-threatening complications. Initiate treatment with high-dose corticosteroids immediately if signs and symptoms of APL differentiation syndrome are present with leukocytosis. Chemotherapy may be added to tretinoin treatment in patients presenting with a WBC count >5,000/mm3 or for a rapid WBC increase in patients leukopenic at start of treatment (may result in a lower incidence of APL differentiation syndrome). Consider adding full-dose chemotherapy (including an anthracycline if not contraindicated) to tretinoin therapy on day 1 or 2 for patients presenting with a WBC count >5,000/mm3; immediately add for patients presenting with a WBC count <5,000/mm3 if the WBC count reaches ≥6,000/mm3 by day 5, ≥10,000/mm3 by day 10, or ≥15,000/mm3 by day 28.
- Lipid effects: Up to 60% of patients experienced hypercholesterolemia or hypertriglyceridemia, which were reversible upon completion of treatment.
- Liver function test abnormalities: Elevated liver function test results occur in 50% to 60% of patients during treatment. Carefully monitor liver function test results during treatment and give consideration to a temporary withdrawal of tretinoin if test results reach >5 times the upper limit of normal. Most liver function test abnormalities will resolve without interruption of treatment or after therapy completion.
- Pseudotumor cerebri: Retinoids have been associated with pseudotumor cerebri (benign intracranial hypertension), especially in children. Concurrent use of other drugs associated with this effect (eg, tetracyclines) may increase risk. Early signs and symptoms include papilledema, headache, nausea, vomiting, visual disturbances, intracranial noises, or pulsate tinnitus.
Disease-related concerns:
- APL: Tretinoin treatment for APL should be initiated early, discontinue if pending cytogenetic analysis does not confirm APL by t(15;17) translocation or the presence of the PML/RARα fusion protein (caused by translocation of the promyelocytic [PML] gene on chromosome 15 and retinoic acid receptor [RAR] alpha gene on chromosome 17).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Sedatives: Effects may be potentiated when used with other sedative drugs or ethanol.
Special populations:
- Pregnancy: [US Boxed Warning]: High risk of teratogenicity; if treatment with tretinoin is required in women of childbearing potential, two reliable forms of contraception should be used during and for 1 month after discontinuation of treatment, unless abstinence is the chosen method. Within 1 week prior to starting therapy, serum or urine pregnancy test (sensitivity at least 50 milliunits/mL) should be collected. If possible, delay therapy until results are available. Repeat pregnancy testing and contraception counseling monthly throughout the period of treatment. Microdosed progesterone products (“minipill”) may provide inadequate pregnancy protection. Repeat pregnancy testing and contraception counseling monthly throughout the period of treatment. If possible, initiation of treatment with tretinoin should be delayed until negative pregnancy test result is confirmed.
Dosage form specific issues:
- Product interchange: Tretinoin (which is also known as all-trans retinoic acid, or ATRA) and isotretinoin may be confused, while both products may be used in cancer treatment, they are not interchangeable; verify product prior to dispensing and administration to prevent medication errors.
Other warnings/precautions:
- Experienced physician: [US Boxed Warning]: Should be administered under the supervision of an experienced cancer chemotherapy physician. Patients with APL are at high risk and can have severe adverse reactions to tretinoin. Administer tretinoin only to patients with APL under the close supervision of a provider who is experienced in the management of patients with acute leukemia, and in a facility with laboratory and supportive services for appropriate monitoring.
Monitoring Parameters
Bone marrow cytology to confirm t(15;17) translocation or the presence of the PML/RARα fusion protein (do not withhold treatment initiation for results); monitor CBC with differential, coagulation profile, liver function test results, and triglyceride and cholesterol levels frequently; monitor closely for signs of APL differentiation syndrome (eg, monitor volume status, pulmonary status, temperature, respiration)
Pregnancy
Pregnancy Risk Factor
D
Pregnancy Considerations
[US Boxed Warning]: There is a high risk that a severely deformed infant will result if tretinoin capsules are administered during pregnancy. Tretinoin was detected in the serum of a neonate at birth following maternal use of standard doses during pregnancy (Takitani 2005). Major fetal abnormalities and spontaneous abortions have been reported with other retinoids; some of these abnormalities were fatal. Birth defects associated with exposure to retinoids include facial dysmorphia, cleft palate, eye abnormalities and abnormalities of the central nervous system, cardiovascular system, musculoskeletal system, and parathyroid hormone deficiencies. All exposed fetuses have the potential to be affected.
Use in humans for the treatment of acute promyelocytic leukemia (APL) is limited and exposure occurred after the first trimester in most cases (Valappil 2007). If the clinical condition of a patient presenting with APL during pregnancy warrants immediate treatment, tretinoin use should be avoided in the first trimester; treatment with tretinoin may be considered in the second and third trimester with careful fetal monitoring, including cardiac monitoring (Sanz 2009).
[US Boxed Warning]: If, nonetheless, it is determined that tretinoin capsules represent the best available treatment for a pregnant woman or a woman of childbearing potential, it must be assured that the patient has received full information and warnings of the risk to the fetus if she were to be pregnant and of the risk of possible contraception failure and has been instructed in the need to use two reliable forms of contraception simultaneously during therapy and for 1 month following discontinuation of therapy, and has acknowledged her understanding of the need for using dual contraception, unless abstinence is the chosen method. Within 1 week prior to the institution of tretinoin capsules therapy, the patient should have blood or urine collected for a serum or urine pregnancy test with a sensitivity of at least 50 mIU/mL. When possible, tretinoin capsules therapy should be delayed until a negative result from this test is obtained. When a delay is not possible, the patient should be placed on two reliable forms of contraception. Pregnancy testing and contraception counseling should be repeated monthly throughout the period of tretinoin capsules treatment. Contraception must be used even when there is a history of infertility or menopause, unless a hysterectomy has been performed.
Patient Education
What is this drug used for?
- It is used to treat a type of leukemia.
Frequently reported side effects of this drug
- Flushing
- Abdominal pain
- Constipation
- Diarrhea
- Nausea
- Vomiting
- Bone pain
- Skin irritation
- Loss of strength and energy
- Dry mouth
- Dry eyes
- Dry skin
- Dry lips
- Sweating a lot
- Hair loss
- Mouth sores
- Flank pain
- Shivering
- Common cold symptoms
- Muscle pain
- Weight loss
- Lack of appetite
- Ear pain
- Mouth irritation
- Anxiety
- Trouble sleeping
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Infection
- Retinoic-acid-APL syndrome like fever, shortness of breath, difficulty breathing, or weight gain.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Blood clots like numbness or weakness on one side of the body; pain, redness, tenderness, warmth, or swelling in the arms or legs; change in color of an arm or leg; chest pain; shortness of breath; fast heartbeat; or coughing up blood.
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or vision changes.
- Trouble hearing
- Hearing loss
- Abdominal swelling
- Abnormal heartbeat
- Burning or numbness feeling
- Depression
- Severe pulmonary disorder like lung or breathing problems like trouble breathing, shortness of breath, or a cough that is new or worse.
- Severe headache
- Dizziness
- Passing out
- Vision changes
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Confusion
- Sensing things that seem real but are not
- Pale skin
- Brain edema like severe headache, dizziness, nausea, vomiting, seizures.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.