Boxed Warning
Hyperkalemia:
Abnormal elevation of serum potassium levels (at least 5.5 mEq/L) can occur with all potassium-sparing agents, including triamterene. Hyperkalemia is more likely to occur in patients with renal impairment and diabetes (even without evidence of renal impairment), and in elderly or severely ill patients. Because uncorrected hyperkalemia may be fatal, serum potassium levels must be monitored at frequent intervals especially in patients receiving triamterene, when dosages are changed, or with any illness that may influence renal function.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
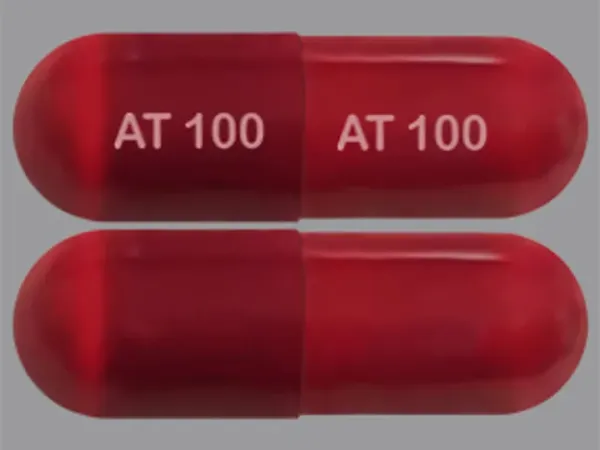
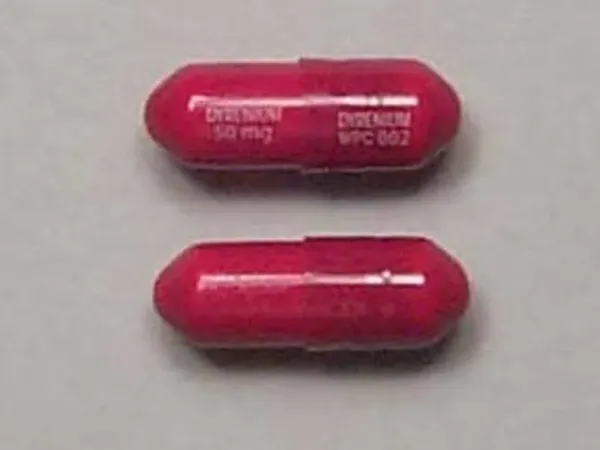
Capsule, Oral:
Dyrenium: 50 mg, 100 mg [contains fd&c yellow #6 (sunset yellow)]
Generic: 50 mg, 100 mg
Pharmacology
Mechanism of Action
Blocks epithelial sodium channels in the late distal convoluted tubule (DCT) and collecting duct which inhibits sodium reabsorption from the lumen. This effectively reduces intracellular sodium, decreasing the function of Na+/K+ ATPase, leading to potassium retention and decreased calcium, magnesium, and hydrogen excretion. As sodium uptake capacity in the DCT/collecting duct is limited, the natriuretic, diuretic, and antihypertensive effects are generally considered weak.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Metabolism
Primarily metabolized to the sulfate conjugate of hydroxytriamterene
Excretion
Urine (21% to <50%; primarily as metabolites)
Onset of Action
Diuresis: 2 to 4 hours; Note: Maximum therapeutic effect may not occur until after several days of therapy
Time to Peak
Plasma: ~3 hours
Duration of Action
Diuresis: 7 to 9 hours
Use: Labeled Indications
Edema: Treatment of edema associated with congestive heart failure, cirrhosis of the liver and the nephrotic syndrome; also in steroid-induced edema, idiopathic edema and edema due to secondary hyperaldosteronism.
Use: Off Label
Hypertension (alternative agent)yes
Based on the 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults, potassium-sparing diuretics may be considered in combination with a thiazide diuretic in hypertensive patients with hypokalemia receiving thiazide monotherapy. Potassium-sparing diuretics are not recommended for the initial treatment of hypertension and should not be used as monotherapy.
Contraindications
Hypersensitivity to triamterene or any component of the formulation; anuria; severe or progressive kidney disease or dysfunction with the possible exception of nephrosis; severe hepatic disease; hyperkalemia; coadministration with other potassium-sparing agents or other formulations containing triamterene
Dosage and Administration
Dosing: Adult
Edema: Oral: Initial: 100 mg twice daily; titrate as need based on patient response; maximum: 300 mg/day
Hypertension (off-label use) (alternative agent): Oral: 50 to 100 mg/day in 1 or 2 divided doses (ACC/AHA [Whelton 2017]). Note: Typically used as combination therapy with thiazide diuretics to prevent hypokalemia; minimal antihypertensive effect as monotherapy.
Dosing: Geriatric
Refer to adult dosing. In the management of hypertension, consider lower initial doses and titrate to response (Aronow 2011).
Dosing: Pediatric
Edema: Children and Adolescents: Limited data available: Oral: 1 to 4 mg/kg/day divided into 1 to 2 doses; maximum daily dose: 6 mg/kg/day or 300 mg/day, whichever is lower (Kliegman 2007; van der Vorst 2006)
Hypertension: Limited data available: Children and Adolescents: Oral: Initial: 0.5 to 1 mg/kg/dose twice daily; maximum daily dose: 3 to 4 mg/kg/day or 300 mg/day, whichever is lower (NHLBI 2004; NHLBI 2011)
Administration
Oral: Administer after meals.
Storage
Store at 25°C (77°F); excursions permitted to between 15°C and 30°C (59°F and 86°F). Protect from light.
Triamterene Images
Drug Interactions
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Ammonium Chloride: Potassium-Sparing Diuretics may enhance the adverse/toxic effect of Ammonium Chloride. Specifically the risk of systemic acidosis. Consider therapy modification
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Angiotensin II Receptor Blockers: May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Potassium-Sparing Diuretics may enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Cardiac Glycosides: Potassium-Sparing Diuretics may diminish the therapeutic effect of Cardiac Glycosides. In particular, the inotropic effects of digoxin appear to be diminished. Potassium-Sparing Diuretics may increase the serum concentration of Cardiac Glycosides. This particular effect may be unique to Spironolactone. Monitor therapy
CycloSPORINE (Systemic): Potassium-Sparing Diuretics may enhance the hyperkalemic effect of CycloSPORINE (Systemic). Avoid combination
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diacerein: May enhance the therapeutic effect of Diuretics. Specifically, the risk for dehydration or hypokalemia may be increased. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dofetilide: Triamterene may increase the serum concentration of Dofetilide. Monitor therapy
Drospirenone: May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Eplerenone: May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Management: This combination is contraindicated in patients receiving eplerenone for treatment of hypertension. Consider therapy modification
Heparin: May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Management: Monitor serum potassium concentrations closely. The spironolactone Canadian product monograph lists its combination with heparin or low molecular weight heparins as contraindicated. Monitor therapy
Heparins (Low Molecular Weight): May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Management: Monitor serum potassium concentrations closely. The spironolactone Canadian product monograph lists its combination with heparin or low molecular weight heparins as contraindicated. Monitor therapy
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Indomethacin: May enhance the nephrotoxic effect of Triamterene. Management: Consider alternatives to concomitant treatment with triamterene and indomethacin. If the combination cannot be avoided, monitor for development of renal failure. Consider therapy modification
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May diminish the antihypertensive effect of Potassium-Sparing Diuretics. Nonsteroidal Anti-Inflammatory Agents may enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Opioid Agonists: May enhance the adverse/toxic effect of Diuretics. Opioid Agonists may diminish the therapeutic effect of Diuretics. Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Potassium Salts: May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Consider therapy modification
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
QuiNIDine: Potassium-Sparing Diuretics may diminish the therapeutic effect of QuiNIDine. Monitor therapy
Sodium Phosphates: Diuretics may enhance the nephrotoxic effect of Sodium Phosphates. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with diuretics, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, hydrate adequately and monitor fluid and renal status. Consider therapy modification
Spironolactone: Triamterene may enhance the hyperkalemic effect of Spironolactone. Avoid combination
Tacrolimus (Systemic): Potassium-Sparing Diuretics may enhance the hyperkalemic effect of Tacrolimus (Systemic). Monitor therapy
Tolvaptan: May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Test Interactions
Interferes with fluorometric assay of quinidine; may lead to false-negative aldosterone/renin ratio (ARR) (Funder 2016)
Adverse Reactions
Frequency not defined.
Central nervous system: Dizziness, fatigue, headache
Dermatologic: Skin photosensitivity, skin rash
Endocrine & metabolic: Hyperkalemia, hypokalemia, increased uric acid, metabolic acidosis
Gastrointestinal: Diarrhea, nausea, vomiting, xerostomia
Genitourinary: Azotemia
Hematologic & oncologic: Hematologic abnormality, megaloblastic anemia, thrombocytopenia
Hepatic: Jaundice, liver enzyme disorder
Hypersensitivity: Anaphylaxis
Neuromuscular & skeletal: Weakness
Renal: Acute interstitial nephritis (rare), acute renal failure (rare), increased blood urea nitrogen, increased serum creatinine, nephrolithiasis
Warnings/Precautions
Concerns related to adverse effects:
- Fluid/electrolyte loss: Triamterene can lead to profound diuresis with fluid and electrolyte loss; close medical supervision and dose evaluation are required. Patients with heart failure, renal disease, or cirrhosis may be particularly susceptible to fluid and electrolyte abnormalities. Watch for and correct electrolyte disturbances; adjust dose to avoid dehydration.
- Hyperkalemia: [US Boxed Warning]: Hyperkalemia can occur; patients at risk include those with renal impairment, diabetes, the elderly, and the severely ill. Serum potassium levels must be monitored at frequent intervals especially when dosages are changed or with any illness that may cause renal dysfunction. . In patients who develop hyperkalemia or if hyperkalemia is suspected, obtain an electrocardiogram to rule out hyperkalemia-induced QRS prolongation or other cardiac arrhythmias. Discontinue triamterene and any potassium supplementation in patients who develop hyperkalemia; treat cardiac arrhythmias as clinically indicated.
- Hypersensitivity reactions: Isolated occurrences have been reported. Observe for blood dyscrasias, liver damage or idiosyncratic reactions
- Photosensitivity: Can cause photosensitivity.
Disease-related concerns:
- Adrenal insufficiency: Avoid use of diuretics for treatment of elevated blood pressure in patients with primary adrenal insufficiency (Addison disease). Adjustment of glucocorticoid/mineralocorticoid therapy and/or use of other antihypertensive agents is preferred to treat hypertension (Bornstein 2016; Inder 2015).
- Diabetes: Use with caution in patients with prediabetes or diabetes mellitus; may increase blood glucose concentrations and necessitate dosage adjustment of hypoglycemic agents.
- Gout: May cause elevation in uric acid.
- Hepatic impairment: Use with caution in patients with severe hepatic dysfunction; in cirrhosis, avoid electrolyte and acid/base imbalances that might lead to hepatic encephalopathy.
- Kidney stones: Use with caution in patients with kidney stones.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Abrupt discontinuation: In patients who have received triamterene for prolonged periods of time, a hypothetical risk of rebound kaliuresis may occur when abruptly discontinued; withdraw triamterene gradually in these patients.
Monitoring Parameters
Blood pressure; serum electrolytes (especially potassium), renal function; weight, I & O
Hypertension: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (ACC/AHA [Whelton 2017]):
Confirmed hypertension and known CVD or 10-year ASCVD risk ≥10%: Target blood pressure <130/80 mm Hg is recommended
Confirmed hypertension without markers of increased ASCVD risk: Target blood pressure <130/80 mm Hg may be reasonable
Pregnancy
Pregnancy Considerations
Triamterene crosses the placenta and is found in cord blood. Use of triamterene to treat edema during normal pregnancies is not appropriate; use may be considered when edema is due to pathologic causes (as in the nonpregnant patient); monitor.
Patient Education
What is this drug used for?
- It is used to get rid of extra fluid.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Fatigue
- Dizziness
- Headache
- Diarrhea
- Dry mouth
- Nausea
- Vomiting
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Fluid and electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, severe dizziness, passing out, fast heartbeat, increased thirst, seizures, loss of strength and energy, lack of appetite, unable to pass urine or change in amount of urine passed, dry mouth, dry eyes, or nausea or vomiting
- Kidney stone like back pain, abdominal pain, or blood in the urine
- Infection
- Bruising
- Bleeding
- Severe loss in strength and energy
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.