Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Oral, as hydrochloride:
Generic: 0.4 mg/mL (473 mL)
Tablet, Oral, as hydrochloride:
Generic: 2 mg, 5 mg
Pharmacology
Mechanism of Action
Exerts a direct inhibitory effect on the parasympathetic nervous system. It also has a relaxing effect on smooth musculature; exerted both directly on the muscle itself and indirectly through parasympathetic nervous system (inhibitory effect)
Pharmacokinetics/Pharmacodynamics
Metabolism
Hydroxylation of the alicyclic groups (Brocks 1999)
Excretion
Urine and bile (Brocks 1999)
Time to Peak
Serum: 1.3 hours (Brocks 1999)
Half-Life Elimination
33 hours (Brocks 1999)
Use: Labeled Indications
Drug-induced extrapyramidal symptoms (treatment): Aid in the control of extrapyramidal symptoms caused by CNS drugs (eg, dibenzoxazepines, phenothiazines, thioxanthenes, butyrophenones)
Parkinsonism: Treatment of all forms of parkinsonism (postencephalitic, arteriosclerotic, and idiopathic) as adjunctive therapy
Contraindications
Hypersensitivity to trihexyphenidyl or any component of the formulation; narrow angle glaucoma.
Dosage and Administration
Dosing: Adult
Drug-induced extrapyramidal symptoms (treatment): Note: Prophylactic use is generally not recommended to prevent antipsychotic-associated extrapyramidal symptoms (EPS); consider individual preferences, history of EPS, and baseline risk factors for EPS, including antipsychotic receptor binding and adverse effect profile (Kreyenbuhl 2009).
Oral: Initial: 1 mg/day; increase as necessary to usual range: 5 to 15 mg/day in 3 to 4 divided doses
Parkinsonism: Oral: Initial: 1 mg/day, increase by 2 mg increments at intervals of 3 to 5 days; usual dose: 6 to 10 mg/day in 3 to 4 divided doses; doses of 12 to 15 mg/day may be required
Use in combination with levodopa: When trihexyphenidyl is used concomitantly with levodopa, the usual dose of each may need to be reduced. Usual range: 3 to 6 mg/day in divided doses
Dosing: Geriatric
Avoid use (Beers Criteria [AGS 2019]).
Dosing: Pediatric
Dystonia in cerebral palsy: Limited data available: Children and Adolescents: Oral: Initial: 0.1 to 0.2 mg/kg/day in 2 to 3 divided doses; after the first week, titrate weekly or every 2 weeks as tolerated (eg, increase by 0.15 mg/kg/day or increase by 10% to 20%) (Ben-Pazi 2011; Carranza-del Rio 2011; Rice 2009; Sanger 2007). Usual maximum daily dose: 0.75 mg/kg/day in 3 divided doses (Sanger 2007). Doses as high as 2.6 mg/kg/day in 3 divided doses have been described (Rice 2009).
Administration
Oral: May be administered before or after meals (if excessive dry mouth develops, consider administering before meals unless it causes nausea; postencephalitic patients who are prone to excessive salivation may prefer to take after meals); tolerated best if given in 3 daily doses and with food. High doses (>10 mg/day) may be divided into 4 doses (at each meal and at bedtime).
Dietary Considerations
May be taken before or after meals; tolerated best if given with food.
Storage
Store at 20°C to 25°C (68°F to 77°F).
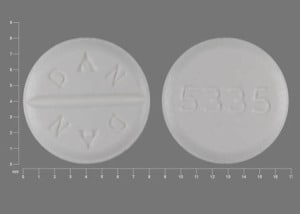
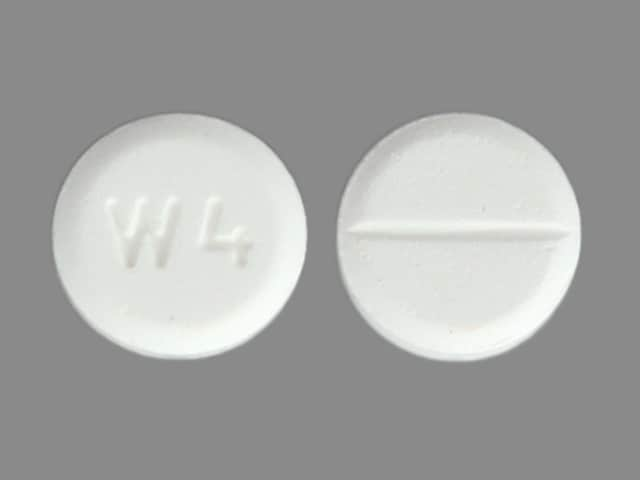
Trihexyphenidyl Images
Drug Interactions
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Amantadine: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Cannabinoid-Containing Products: Anticholinergic Agents may enhance the tachycardic effect of Cannabinoid-Containing Products. Exceptions: Cannabidiol. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Opioid Agonists: Anticholinergic Agents may enhance the adverse/toxic effect of Opioid Agonists. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Adverse Reactions
Frequency not defined.
Cardiovascular: Tachycardia
Central nervous system: Agitation, confusion, delusions, dizziness, drowsiness, euphoria, hallucination, headache, nervousness, paranoia, psychiatric disturbance
Dermatologic: Skin rash
Gastrointestinal: Constipation, intestinal obstruction, nausea, parotitis, toxic megacolon, vomiting, xerostomia
Genitourinary: Urinary retention
Neuromuscular & skeletal: Weakness
Ophthalmic: Blurred vision, glaucoma, increased intraocular pressure, mydriasis
Warnings/Precautions
Concerns related to adverse effects:
- Anhidrosis/hyperthermia: May cause anhidrosis and hyperthermia. Severe anhidrosis and fatal hyperthermia have occurred; use with caution in hot weather or during exercise, especially when administered concomitantly with other anticholinergic drugs to chronically ill patients, alcoholics, patients with CNS disease, or persons doing manual labor in a hot environment.
- Anticholinergic effects: May cause anticholinergic effects (constipation, xerostomia, blurred vision, urinary retention); monitor patients on long-term use.
- CNS effects: May impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving).
- Ocular effects: May precipitate angle closure with an increase in intraocular pressure. If blurring of vision occurs, consider the possibility of narrow angle glaucoma; blindness because of aggravation of narrow angle glaucoma has been reported. Patients should have a gonioscope evaluation prior to initiation of therapy and close monitoring of IOP.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with cardiovascular disease, including hypertension.
- GI obstruction: Use with caution in patients with obstructive disease of the GI tract.
- Glaucoma: Use with caution in patients with glaucoma. Contraindicated in patients with narrow angle glaucoma; blindness after long-term use because of narrow angle glaucoma has been reported.
- Hepatic impairment: Use with caution in patients with hepatic impairment.
- Prostatic hyperplasia/urinary stricture: Use with caution in patients with prostatic hyperplasia and/or urinary stricture or retention.
- Psychiatric effects: May impair memory and further exacerbate cognitive deficits in elderly patients; in high doses may cause confusion, delirium, and hallucinations (Holloman 1997; Tonda 1994).
- Renal impairment: Use with caution in patients with renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Discontinuation of therapy: Dose reduction or discontinuation of trihexyphenidyl has been associated with neuroleptic malignant syndrome (NMS), exacerbation of Parkinsonism, and withdrawal symptoms including tension, irritability, perspiration, palpitations, headache, insomnia, abdominal distress, anorexia, faint or choking feelings, nausea, and photophobia (McInnis 1985). According to the manufacturer's labeling, withdraw trihexyphenidyl gradually; abrupt or rapid discontinuation may result in acute exacerbation of symptoms or side effects (Manos 1981a; Manos 1981b).
- Tardive dyskinesia: Not recommended for use in patients with tardive dyskinesia unless concomitant Parkinson disease or tardive dystonia exists (Kang 1986); trihexyphenidyl does not relieve symptoms of tardive dyskinesia and may potentially exacerbate symptoms.
Monitoring Parameters
Gonioscopic evaluations (prior to therapy initiation); IOP (periodically); anticholinergic adverse reactions (patients on long-term therapy)
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Animal reproduction studies have not been conducted. One case report did not show evidence of adverse events after trihexyphenidyl administration during pregnancy (Robottom 2011).
Patient Education
What is this drug used for?
- It is used to treat Parkinson disease.
- It is used to treat side effects caused by some other drugs.
Frequently reported side effects of this drug
- Blurred vision
- Dizziness
- Trouble sleeping
- Weight loss
- Fatigue
- Headache
- Anxiety
- Dry mouth
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Sensing things that seem real but are not
- Agitation
- Behavioral changes
- Confusion
- Trouble with memory
- Severe nausea
- Severe vomiting
- Difficult urination
- Fast heartbeat
- Severe constipation
- Severe abdominal pain
- Muscle weakness
- Trouble controlling body movements
- Vision changes
- Eye pain
- Severe eye irritation
- Lack of sweat
- Enlarged pupils
- Neuroleptic malignant syndrome like fever, muscle cramps or stiffness, dizziness, very bad headache, confusion, change in thinking, fast heartbeat, abnormal heartbeat, or sweating a lot
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.