Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral:
Actigall: 300 mg [DSC]
Actigall: 300 mg [contains corn starch]
Generic: 300 mg
Tablet, Oral:
Urso 250: 250 mg
Urso Forte: 500 mg [scored]
Generic: 250 mg, 500 mg
Pharmacology
Mechanism of Action
Decreases the cholesterol content of bile and bile stones by reducing the secretion of cholesterol from the liver and the fractional reabsorption of cholesterol by the intestines. Mechanism of action in primary biliary cirrhosis is not clearly defined.
Pharmacokinetics/Pharmacodynamics
Absorption
90%
Metabolism
Undergoes extensive enterohepatic recycling; following hepatic conjugation and biliary secretion, the drug is hydrolyzed to active ursodiol, where it is recycled or transformed to lithocholic acid by colonic microbial flora; during chronic administration, ursodiol becomes a major biliary and plasma bile acid constituting 30% to 50% of biliary and plasma bile acids
Excretion
Feces; urine (<1%)
Protein Binding
~70%
Use: Labeled Indications
Gallstones (capsules only):
Treatment of patients with radiolucent, noncalcified gallbladder stones less than 20 mm in greatest diameter in whom elective cholecystectomy would be undertaken except for the presence of increased surgical risk caused by systemic disease, advanced age, idiosyncratic reaction to general anesthesia, or for those patients who refuse surgery. Safety for use of ursodiol beyond 24 months is not established.
Prevention of gallstone formation in obese patients experiencing rapid weight loss.
Primary biliary cirrhosis (tablets only): Treatment of patients with primary biliary cirrhosis (PBC).
Use: Off Label
Gallstone prevention post-bariatric surgerybyes
Data from a meta-analysis evaluating retrospective and uncontrolled studies as well as randomized controlled trials support the use of ursodiol for reducing the incidence of gallstone formation and the need for urgent cholecystectomy after bariatric surgery-induced rapid weight loss Magouliotis 2017.
Based on the American Association of Clinical Endocrinologists, The Obesity Society, and the American Society for Metabolic and Bariatric Surgery guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient, ursodiol may be considered after bariatric surgery in patients who have not had a cholecystectomy.
Contraindications
Hypersensitivity to ursodiol or any component of the formulation; not to be used with calcified cholesterol stones, radiopaque stones, or radiolucent bile pigment stones; patients with unremitting acute cholecystitis, cholangitis, biliary obstruction, gallstone pancreatitis, or biliary-gastrointestinal fistula; allergy to bile acids
Canadian labeling: Additional contraindications (not in US labeling): Complete biliary obstruction of extrahepatic origin; widespread intrahepatic obstruction
Dosage and Administration
Dosing: Adult
Gallstone dissolution (Actigall): Oral: 8 to 10 mg/kg/day in 2 to 3 divided doses; use beyond 24 months is not established
Gallstone prevention post-bariatric surgery (off-label use): Oral: 500 to 600 mg once daily or in 2 divided doses for 6 months. Note: Doses up to 1,200 mg/day were effective but were associated with a higher incidence of nonadherence (Magouliotis 2017).
Gallstone prevention (Actigall): Oral: 300 mg twice daily
Primary biliary cirrhosis (Urso, Urso Forte): Oral: 13 to 15 mg/kg/day in 2 to 4 divided doses (with food). Note: May be given once daily (at bedtime) to improve compliance (AASLD [Lindor 2019]).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Biliary atresia, status post-Kasai procedure: Limited data available: Infants and Children: Oral: 10 to 20 mg/kg/day in 2 to 3 divided doses. Dosing based on small prospective and retrospective trials that included ursodiol as part of a multidrug regimen designed to reduce the risk of cholangitis (Kelly 2007; Meyers 2003; Nittono 1989; Stringer 2007; Yamashiro 1994).
Pruritus secondary to cholestasis: Limited data available: Infants, Children, and Adolescents: Oral: 15 to 20 mg/kg/day once daily or in divided doses twice daily; doses up to 30 mg/kg/day may be necessary in some patients (Dinler 1999; Narkewicz 1998; Kliegman 2016). Dosing based on long-term (2.5 years), open-label, crossover trial of 13 patients (ages 2 to 27 years) with intrahepatic cholestasis; six of the 13 patients had symptomatic improvement in pruritus (Narkewicz 1998). In another study of 24 pediatric patients (1.5 to 15 years) treated with ursodiol, all patients experienced improvement in pruritus and 16.7% had complete resolution of pruritus (Dinler 1999).
Cystic fibrosis-related liver disease: Limited data available: Infants, Children, and Adolescents: Oral: Limited data available: Initial: 20 mg/kg/day in 2 divided doses, reported range: 10 to 30 mg/kg/day in divided doses; individualize dose based on patient response (Columbo 1990; Debray 2011; Lepage 1997; Sokol 1999)
Parenteral nutrition-induced cholestasis, treatment: Limited data available: Infants and Children: Oral: 30 mg/kg/day in 3 divided doses (Chen 2004; De Marco 2006; Spagnuolo 1996)
Extemporaneously Prepared
60 mg/mL Oral Suspension (ASHP Standard Concentration) (ASHP 2017)
A 60 mg/mL ursodiol oral suspension may be made with capsules. Empty the contents of twelve 300 mg capsules into a mortar. Add small portions of glycerin and mix to a uniform paste; mix while adding simple syrup in incremental proportions to almost 60 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 60 mL. Label "shake well" and "refrigerate". Stable for 35 days refrigerated (Johnson 1995).
Johnson CE, Nesbitt J. Stability of ursodiol in an extemporaneously compounded oral liquid. Am J Health Syst Pharm. 1995;52(16):1798-1800.8528836
20 mg/mL Oral Suspension
A 20 mg/mL ursodiol oral suspension may be made with capsules and either a 1:1 mixture of Ora-Sweet and Ora-Plus or a 1:1 mixture of methylcellulose 1% and syrup NF. Empty the contents of seventeen 300 mg capsules into a mortar. Add small portions of the chosen vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 255 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 255 mL. Label "shake well" and "refrigerate". Stable for 91 days refrigerated (Nahata 1999).
Nahata MC, Morosco RS, Hipple TF. Stability of ursodiol in two extemporaneously prepared oral suspensions. J Appl Ther Res. 1999;2:221-224.
25 mg/mL Oral Suspension
A 25 mg/mL ursodiol oral suspension may be made with capsules. Empty the contents of ten 300 mg capsules into a mortar; add 10 mL Glycerin, USP and mix until smooth. Mix while adding 60 mL Ora-Plus; transfer mixture to a light-resistant bottle, rinse mortar with a small amount of Orange Syrup, NF, and add quantity of syrup sufficient to make 120 mL. Label "shake well". Stable for 60 days at room temperature or refrigerated (Mallett 1997).
Mallett MS, Hagan RL, Peters DA. Stability of ursodiol 25 mg/mL in an extemporaneously prepared oral liquid. Am J Health Syst Pharm. 1997;54(12):1401-1404.9194984
50 mg/mL Oral Suspension
A 50 mg/mL ursodiol oral suspension may be made with tablets and 60 mL of either a 1:1 mixture of Ora-Plus and strawberry syrup or a 1:1 mixture of Ora-Plus and Ora-Sweet SF. Crush twelve 250 mg tablets in a mortar and reduce to a fine powder. Add small portions of the chosen vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 60 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 60 mL. Label "shake well" and "refrigerate". Stable for 90 days refrigerated (Johnson 2002).
Johnson CE, Streetman DD. Stability of oral suspensions of ursodiol made from tablets. Am J Health Syst Pharm. 2002;59(4):361-363.11885400
Administration
Oral: Do not administer with aluminum-based antacids or bile acid sequestrants. If aluminum-based antacids are needed, administer 2 hours after ursodiol; some experts recommend administering ursodiol 1 hour prior to or 4 to 5 hours after bile acid sequestrants (AASLD [Lindor 2019]; Rust 2000). Urso Forte can be split into halves for appropriate dosage; do not chew. Urso and Urso Forte should be taken with food.
Dietary Considerations
Urso and Urso Forte should be taken with food.
Storage
Actigall: Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Urso: Store at 20°C to 25°C (68°F to 77°F).
Urso Forte: Store at 20°C to 25°C (68°F to 77°F). When broken in half, scored Urso Forte 500 mg tablets maintain quality for up to 28 days when kept in current packaging and stored at 20°C to 25°C (68°F to 77°F). Split tablets should be stored separately from whole tablets due to bitter taste.
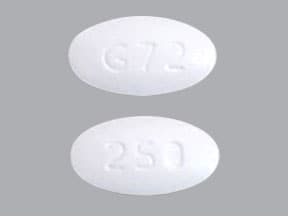
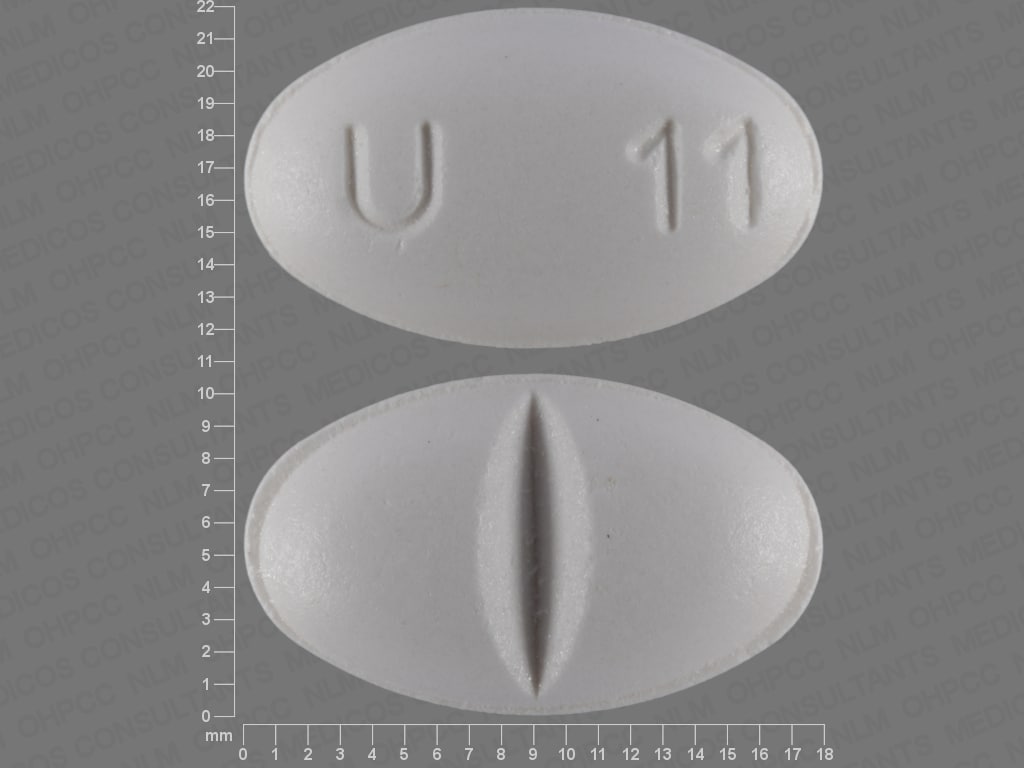
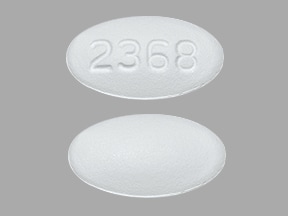
Ursodiol Images
Drug Interactions
Aluminum Hydroxide: May decrease the serum concentration of Ursodiol. Management: Consider administration of ursodiol 2 hours before or 6 hours after aluminum-containing antacid products to prevent adsorption in the gastrointestinal tract. Consider therapy modification
Bile Acid Sequestrants: May decrease the serum concentration of Ursodiol. Management: Administer ursodiol 2 to 4 hours before or at least 2 to 5 hours after bile acid sequestrants to minimize the potential for any significant interaction. Monitor for decreased therapeutic effects of ursodiol in patients receiving bile acid sequestrants. Consider therapy modification
Estrogen Derivatives: May diminish the therapeutic effect of Ursodiol. Monitor therapy
Fibric Acid Derivatives: May diminish the therapeutic effect of Ursodiol. Monitor therapy
Nitrendipine: Ursodiol may decrease the absorption of Nitrendipine. Management: Consider therapeutic alternatives. If concomitant therapy cannot be avoided, avoid simultaneous administration. Consider therapy modification
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Adverse Reactions
>10%:
Central nervous system: Headache (≤25%), dizziness (17%)
Gastrointestinal: Diarrhea (≤27%), constipation (≤26%), dyspepsia (≤17%), nausea (≤17%)
Neuromuscular & skeletal: Back pain (≤12%)
Respiratory: Upper respiratory tract infection (≤16%)
1% to 10%:
Dermatologic: Alopecia (5%), skin rash (3%)
Endocrine & metabolic: Hyperglycemia (1%)
Gastrointestinal: Vomiting (≤10%), peptic ulcer (1%)
Genitourinary: Urinary tract infection (7%)
Hematologic & oncologic: Leukopenia (3%), thrombocytopenia (1%)
Hepatic: Cholecystitis (5%)
Hypersensitivity: Hypersensitivity reaction (5%)
Infection: Viral infection (9%)
Neuromuscular & skeletal: Arthritis (6%), musculoskeletal pain (6%)
Renal: Increased serum creatinine (1%)
Respiratory: Pharyngitis (≤8%), bronchitis (7%), cough (7%), flu-like symptoms (7%)
<1%, postmarketing, and/or case reports: Abdominal distress, abdominal pain, abnormal hepatic function tests, angioedema, anorexia, biliary colic, esophagitis, facial edema, fever, hepatobiliary disease, increased gamma-glutamyl transferase, increased liver enzymes, increased serum alkaline phosphatase, increased serum ALT, increased serum AST, increased serum bilirubin, jaundice, laryngeal edema, malaise, metallic taste, myalgia, peripheral edema, pruritus, transaminases increased, urticaria, weakness
Warnings/Precautions
Concerns related to adverse effects:
- Biliary obstruction: Maintain bile flow during therapy to prevent biliary obstruction.
Disease-related concerns:
- Hepatic effects: Use with caution in patients with chronic liver disease; monitor liver function tests monthly for the first 3 months, and every 6 months thereafter or as clinically necessary. Discontinuation of therapy may be necessary with significant elevations in liver function tests.
Other warnings/precautions:
- Appropriate use: Gallbladder stone dissolution may take several months of therapy; complete dissolution may not occur and recurrence of stones within 5 years has been observed in up to 50% of patients. Patients should be cautiously selected for therapy, consider alternative treatments. Specific treatments should be initiated in patients with ascites, hepatic encephalopathy, variceal bleeding, or if an urgent liver transplant is necessary.
- Nonvisualizing gallbladder: Use with caution in patients with a nonvisualizing gallbladder; therapy should be discontinued if gallbladder nonvisualization occurs during treatment.
Monitoring Parameters
Gallstone disease: ALT, AST, sonogram
Primary biliary cirrhosis: Monitor liver function tests (GGT, AST, ALT, bilirubin, and alkaline phosphatase) monthly for the first 3 months and every 6 months thereafter or as clinically necessary (90% of the improvement usually occurs within 6 to 9 months) ([Lindor 2019]); baseline vitamin D level (Guo 2015)
Pregnancy
Pregnancy Considerations
Adverse events have not been observed in animal reproduction studies. Ursodiol (ursodeoxycholic acid) is the treatment of choice for intrahepatic cholestasis of pregnancy (Kremer 2011).
Patient Education
What is this drug used for?
- It is used to treat or prevent gallstones.
- It is used to treat a type of liver disease caused by bile duct problems in the liver (biliary cirrhosis).
Frequently reported side effects of this drug
- Dizziness
- Headache
- Back pain
- Nausea
- Vomiting
- Constipation
- Muscle pain
- Joint pain
- Common cold symptoms
- Hair loss
- Diarrhea
- Abdominal pain
- Heartburn
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.