What is Versacloz?
Versacloz is a prescription antipsychotic medicine used to treat people with certain types of schizophrenia, including people who:
- are not helped by other schizophrenia medicines
- have been suicidal and may be at risk of suicidal behavior again
It is not known if Versacloz is safe and effective in children.
What is the most important information I should know about Versacloz?
Versacloz can cause serious side effects, including:
1. Severe neutropenia, a blood disorder that can lead to serious infections and death. Severe neutropenia means that you do not have enough of certain white blood cells to fight infection. Tell your healthcare provider right away if you have any of the following symptoms or signs of neutropenia or infection:
- Skin, throat, urinary tract, vaginal, pneumonia, or any other infection
- Fever or chills
- Sores or ulcers inside your mouth, gums or on your skin
- Wounds that take a long time to heal
- Feel like you have the flu
- Pain or burning while urinating
- Unusual vaginal discharge or itching
- Abdominal pain
- Sores or pain in or around your rectal area
- Feel extremely tired or weak
If you have symptoms of severe neutropenia or infection you will need to have a blood test right away to check if Versacloz is causing your symptoms. You must have frequent blood tests while taking Versacloz so your healthcare provider can make sure you are not getting severe neutropenia or infection.
Versacloz is available only through a restricted program called the Clozapine REMS Program. This program makes sure that you will receive each refill of Versacloz only if you have a blood test and your blood test result is acceptable to your healthcare provider.
During your first 6 months of clozapine treatment, you will have weekly blood tests. If you have not taken clozapine before, you will need weekly blood tests when you first start Versacloz. If you have acceptable blood test results during your first 6 months of clozapine treatment, you can have a blood test every other week for the next 6 months. After a year of acceptable blood test results, you can have blood tests every 4 weeks while you are taking Versacloz.
2. Decreased blood pressure (orthostatic hypotension), slow heart rate (bradycardia), or fainting (syncope) that can lead to death. Lightheadedness or fainting caused by a sudden change in your heart rate and blood pressure when you rise too quickly from a sitting or lying position can happen while you take Versacloz and can be life threatening. These problems may happen more often when you are first starting treatment with Versacloz or when your dose is increased. Tell your healthcare provider right away if you feel faint, lose consciousness, or have symptoms of slow heart rate or an irregular heart rhythm.
3. Seizures. Seizures can occur during Versacloz treatment. Be especially careful while driving or during any other dangerous activity while taking Versacloz.
4. Myocarditis (heart muscle inflammation) and cardiomyopathy (heart muscle weakness) that may lead to death. Symptoms of myocarditis and cardiomyopathy include:
- chest pain
- fast heartbeat
- shortness of breath
- dizziness
- swollen legs, ankles and feet
- feel tired
- fever
5. Higher risk of death in elderly people with memory loss (dementia) or psychosis. Versacloz can increase the risk of death in elderly people who have dementia. Versacloz is not for treating psychosis in elderly people with dementia.
Who should not take Versacloz?
Do not take Versacloz if you:
- have blood problems called neutropenia
- are allergic to clozapine or any of the ingredients in Versacloz. See the end of this Patient Information guide for a complete list of ingredients in Versacloz.
What should I tell my healthcare provider before taking Versacloz?
Before you take Versacloz, tell your healthcare provider about all of your medical conditions, including if you:
- have or have had heart problems or a family history of heart problems including heart attack, heart failure, abnormal heart rhythm, or long QT syndrome
- have or have had liver or kidney problems
- have or have had seizures or epilepsy
- have or have had low levels of potassium or magnesium in your blood
- have diabetes
- have increased pressure in your eyes (glaucoma)
- have had Neuroleptic Malignant Syndrome (NMS)
- have or have had uncontrolled movements of your tongue, face, mouth, or jaw (tardive dyskinesia)
- have or have had diarrhea or constipation
- have or have had an enlarged prostate gland
- smoke tobacco
- plan to stop smoking tobacco while taking Versacloz
- use products containing caffeine
- are pregnant or plan to become pregnant. It is not known if Versacloz will harm your unborn baby. Talk to your healthcare provider if you become pregnant while taking Versacloz.
- If you become pregnant while receiving clozapine, talk to your healthcare provider about registering with the National Pregnancy Registry for Atypical Antipsychotics. You can register by calling 1-866-961-2388 or go to http://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/
- are breastfeeding or plan to breastfeed. Versacloz can pass into your breast milk. Talk to your healthcare provider about the best way to feed your baby if you take Versacloz.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
Versacloz and other medicines may affect each other causing side effects.
Especially tell your healthcare provider if you take:
- chemotherapy, radiation, or other medicines that cause agranulocytosis, neutropenia, low white blood cell count, or affect your bone marrow
- other antipsychotics or other medicines that can affect the amount of clozapine in your blood
- medicines used to treat anxiety, relax your muscles, or help you sleep
- any medicines that make you feel sleepy
- antibiotics
- medicines used to treat heart problems
- medicines used to lower the amount of water in your body (diuretics)
- medicines used for birth control
Ask your healthcare provider for a list of these medicines if you are not sure.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I take Versacloz?
- Read the “Instructions for Use” at the end of this Patient Information for specific information about the right way to use Versacloz.
- Your pharmacist should go over the instructions for how to use Versacloz with you when you receive your first prescription.
- Take Versacloz exactly as your healthcare provider tells you to take it. Talk to your healthcare provider or pharmacist if you are not sure how to take Versacloz.
- Do not change your dose or stop taking Versacloz without talking to your healthcare provider.
The symptoms of Versacloz overdose can include:
- feeling sleepy
- seizures
- confusion
- coma
- fast or irregular heartbeat
- low blood pressure
- shallow or difficult breathing
- having a lot of saliva in your mouth
If you miss a dose of Versacloz for more than 2 days, check with your healthcare provider before starting to take it again to make sure you take the correct dose.
What should I avoid while taking Versacloz?
- You should not drink alcohol while taking Versacloz. It can increase your chances of getting serious side effects.
- Do not drive, operate machinery, swim, climb, or do other dangerous activities until you know how Versacloz affects you.
What are the possible side effects of Versacloz?
Versacloz may cause serious side effects, including:
- See "What is the most important information I should know about Versacloz?"
- severe constipation and bowel problems. You may not feel or be aware of constipation symptoms. Contact your healthcare provider if you are having bowel movements at less than your normal frequency, especially if it is less than three times a week, you have hard or dry stools, or you have difficulty passing gas. Talk with your healthcare provider about ways to prevent constipation. Other symptoms associated with bowel problems include nausea, bloating or stomach swelling, stomach pain, and vomiting.
- high count of a certain white blood cell (eosinophilia)
- problems with your heartbeat. These heart problems can cause death. Call your healthcare provider right away if you have any of these symptoms:
- passing out or feeling like you will pass out
- dizziness
- feeling as if your heart is pounding or missing beats
- high blood sugar (diabetes) and changes in the fat levels in your blood (dyslipidemia)
- Neuroleptic Malignant Syndrome (NMS). NMS is a rare but very serious problem that can happen in people who take Versacloz. NMS can cause death and must be treated in a hospital. Call your healthcare provider right away if you become severely ill and have any of these symptoms:
- high fever
- excessive sweating
- stiff muscles
- confusion
- changes in your breathing, heartbeat and blood pressure
- falls, which may lead to fractures or other injuries
- liver problems. Call your healthcare provider right away if you have any of these symptoms:
- nausea
- vomiting
- loss of appetite
- feel tired
- pain on the right side of your stomach (abdomen)
- yellowing of your skin or the whites of your eyes
- fever. Some people may have a fever that comes and goes while they take Versacloz. This happens more often in the first 3 weeks you take Versacloz. Talk to your healthcare provider if you have a fever.
- blood clot in your lung (pulmonary embolism) or in the veins of your legs (deep-vein thrombosis). Get emergency help right away if you have symptoms of a blood clot including:
- chest pain and shortness of breath
- swelling or pain in your leg, ankle or foot
- warm feeling in the skin of your affected leg
- changes in your skin color such as turning pale or blue
- a problem that includes dry mouth, increased sweating, increased pulse rate and constipation (anticholinergic toxicity)
- problems thinking clearly and moving your body
- uncontrolled movements of your tongue, face, mouth, or jaw (tardive dyskinesia)
- stroke in elderly people (cerebrovascular problems)
The most common side effects of Versacloz include:
- sleepiness or drowsiness
- dizziness
- hearth and blood vessel problems
- fast heartbeat
- passing out (syncope)
- increased sweating
- vision problems
- headache
- shaking movements (tremors)
- low blood pressure
- having a lot of saliva in your mouth
- dry mouth
- stomach and intestinal problems
- nausea
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of Versacloz. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
General information about the safe and effective use of Versacloz
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information Leaflet. Do not use Versacloz for a condition for which it was not prescribed. Do not give Versacloz to other people, even if they have the same symptoms that you have. It may harm them.
This Patient Information Leaflet summarizes the most important information about Versacloz. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for more information about Versacloz that is written for healthcare professionals.
For more information, go to www.VERSACLOZ.com or call 1-800-520-5568.
How should I store Versacloz?
- Store Versacloz at room temperature between 68°F to 77°F (20°C to 25°C).
- Do not refrigerate or freeze Versacloz.
- Protect Versacloz from light.
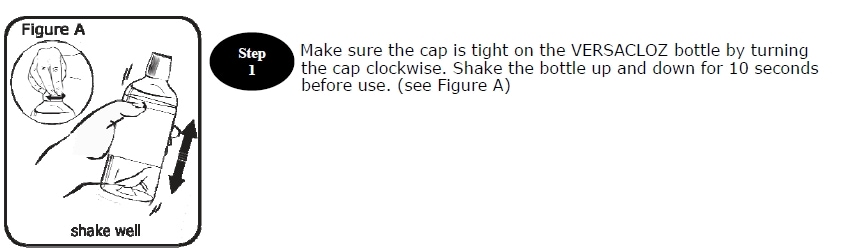
- Shake your Versacloz bottle well for 10 seconds before each use.
Keep Versacloz and all medicines out of the reach of children.
What are the ingredients in Versacloz?
Active ingredient: clozapine
Inactive ingredients: glycerin, sorbitol (crystallizing), sodium dihydrogen phosphate dihydrate, xanthan gum, sodium methylparaben, sodium propylparaben, povidone, water, and sodium hydroxide
Instructions for use for Versacloz
Versacloz (VER sa kloz)
(clozapine)
Oral Suspension
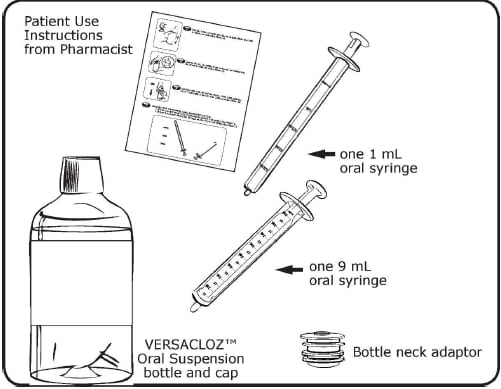
Supplies you will need to take your Versacloz dose:
- Versacloz Oral Suspension bottle
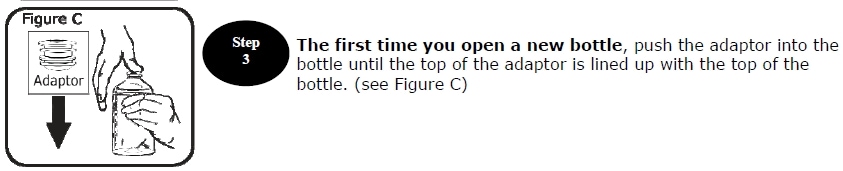
- a bottle neck adaptor
- the correct oral syringe to measure your dose
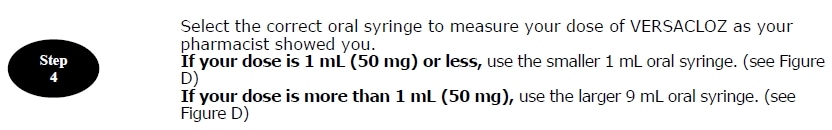
- If your dose is 1 mL (50 mg) or less, use the smaller 1 mL oral syringe.
- If your dose is more than 1 mL (50 mg), use the larger 9 mL oral syringe.
Disposal of your oral syringe, empty Versacloz bottle and bottle neck adaptor:
Place the cap back on the empty Versacloz bottle before you throw it away. The oral syringe, empty bottle and bottle neck adaptor should be placed in your household trash when you finish your bottle of Versacloz. The oral syringe should not be shared with other people or used for medicines other than Versacloz.
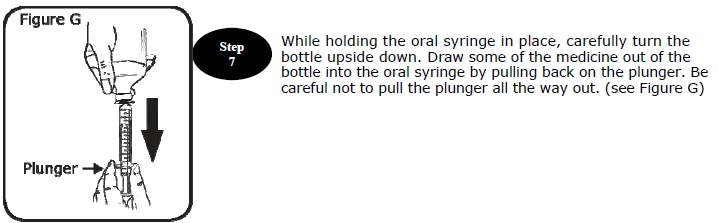
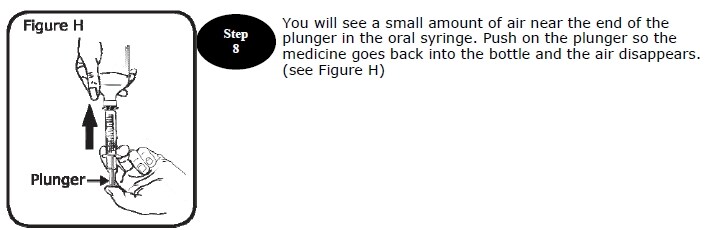
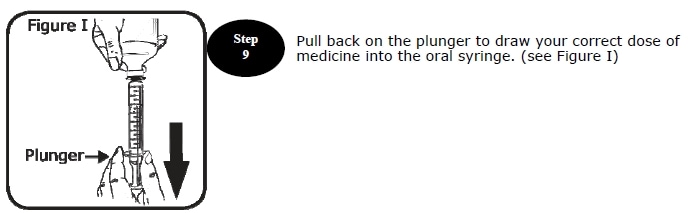
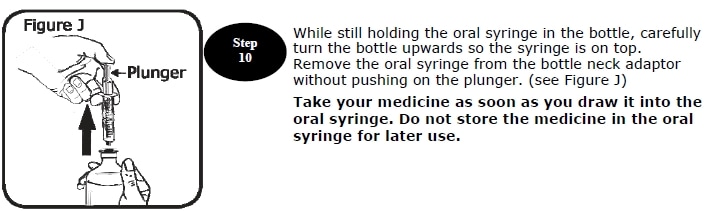
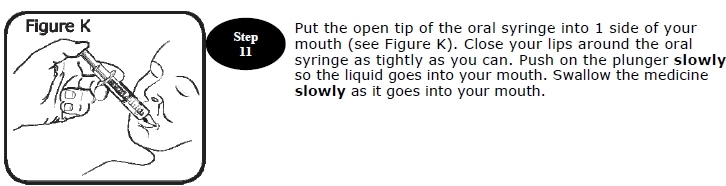
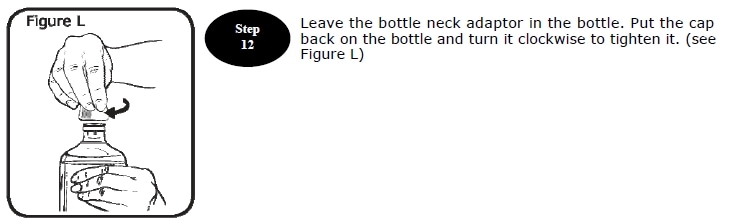
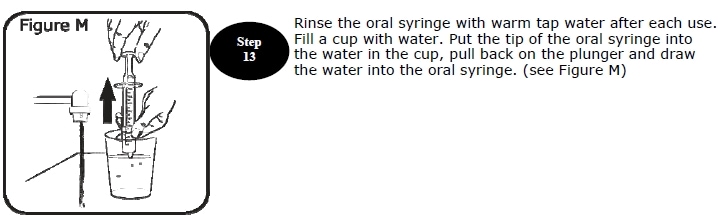
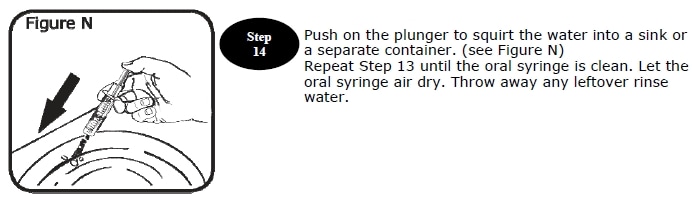
Instructions for use last revised 01/2018.


