Coronaviruses are a family of viruses that can cause illnesses such as the common cold, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). In 2019, a new coronavirus was identified as the cause of a disease outbreak that originated in China.
The virus is known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The disease it causes is called coronavirus disease 2019 (COVID-19). In March 2020, the World Health Organization (WHO) declared the COVID-19 outbreak a pandemic.
Public health groups, including the U.S. Centers for Disease Control and Prevention (CDC) and WHO, are monitoring the COVID-19 pandemic and posting updates on their websites. These groups have also issued recommendations for preventing and treating the virus that causes COVID-19.
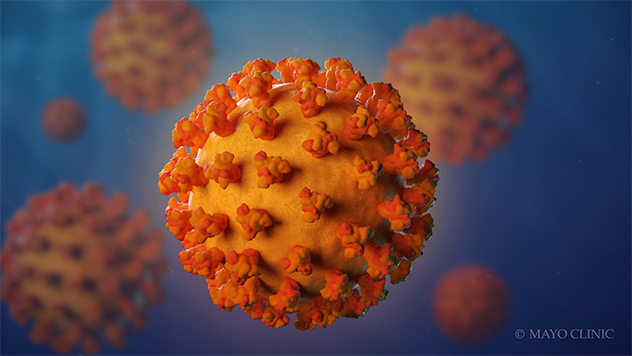
Coronavirus is a family of viruses that can cause respiratory illnesses such as the common cold, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS).
Symptoms
Signs and symptoms of coronavirus disease 2019 (COVID-19) may appear 2 to 14 days after exposure. This time after exposure and before having symptoms is called the incubation period. You can still spread COVID-19 before you have symptoms (presymptomatic transmission). Common signs and symptoms can include:
- Fever
- Cough
- Tiredness
Early symptoms of COVID-19 may include a loss of taste or smell.
Other symptoms can include:
- Shortness of breath or difficulty breathing
- Muscle aches
- Chills
- Sore throat
- Runny nose
- Headache
- Chest pain
- Pink eye (conjunctivitis)
- Nausea
- Vomiting
- Diarrhea
- Rash
This list isn't complete. Children have similar symptoms to adults and generally have mild illness.
The severity of COVID-19 symptoms can range from very mild to severe. Some people may have only a few symptoms. Some people may have no symptoms at all, but can still spread it (asymptomatic transmission). Some people may experience worsened symptoms, such as worsened shortness of breath and pneumonia, about a week after symptoms start.
Some people experience COVID-19 symptoms for more than four weeks after they're diagnosed. These health issues are sometimes called post-COVID-19 conditions. Some children experience multisystem inflammatory syndrome, a syndrome that can affect some organs and tissues, several weeks after having COVID-19. Rarely, some adults experience the syndrome too.
People who are older have a higher risk of serious illness from COVID-19, and the risk increases with age. People who have existing medical conditions also may have a higher risk of serious illness. Certain medical conditions that may increase the risk of serious illness from COVID-19 include:
- Serious heart diseases, such as heart failure, coronary artery disease or cardiomyopathy
- Cancer
- Chronic obstructive pulmonary disease (COPD)
- Type 1 or type 2 diabetes
- Overweight, obesity or severe obesity
- High blood pressure
- Smoking
- Chronic kidney disease
- Sickle cell disease or thalassemia
- Weakened immune system from solid organ transplants or bone marrow transplants
- Pregnancy
- Asthma
- Chronic lung diseases such as cystic fibrosis or pulmonary hypertension
- Liver disease
- Dementia
- Down syndrome
- Weakened immune system from bone marrow transplant, HIV or some medications
- Brain and nervous system conditions, such as strokes
- Substance use disorders
This list is not complete. Other medical conditions may increase your risk of serious illness from COVID-19.
When to see a doctor
If you have COVID-19 signs or symptoms or you've been in contact with someone diagnosed with COVID-19, contact your health care provider right away for medical advice. Your health care provider will likely recommend that you get tested for COVID-19. If you have emergency COVID-19 symptoms, such as trouble breathing, seek care immediately. If you need to go to a hospital, call ahead so that health care providers can take steps to ensure that others aren't exposed.
If you have emergency COVID-19 signs and symptoms, seek care immediately. Emergency signs and symptoms can include:
- Trouble breathing
- Persistent chest pain or pressure
- Inability to stay awake
- New confusion
- Pale, gray or blue-colored skin, lips or nail beds — depending on skin tone
This list isn't complete. Let your health care provider know if you are an older adult or have chronic medical conditions, such as heart disease or lung disease, as you may have a greater risk of becoming seriously ill with COVID-19.
Causes
Infection with severe acute respiratory syndrome coronavirus 2, or SARS-CoV-2, causes coronavirus disease 2019 (COVID-19).
The virus that causes COVID-19 spreads easily among people. Data has shown that the COVID-19 virus spreads mainly from person to person among those in close contact (within about 6 feet, or 2 meters). The virus spreads by respiratory droplets released when someone with the virus coughs, sneezes, breathes, sings or talks. These droplets can be inhaled or land in the mouth, nose or eyes of a person nearby.
Sometimes the COVID-19 virus can spread when a person is exposed to very small droplets or aerosols that stay in the air for several minutes or hours — called airborne transmission.
The virus can also spread if you touch a surface with the virus on it and then touch your mouth, nose or eyes. But the risk is low.
The COVID-19 virus can spread from someone who is infected but has no symptoms. This is called asymptomatic transmission. The COVID-19 virus can also spread from someone who is infected but hasn't developed symptoms yet. This is called presymptomatic transmission.
It's possible to get COVID-19 twice or more, but this is uncommon.
When a virus has one or more new mutations it’s called a variant of the original virus. The omicron (B.1.1.529) variant spreads more easily than the original virus that causes COVID-19 and the delta variant. However, omicron appears to cause less severe disease. People who are fully vaccinated can get breakthrough infections and spread the virus to others. But the COVID-19 vaccines are effective at preventing severe illness. This variant also reduces the effectiveness of some monoclonal antibody treatments. Omicron has a few major offshoots (sublineages), including BA.5 and BA.2.12.1. BA.5 made up about 88% of COVID-19 infections that had genetic sequencing in the U.S. in August, 2022, according to the CDC.
In April, the CDC downgraded the delta variant from a variant of concern to a variant being monitored. This means that the delta variant isn’t currently considered a major public health threat in the U.S.
Risk factors
Risk factors for COVID-19 appear to include:
- Close contact (within 6 feet, or 2 meters) with someone who has COVID-19, especially someone with symptoms
- Being coughed or sneezed on by an infected person
- Being near an infected person when in an indoor space with poor air flow
Complications
Although most people with COVID-19 have mild to moderate symptoms, the disease can cause severe medical complications and lead to death in some people. Older adults or people with existing medical conditions are at greater risk of becoming seriously ill with COVID-19.
Complications can include:
- Pneumonia and trouble breathing
- Organ failure in several organs
- Heart problems
- A severe lung condition that causes a low amount of oxygen to go through your bloodstream to your organs (acute respiratory distress syndrome)
- Blood clots
- Acute kidney injury
- Additional viral and bacterial infections
Prevention
The U.S. Food and Drug Administration (FDA) has given emergency use authorization to some COVID-19 vaccines in the United States. The FDA has approved the Pfizer-BioNTech COVID-19 vaccine, now called Comirnaty, to prevent COVID-19 in people age 16 and older. The FDA has given emergency use authorization to Pfizer-BioNTech COVID-19 vaccines for ages 6 months through 11. The FDA has approved the Moderna vaccine, now called Spikevax, to prevent COVID-19 in people age 18 and older. The FDA has also authorized the Moderna COVID-19 vaccine in children ages 6 months through 17 years old. The FDA has also authorized the Novavax COVID-19, adjuvanted vaccine to prevent COVID-19 in people age 12 and older.
Due to the risk of a potentially life-threatening blood-clotting problem, the FDA is restricting use of the Janssen/Johnson & Johnson vaccine to certain people age 18 and older. Examples include people who had a severe allergic reaction after getting an mRNA COVID-19 vaccine and people who can't get an mRNA COVID-19 vaccine due to limited access or personal or religious concerns. If you get this vaccine, be sure to understand the risks and symptoms of the blood-clotting problem.
A vaccine can prevent you from getting the COVID-19 virus or prevent you from becoming seriously ill if you get the COVID-19 virus. In addition, COVID-19 vaccination might offer better protection than getting sick with COVID-19. A recent study showed that unvaccinated people who already had COVID-19 are more than twice as likely as fully vaccinated people to get reinfected with COVID-19.
After getting vaccinated, you can more safely return to many activities you may not have been able to do because of the pandemic. However, if you are in an area with a high number of people with COVID-19 in the hospital and new COVID-19 cases, the CDC recommends wearing a mask indoors in public. You're considered fully vaccinated two weeks after you get a second dose of an mRNA COVID-19 vaccine, after two doses of the Novavax vaccine, or two weeks after you get a single dose of the Janssen/Johnson & Johnson COVID-19 vaccine. You are considered up to date with your vaccines if you have gotten all recommended COVID-19 vaccines, including booster doses, when you become eligible.
An additional primary dose of a COVID-19 vaccine is recommended for people who are vaccinated and might not have had a strong enough immune response.
In contrast, a booster dose is recommended for people who are vaccinated and whose immune response weakened over time. Research suggests that getting a booster dose can decrease your risk of infection and severe illness with COVID-19.
People who have a moderately or severely weakened immune system should get an additional primary shot and a booster shot.
The CDC recommends additional doses and booster doses of COVID-19 vaccines in specific instances:
-
Additional dose. The CDC recommends a third dose of an mRNA COVID-19 vaccine for some people with weakened immune systems, such as those who have had an organ transplant. People with weakened immune systems might not develop enough immunity after vaccination with two doses of an mRNA COVID-19 vaccine. An additional dose might improve their protection against COVID-19. This recommendation is for people age 5 and older.
The third dose should be given at least 28 days after a second dose of an mRNA COVID-19 vaccine. The additional dose should be the same brand as the other two mRNA COVID-19 vaccine doses you were given. If the brand given isn't known, either brand of mRNA COVID-19 vaccine can be given as a third dose.
-
Booster dose. These recommendations differ by age, what vaccines you have been given and the state of your immune system.
Kids ages 5 through 17 should get a Pfizer-BioNTech COVID-19 booster shot if they been given both doses of the Pfizer-BioNTech COVID-19 vaccine and it’s been at least five months. Currently, booster doses aren’t recommended for any children or teens who get the Moderna COVID-19 vaccine for their first two doses.
If you are age 18 or older, have been given both doses of the Moderna COVID-19 vaccine and it’s been at least 5 months, you should get a single booster dose. The Pfizer-BioNTech or Moderna COVID-19 vaccine boosters are preferred in most situations.
If you are age 18 or older, have been given one dose of the Janssen/Johnson & Johnson COVID-19 vaccine and it’s been at least 2 months, you should get a single booster dose. The Pfizer-BioNTech or Moderna COVID-19 vaccine boosters are preferred in most situations.
Pregnant women may also receive a COVID-19 booster shot.
Kids ages 5 through 17 who have a weakened immune system should get a Pfizer-BioNTech COVID-19 vaccine booster shot if they have been given both doses of the Pfizer-BioNTech COVID-19 vaccine and it’s been at least three months since the additional primary shot.
If you are age 18 or older, have a weakened immune system and had two doses of an mRNA COVID-19 vaccine and an additional primary shot, and it’s been at least two months since the additional shot, get a single booster dose. An mRNA COVID-19 vaccine is preferred.
If you are age 18 and older, have a weakened immune system and had one dose of the Janssen/Johnson & Johnson COVID-19 vaccine and an additional primary shot of an mRNA COVID-19 vaccine, and it’s been at least two months since the additional shot, get a single booster dose. An mRNA COVID-19 vaccine is preferred.
Second booster dose. A second booster dose of an mRNA COVID-19 vaccine is recommended for certain people who have a weakened immune system and people age 50 or older. This second booster dose can be given to those eligible four months after a first booster dose of any authorized or approved COVID-19 vaccine.
A second booster dose of an mRNA COVID-19 is also recommended for people who got two doses of the Janssen/Johnson & Johnson COVID-19 vaccine at least four months ago.
You might consider delaying getting a second booster dose if you had COVID-19 in the past three months or if getting a second booster dose now would make you not want to get another booster in the future.
Kids age 12 and older who have a weakened immune system, got both doses of the Pfizer-BioNTech COVID-19 vaccine and got a single booster dose of the Pfizer-BioNTech COVID-19 vaccine at least four months ago can also get a second booster dose of the Pfizer-BioNTech COVID-19 vaccine.
The FDA has also authorized the monoclonal antibodies tixagevimab and cilgavimab (Evusheld) to prevent COVID-19 in some people with weakened immune systems or a history of severe reactions to a COVID-19 vaccine.
There are many steps you can take to reduce your risk of infection from the COVID-19 virus and reduce the risk of spreading it to others. WHO and CDC recommend following these precautions:
- Get vaccinated. COVID-19 vaccines reduce the risk of getting and spreading COVID-19.
- Avoid close contact (within about 6 feet, or 2 meters) with anyone who is sick or has symptoms.
- Keep distance between yourself and others (within about 6 feet, or 2 meters) when you're in indoor public spaces if you're not fully vaccinated. This is especially important if you have a higher risk of serious illness. Keep in mind some people may have COVID-19 and spread it to others, even if they don't have symptoms or don't know they have COVID-19.
- Avoid crowds and indoor places that have poor air flow (ventilation).
- Wash your hands often with soap and water for at least 20 seconds, or use an alcohol-based hand sanitizer that contains at least 60% alcohol.
- Wear a face mask in indoor public spaces if you're in an area with a high number of people with COVID-19 in the hospital and new COVID-19 cases, whether or not you're vaccinated. The CDC recommends wearing the most protective mask possible that you'll wear regularly, fits well and is comfortable.
- Improve the air flow indoors. Open windows. Turn on fans to direct air out of windows. If you can't open windows, consider using air filters. And turn on exhaust fans in your bathroom and kitchen. You might also consider a portable air cleaner.
- Cover your mouth and nose with your elbow or a tissue when you cough or sneeze. Throw away the used tissue. Wash your hands right away.
- Avoid touching your eyes, nose and mouth.
- Avoid sharing dishes, glasses, towels, bedding and other household items if you're sick.
- Clean and disinfect high-touch surfaces, such as doorknobs, light switches, electronics and counters, regularly.
- Stay home from work, school and public areas and stay home in isolation if you're sick, unless you're going to get medical care. Avoid public transportation, taxis and ride-hailing services if you're sick.
If you have a chronic medical condition and may have a higher risk of serious illness, check with your doctor about other ways to protect yourself.
Travel
If you're planning to travel, first check the CDC and WHO websites for updates and advice. The CDC recommends that you wear a mask on planes, buses, trains and other indoor public transportation traveling to, within or out of the U.S., as well as in places such as airports and train stations. Use appropriate hand hygiene when in public. You may also want to talk with your health care provider if you have health conditions that make you more susceptible to respiratory infections and complications.
Diagnosis
If you develop symptoms of coronavirus disease 2019 (COVID-19) or you've been exposed to the COVID-19 virus, contact your health care provider. Also let your health care provider know if you've had close contact with anyone who has been diagnosed with COVID-19.
Factors used to decide whether to test you for the virus that causes COVID-19 may differ depending on where you live. Depending on your location, you may need to be screened by your clinic to determine if testing is appropriate and available.
In the U.S., your health care provider will determine whether to conduct tests for the virus that causes COVID-19 based on your signs and symptoms, as well as whether you have had close contact with someone diagnosed with COVID-19. Your health care provider may also consider testing if you are at higher risk of serious illness or you are going to have a medical procedure. If you have had close contact with someone with COVID-19 but you've had COVID-19 in the past three months, you don't need to be tested. If you've been fully vaccinated and you've had close contact with someone with COVID-19, get tested 5 to 7 days after you've had contact with them.
To test for the COVID-19 virus, a health care provider takes a sample from the nose (nasopharyngeal swab), throat (throat swab) or saliva. The samples are then sent to a lab for testing. If you're coughing up sputum, that may be sent for testing. The FDA has authorized at-home tests for the COVID-19 virus. These are available only with a doctor's prescription.
Treatment
Currently, only one medication has been approved to treat COVID-19. No cure is available for COVID-19. Antibiotics aren't effective against viral infections such as COVID-19. Researchers are testing a variety of possible treatments.
The FDA has approved the antiviral drug remdesivir (Veklury) to treat COVID-19 in hospitalized adults and children who are age 12 and older in the hospital. Remdesivir may be prescribed for people who are hospitalized with COVID-19 and need supplemental oxygen or have a higher risk of serious illness. It's given through a needle in the skin (intravenously).
The FDA has authorized a drug called Paxlovid that includes nirmatrelvir – a drug that blocks the activity of a specific enzyme needed for the virus that causes COVID-19 to replicate – and an antiviral drug called ritonavir that helps slow the breakdown of nirmatrelvir. Paxlovid is authorized to treat mild to moderate COVID-19 in people age 12 and older who are at higher risk of serious illness. The medications are taken by mouth as pills.
The FDA has authorized another drug called molnupiravir to treat mild to moderate COVID-19 in adults who are at higher risk of serious illness and who aren't able to take other treatment options. The medication is taken by mouth as a pill.
The FDA has authorized the rheumatoid arthritis drug baricitinib (Olumiant) to treat COVID-19 in some cases. Baricitinib is a pill that seems to work against COVID-19 by reducing inflammation and having antiviral activity. Baricitinib may be used in people who are hospitalized with COVID-19 who are on mechanical ventilators or need supplemental oxygen.
Monoclonal antibody medications include sotrovimab; bebtelovimab; a combination of bamlanivimab and etesevimab; and a combination of casirivimab and imdevimab. Some monoclonal antibodies, including bamlanivimab and etesevimab and casirivimab and imdevimab, aren't effective against COVID-19 caused by the omicron variant. However, sotrovimab and bebtelovimab can be used to treat COVID-19 caused by the omicron variant.
These drugs are used to treat mild to moderate COVID-19 in people who have a higher risk of developing serious illness due to COVID-19. Treatment involves a single infusion given by a needle in the arm (intravenously) in an outpatient setting. To be most effective, these medications need to be given soon after COVID-19 symptoms start and prior to hospitalization.
The U.S. National Institutes of Health has recommended the corticosteroid dexamethasone for people hospitalized with severe COVID-19 who are on supplemental oxygen or need mechanical ventilation. Other corticosteroids, such as prednisone, methylprednisolone or hydrocortisone, may be used if dexamethasone isn't available.
In some cases, the drugs remdesivir, tocilizumab or baricitinib may be given with dexamethasone in hospitalized people who are on mechanical ventilation or need supplemental oxygen.
The FDA has also authorized convalescent plasma therapy with high antibody levels to treat COVID-19. Convalescent plasma is blood donated by people who've recovered from COVID-19. Convalescent plasma with high antibodies may be used to treat some hospitalized people ill with COVID-19 who are either early in their illness or who have weakened immune systems.
Many people with COVID-19 may have mild illness and can be treated with supportive care. Supportive care is aimed at relieving symptoms and may include:
- Pain relievers (ibuprofen or acetaminophen)
- Cough syrup or medication
- Rest
- Fluid intake
There is no evidence that ibuprofen or other nonsteroidal anti-inflammatory drugs (NSAIDs) need to be avoided.
If you have mild symptoms, your health care provider will likely recommend that you recover at home. You may be given special instructions to monitor your symptoms and to avoid spreading the illness to others. You'll likely be asked to isolate yourself as much as possible from family and pets while you're sick, wear a mask when you're around people and pets, and use a separate bedroom and bathroom. And keep air flow in your home by opening windows and using air filters when possible.
Your health care provider will likely recommend that you stay in home isolation for a period of time except to get medical care. Your health care provider will likely follow up with you regularly. Follow guidelines from your health care provider and local health department about when you can end home isolation.
If you're very ill, you may need to be treated in the hospital.
Coping and support
It's common to feel fearful and anxious during the COVID-19 pandemic. You're probably worried that you or those you love will get sick. You may be concerned about taking care of yourself or others who are ill.
During this time, remember to take care of yourself and manage your stress.
- Eat healthy meals.
- Get enough sleep.
- Get physical activity.
- Try relaxation exercises such as deep breathing, stretching and meditation.
- Avoid watching or reading too much news.
- Connect with friends and family, such as with phone or video calls.
- Do activities you enjoy, such as reading a book or watching a funny movie.
If you're ill with COVID-19, it's especially important to:
- Get plenty of rest.
- Drink fluids.
- Let your health care provider know right away if your symptoms worsen.
Having COVID-19 or caring for someone with the disease can cause stress and anxiety. If stress is affecting your daily life after several days, contact your health care provider and consider requesting a referral to a mental health professional.
Preparing for an appointment
To be treated for COVID-19, you may start by seeing your primary care doctor or other health care provider. Or you may be referred immediately to a doctor trained in treating infectious diseases. If you think you have COVID-19, tell your health care provider before going in. The health care provider and medical team can then:
- Contact infection prevention and control and public health officials
- Prepare to move you to a room quickly
- Have a mask ready for you
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment
- Your recent travels, including any international travels
- Key personal information, including major stresses, recent life changes and family medical history
- All medications, vitamins or other supplements you take, including the doses
- Questions to ask your doctor
Take a family member or friend along, if possible, to help you remember the information you're given. Avoid bringing more than one or two people. Check before you go to the appointment, as your hospital or clinic may have visitor restrictions.
Some basic questions to ask your health care provider include:
- How likely is it that COVID-19 is causing my symptoms?
- What are other possible causes for my symptoms?
- What tests do I need?
- What course of action do you recommend?
- Are there restrictions I need to follow?
- Should I see a specialist?
What to expect from your doctor
Your health care provider is likely to ask you several questions, such as:
- When did your symptoms begin?
- Where have you traveled recently?
- Who have you been in close contact with?
- How severe are your symptoms?
Copyright © 1998-2026 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.