Esophageal varices are abnormal, enlarged veins in the tube that connects the throat and stomach (esophagus). This condition occurs most often in people with serious liver diseases.
Esophageal varices develop when normal blood flow to the liver is blocked by a clot or scar tissue in the liver. To go around the blockages, blood flows into smaller blood vessels that aren't designed to carry large volumes of blood. The vessels can leak blood or even rupture, causing life-threatening bleeding.
A number of drugs and medical procedures can help prevent or stop bleeding from esophageal varices.
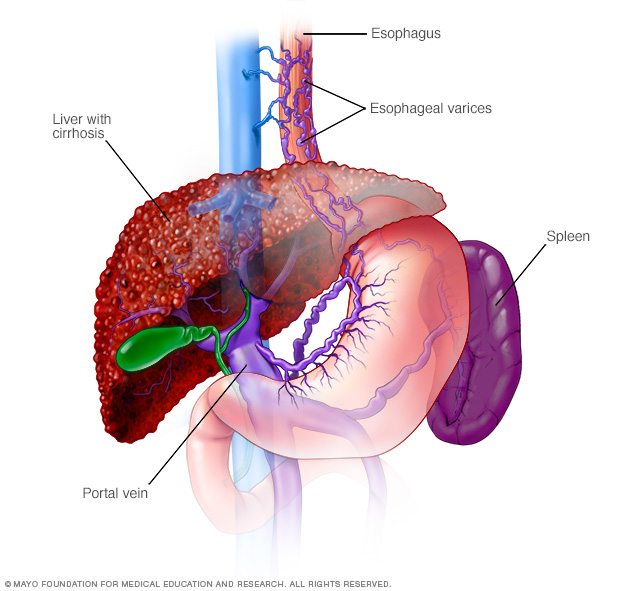
Esophageal varices are enlarged veins in the esophagus. They're often due to obstructed blood flow through the portal vein, which carries blood from the intestine, pancreas and spleen to the liver.
Symptoms
Esophageal varices usually don't cause signs and symptoms unless they bleed. Signs and symptoms of bleeding esophageal varices include:
- Vomiting large amounts of blood
- Black, tarry or bloody stools
- Lightheadedness
- Loss of consciousness in severe cases
Your doctor might suspect esophageal varices if you have signs of liver disease, including:
- Yellow coloration of your skin and eyes (jaundice)
- Easy bleeding or bruising
- Fluid buildup in your abdomen (ascites)
When to see a doctor
Make an appointment with your doctor if you have signs or symptoms that worry you. If you've been diagnosed with liver disease, ask your doctor about your risk of esophageal varices and what you can do to reduce your risk. Also ask your doctor whether you should get a procedure to check for esophageal varices.
If you've been diagnosed with esophageal varices, your doctor is likely to instruct you to watch for signs of bleeding. Bleeding esophageal varices are an emergency. Call 911 or your local emergency services right away if you have bloody vomit or bloody stools.
Causes
Esophageal varices sometimes form when blood flow to your liver is blocked, most often by scar tissue in the liver caused by liver disease. The blood flow begins to back up, increasing pressure within the large vein (portal vein) that carries blood to your liver.
This increased pressure (portal hypertension) forces the blood to seek other pathways through smaller veins, such as those in the lowest part of the esophagus. These thin-walled veins balloon with the added blood. Sometimes the veins rupture and bleed.
Causes of esophageal varices include:
- Severe liver scarring (cirrhosis). A number of liver diseases — including hepatitis infection, alcoholic liver disease, fatty liver disease and a bile duct disorder called primary biliary cirrhosis — can result in cirrhosis.
- Blood clot (thrombosis). A blood clot in the portal vein or in a vein that feeds into the portal vein (splenic vein) can cause esophageal varices.
- Parasitic infection. Schistosomiasis is a parasitic infection found in parts of Africa, South America, the Caribbean, the Middle East and East Asia. The parasite can damage the liver, as well as the lungs, intestine, bladder and other organs.
Risk factors
Although many people with advanced liver disease develop esophageal varices, most won't have bleeding. Esophageal varices are more likely to bleed if you have:
- High portal vein pressure. The risk of bleeding increases as the pressure in the portal vein increases (portal hypertension).
- Large varices. The larger the esophageal varices, the more likely they are to bleed.
- Red marks on the varices. When viewed through a thin, flexible tube (endoscope) passed down your throat, some esophageal varices show long, red streaks or red spots. These marks indicate a high risk of bleeding.
- Severe cirrhosis or liver failure. Most often, the more severe your liver disease, the more likely esophageal varices are to bleed.
- Continued alcohol use. Your risk of variceal bleeding is far greater if you continue to drink than if you stop, especially if your disease is alcohol related.
If you've had bleeding from esophageal varices before, you're more likely to have varices that bleed again.
Complications
The most serious complication of esophageal varices is bleeding. Once you've had a bleeding episode, your risk of another bleeding episode greatly increases. If you lose enough blood, you can go into shock, which can lead to death.
Prevention
Currently, no treatment can prevent the development of esophageal varices in people with cirrhosis. While beta blocker drugs are effective in preventing bleeding in many people who have esophageal varices, they don't prevent esophageal varices from forming.
If you've been diagnosed with liver disease, ask your doctor about strategies to avoid liver disease complications. To keep your liver healthy:
- Don't drink alcohol. People with liver disease are often advised to stop drinking alcohol, since the liver processes alcohol. Drinking alcohol may stress an already vulnerable liver.
- Eat a healthy diet. Choose a plant-based diet that's full of fruits and vegetables. Select whole grains and lean sources of protein. Reduce the amount of fatty and fried foods you eat.
- Maintain a healthy weight. An excess amount of body fat can damage your liver. Obesity is associated with a greater risk of complications of cirrhosis. Lose weight if you are obese or overweight.
- Use chemicals sparingly and carefully. Follow the directions on household chemicals, such as cleaning supplies and insect sprays. If you work around chemicals, follow all safety precautions. Your liver removes toxins from your body, so give it a break by limiting the amount of toxins it must process.
- Reduce your risk of hepatitis. Sharing needles and having unprotected sex can increase your risk of hepatitis B and C. Protect yourself by abstaining from sex or using a condom if you choose to have sex. Get tested for exposure to hepatitis A, B and C, since infection can make your liver disease worse. Also ask your doctor whether you should be vaccinated for hepatitis A and hepatitis B.
Diagnosis
If you have cirrhosis, your doctor should screen you for esophageal varices when you're diagnosed. How often you'll undergo screening tests depends on your condition. Main tests used to diagnose esophageal varices are:
-
Endoscopic exam. A procedure called upper gastrointestinal endoscopy is the preferred method of screening for esophageal varices. Your doctor inserts a thin, flexible, lighted tube (endoscope) through your mouth and into your esophagus, stomach and the beginning of your small intestine (duodenum).
The doctor will look for dilated veins, measure them, if found, and check for red streaks and red spots, which usually indicate a significant risk of bleeding. Treatment can be performed during the exam.
- Imaging tests. Both abdominal CT scans and Doppler ultrasounds of the splenic and portal veins can suggest the presence of esophageal varices. An ultrasound test called transient elastography that measures scarring in the liver can help your doctor determine if you have portal hypertension, which may lead to esophageal varices.
- Capsule endoscopy. In this test, you swallow a vitamin-sized capsule containing a tiny camera, which takes pictures of the esophagus as it goes through your digestive tract. This might be an option for people who are unable or unwilling to have an endoscopic exam. This technology is more expensive than regular endoscopy and not as available. Capsule endoscopy can only help find esophageal varices and does not treat them.
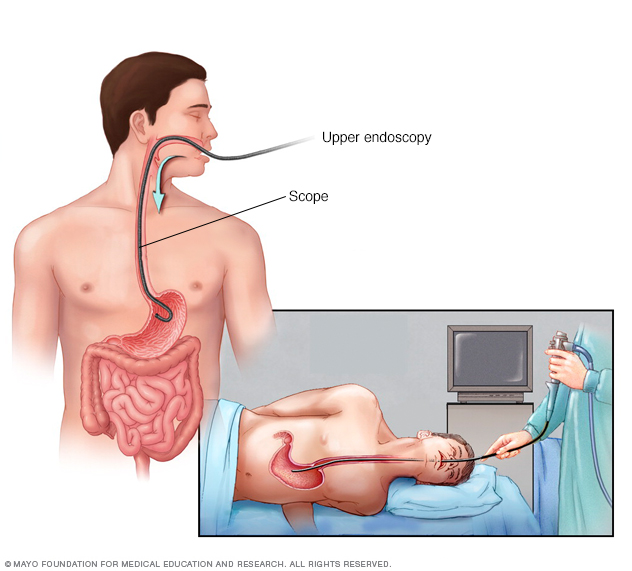
During an endoscopy, your doctor inserts a thin, flexible tube equipped with a light and camera (endoscope) down your throat and into your esophagus. The tiny camera lets your doctor examine your esophagus, stomach and the beginning of your small intestine (duodenum).
Treatment
The primary aim in treating esophageal varices is to prevent bleeding. Bleeding esophageal varices are life-threatening. If bleeding occurs, treatments are available to try to stop the bleeding.
Treatment to prevent bleeding
Treatments to lower blood pressure in the portal vein may reduce the risk of bleeding esophageal varices. Treatments may include:
- Medications to reduce pressure in the portal vein. A type of blood pressure drug called a beta blocker may help reduce blood pressure in your portal vein, decreasing the likelihood of bleeding. These medications include propranolol (Inderal, Innopran XL) and nadolol (Corgard).
-
Using elastic bands to tie off bleeding veins. If your esophageal varices appear to have a high risk of bleeding, or if you've had bleeding from varices before, your doctor might recommend a procedure called endoscopic band ligation.
Using an endoscope, the doctor uses suction to pull the varices into a chamber at the end of the scope and wraps them with an elastic band, which essentially "strangles" the veins so they can't bleed. Endoscopic band ligation carries a small risk of complications, such as bleeding and scarring of the esophagus.
Treatment if you're bleeding
Bleeding esophageal varices are life-threatening, and immediate treatment is essential. Treatments used to stop bleeding and reverse the effects of blood loss include:
- Using elastic bands to tie off bleeding veins. Your doctor may wrap elastic bands around the esophageal varices during an endoscopy.
- Medications to slow blood flow into the portal vein. Drugs such as octreotide (Sandostatin) and vasopressin (Vasostrict) slow the flow of blood to the portal vein. The drug is usually continued for up to five days after a bleeding episode.
-
Diverting blood flow away from the portal vein. If medication and endoscopy treatments don't stop the bleeding, your doctor might recommend a procedure called transjugular intrahepatic portosystemic shunt (TIPS).
The shunt is an opening that is created between the portal vein and the hepatic vein, which carries blood from your liver to your heart. The shunt reduces pressure in the portal vein and often stops bleeding from esophageal varices.
But TIPS can cause serious complications, including liver failure and mental confusion, which can develop when toxins that the liver normally would filter are passed through the shunt directly into the bloodstream.
TIPS is mainly used when all other treatments have failed or as a temporary measure in people awaiting a liver transplant.
-
Placing pressure on varices to stop bleeding. If medication and endoscopy treatments don't work, doctors may try to stop bleeding by applying pressure to the esophageal varices. One way to temporarily stop bleeding is by inflating a balloon to put pressure on the varices for up to 24 hours, a procedure called balloon tamponade. Balloon tamponade is a temporary measure before other treatments can be performed, such as TIPS.
This procedure carries a high risk of bleeding recurrence after the balloon is deflated. Balloon tamponade may also cause serious complications, including a rupture in the esophagus, which can lead to death.
- Restoring blood volume. You might be given a transfusion to replace lost blood and a clotting factor to stop bleeding.
- Preventing infection. There is an increased risk of infection with bleeding, so you'll likely be given an antibiotic to prevent infection.
- Replacing the diseased liver with a healthy one. Liver transplant is an option for people with severe liver disease or those who experience recurrent bleeding of esophageal varices. Although liver transplantation is often successful, the number of people awaiting transplants far outnumbers the available organs.
Re-bleeding
There is a high risk that bleeding will recur in people who've had bleeding from esophageal varices. Beta blockers and endoscopic band ligation are the recommended treatments to help prevent re-bleeding.
After initial banding treatment, your doctor will repeat your upper endoscopy at regular intervals and apply more bands if necessary until the esophageal varices are gone or small enough to reduce the risk of further bleeding.
Potential future treatment
Doctors are exploring an experimental emergency therapy to stop bleeding from esophageal varices that involves spraying an adhesive powder. The hemostatic powder is administered through a catheter during an endoscopy. When sprayed on the esophagus, hemostatic powder sticks to the varices and may stop bleeding.
Another potential way to stop bleeding when all other measures fail is to use self-expanding metal stents (SEMS). SEMS can be placed during an endoscopy and stop bleeding by placing pressure on the bleeding esophageal varices.
However, SEMS could damage tissue and can migrate after being placed. The stent should be removed within seven days and bleeding could recur. This option is experimental and isn't yet widely available.
Preparing for an appointment
You might start by seeing your primary care provider. Or you may be referred immediately to a doctor who specializes in digestive disorders (gastroenterologist). If you're having signs and symptoms of internal bleeding, call 911 or your local emergency number to be taken to the hospital for urgent care.
Here's some information to help you get ready for an appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before a specific test. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment
- Key personal information, including major stresses, recent life changes or recent travels, family and personal medical history, and your alcohol use
- All medications, vitamins or other supplements you take, including doses
- Questions to ask your doctor
Take a family member or friend along, if possible, to help you remember information you're given.
For esophageal varices, questions to ask your doctor include:
- What's likely causing my symptoms?
- What other possible causes are there?
- What tests do I need?
- What's the best course of action?
- What are the side effects of the treatments?
- Are my symptoms likely to recur, and what can I do to prevent that?
- I have other health conditions. How can I best manage them together?
- Are there restrictions that I need to follow?
- Should I see a specialist?
- Are there brochures or other printed materials I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you questions, such as:
- When did your symptoms begin?
- Have your symptoms stayed the same or gotten worse?
- How severe are your symptoms?
- Have you had signs of bleeding, such as blood in your stools or vomit?
- Have you had hepatitis or yellowing of your eyes or skin (jaundice)?
- Have you traveled recently? Where?
- If you drink alcohol, when did you start and how much do you drink?
What you can do in the meantime
If you develop bloody vomit or stools while you're waiting for your appointment, call 911 or your local emergency number or go to an emergency room immediately.
Copyright © 1998-2026 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.