Hemorrhoids (HEM-uh-roids), also called piles, are swollen veins in your anus and lower rectum, similar to varicose veins. Hemorrhoids can develop inside the rectum (internal hemorrhoids) or under the skin around the anus (external hemorrhoids).
Nearly three out of four adults will have hemorrhoids from time to time. Hemorrhoids have a number of causes, but often the cause is unknown.
Fortunately, effective options are available to treat hemorrhoids. Many people get relief with home treatments and lifestyle changes.
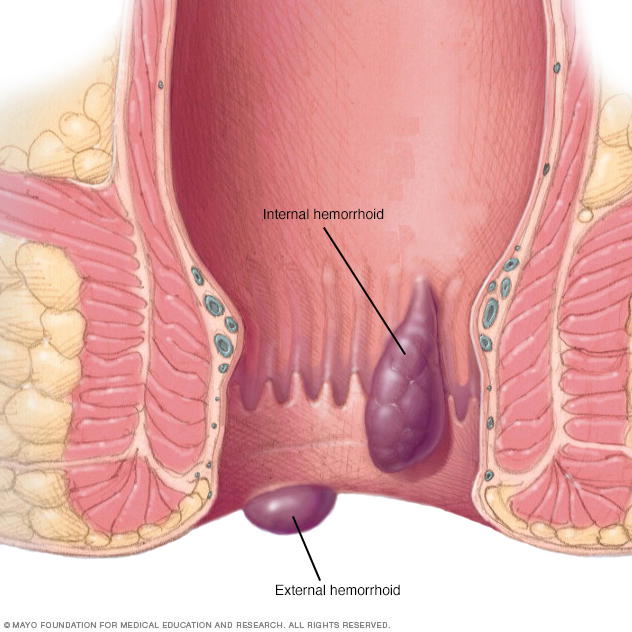
Hemorrhoids are swollen veins in your lower rectum. Internal hemorrhoids are usually painless, but tend to bleed. External hemorrhoids may cause pain.
Symptoms
Signs and symptoms of hemorrhoids usually depend on the type of hemorrhoid.
External hemorrhoids
These are under the skin around your anus. Signs and symptoms might include:
- Itching or irritation in your anal region
- Pain or discomfort
- Swelling around your anus
- Bleeding
Internal hemorrhoids
Internal hemorrhoids lie inside the rectum. You usually can't see or feel them, and they rarely cause discomfort. But straining or irritation when passing stool can cause:
- Painless bleeding during bowel movements. You might notice small amounts of bright red blood on your toilet tissue or in the toilet.
- A hemorrhoid to push through the anal opening (prolapsed or protruding hemorrhoid), resulting in pain and irritation.
Thrombosed hemorrhoids
If blood pools in an external hemorrhoid and forms a clot (thrombus), it can result in:
- Severe pain
- Swelling
- Inflammation
- A hard lump near your anus
When to see a doctor
If you have bleeding during bowel movements or you have hemorrhoids that don't improve after a week of home care, talk to your doctor.
Don't assume rectal bleeding is due to hemorrhoids, especially if you have changes in bowel habits or if your stools change in color or consistency. Rectal bleeding can occur with other diseases, including colorectal cancer and anal cancer.
Seek emergency care if you have large amounts of rectal bleeding, lightheadedness, dizziness or faintness.
Causes
The veins around your anus tend to stretch under pressure and may bulge or swell. Hemorrhoids can develop from increased pressure in the lower rectum due to:
- Straining during bowel movements
- Sitting for long periods of time on the toilet
- Having chronic diarrhea or constipation
- Being obese
- Being pregnant
- Having anal intercourse
- Eating a low-fiber diet
- Regular heavy lifting
Risk factors
As you age, your risk of hemorrhoids increases. That's because the tissues that support the veins in your rectum and anus can weaken and stretch. This can also happen when you're pregnant, because the baby's weight puts pressure on the anal region.
Complications
Complications of hemorrhoids are rare but include:
- Anemia. Rarely, chronic blood loss from hemorrhoids may cause anemia, in which you don't have enough healthy red blood cells to carry oxygen to your cells.
- Strangulated hemorrhoid. If the blood supply to an internal hemorrhoid is cut off, the hemorrhoid may be "strangulated," which can cause extreme pain.
- Blood clot. Occasionally, a clot can form in a hemorrhoid (thrombosed hemorrhoid). Although not dangerous, it can be extremely painful and sometimes needs to be lanced and drained.
Prevention
The best way to prevent hemorrhoids is to keep your stools soft, so they pass easily. To prevent hemorrhoids and reduce symptoms of hemorrhoids, follow these tips:
- Eat high-fiber foods. Eat more fruits, vegetables and whole grains. Doing so softens the stool and increases its bulk, which will help you avoid the straining that can cause hemorrhoids. Add fiber to your diet slowly to avoid problems with gas.
- Drink plenty of fluids. Drink six to eight glasses of water and other liquids (not alcohol) each day to help keep stools soft.
-
Consider fiber supplements. Most people don't get enough of the recommended amount of fiber — 20 to 30 grams a day — in their diet. Studies have shown that over-the-counter fiber supplements, such as psyllium (Metamucil) or methylcellulose (Citrucel), improve overall symptoms and bleeding from hemorrhoids.
If you use fiber supplements, be sure to drink at least eight glasses of water or other fluids every day. Otherwise, the supplements can cause or worsen constipation.
- Don't strain. Straining and holding your breath when trying to pass a stool creates greater pressure in the veins in the lower rectum.
- Go as soon as you feel the urge. If you wait to pass a bowel movement and the urge goes away, your stool could dry out and be harder to pass.
- Exercise. Stay active to help prevent constipation and to reduce pressure on veins, which can occur with long periods of standing or sitting. Exercise can also help you lose excess weight that might be contributing to your hemorrhoids.
- Avoid long periods of sitting. Sitting too long, particularly on the toilet, can increase the pressure on the veins in the anus.
Diagnosis
Your doctor might be able to see external hemorrhoids. Diagnosing internal hemorrhoids might include examination of your anal canal and rectum.
- Digital examination. Your doctor inserts a gloved, lubricated finger into your rectum. He or she feels for anything unusual, such as growths.
- Visual inspection. Because internal hemorrhoids are often too soft to be felt during a rectal exam, your doctor might examine the lower portion of your colon and rectum with an anoscope, proctoscope or sigmoidoscope.
Your doctor might want to examine your entire colon using colonoscopy if:
- Your signs and symptoms suggest you might have another digestive system disease
- You have risk factors for colorectal cancer
- You are middle-aged and haven't had a recent colonoscopy
Treatment
Home remedies
You can often relieve the mild pain, swelling and inflammation of hemorrhoids with home treatments.
- Eat high-fiber foods. Eat more fruits, vegetables and whole grains. Doing so softens the stool and increases its bulk, which will help you avoid the straining that can worsen symptoms from existing hemorrhoids. Add fiber to your diet slowly to avoid problems with gas.
- Use topical treatments. Apply an over-the-counter hemorrhoid cream or suppository containing hydrocortisone, or use pads containing witch hazel or a numbing agent.
- Soak regularly in a warm bath or sitz bath. Soak your anal area in plain warm water for 10 to 15 minutes two to three times a day. A sitz bath fits over the toilet.
- Take oral pain relievers. You can use acetaminophen (Tylenol, others), aspirin or ibuprofen (Advil, Motrin IB, others) temporarily to help relieve your discomfort.
With these treatments, hemorrhoid symptoms often go away within a week. See your doctor in a week if you don't get relief, or sooner if you have severe pain or bleeding.
Medications
If your hemorrhoids produce only mild discomfort, your doctor might suggest over-the-counter creams, ointments, suppositories or pads. These products contain ingredients such as witch hazel, or hydrocortisone and lidocaine, which can temporarily relieve pain and itching.
Don't use an over-the-counter steroid cream for more than a week unless directed by your doctor because it can thin your skin.
External hemorrhoid thrombectomy
If a painful blood clot (thrombosis) has formed within an external hemorrhoid, your doctor can remove the hemorrhoid, which can provide prompt relief. This procedure, done under local anesthesia, is most effective if done within 72 hours of developing a clot.
Minimally invasive procedures
For persistent bleeding or painful hemorrhoids, your doctor might recommend one of the other minimally invasive procedures available. These treatments can be done in your doctor's office or other outpatient setting and don't usually require anesthesia.
-
Rubber band ligation. Your doctor places one or two tiny rubber bands around the base of an internal hemorrhoid to cut off its circulation. The hemorrhoid withers and falls off within a week.
Hemorrhoid banding can be uncomfortable and cause bleeding, which might begin two to four days after the procedure but is rarely severe. Occasionally, more-serious complications can occur.
- Injection (sclerotherapy). Your doctor injects a chemical solution into the hemorrhoid tissue to shrink it. While the injection causes little or no pain, it might be less effective than rubber band ligation.
- Coagulation (infrared, laser or bipolar). Coagulation techniques use laser or infrared light or heat. They cause small, bleeding internal hemorrhoids to harden and shrivel. Coagulation has few side effects and usually causes little discomfort.
Surgical procedures
Only a small percentage of people with hemorrhoids require surgery. However, if other procedures haven't been successful or you have large hemorrhoids, your doctor might recommend one of the following:
-
Hemorrhoid removal (hemorrhoidectomy). Choosing one of various techniques, your surgeon removes excessive tissue that causes bleeding. The surgery can be done with local anesthesia combined with sedation, spinal anesthesia or general anesthesia.
Hemorrhoidectomy is the most effective and complete way to treat severe or recurring hemorrhoids. Complications can include temporary difficulty emptying your bladder, which can result in urinary tract infections. This complication occurs mainly after spinal anesthesia.
Most people have some pain after the procedure, which medications can relieve. Soaking in a warm bath also might help.
-
Hemorrhoid stapling. This procedure, called stapled hemorrhoidopexy, blocks blood flow to hemorrhoidal tissue. It is typically used only for internal hemorrhoids.
Stapling generally involves less pain than hemorrhoidectomy and allows for earlier return to regular activities. Compared with hemorrhoidectomy, however, stapling has been associated with a greater risk of recurrence and rectal prolapse, in which part of the rectum protrudes from the anus.
Complications can also include bleeding, urinary retention and pain, as well as, rarely, a life-threatening blood infection (sepsis). Talk with your doctor about the best option for you.
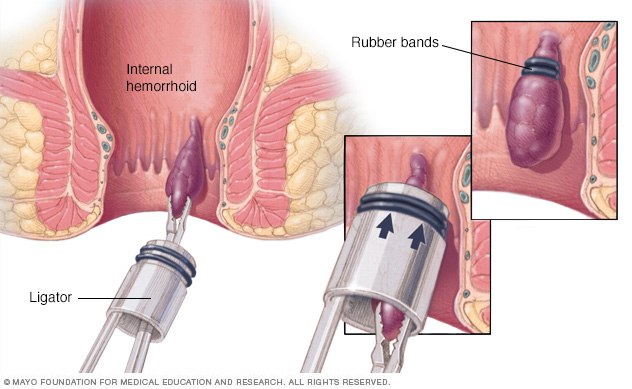
To remove a hemorrhoid using rubber band ligation, your doctor inserts a small tool called a ligator through a lighted tube (scope) in the anal canal and grasps the hemorrhoid with forceps. Sliding the ligator's cylinder upward releases rubber bands around the base of the hemorrhoid. Rubber bands cut off the hemorrhoid's blood supply, causing it to wither and drop off.
Preparing for an appointment
If you have signs and symptoms of hemorrhoids, make an appointment with your regular doctor. If needed, your doctor might refer you to one or more specialists — including a doctor with expertise in the digestive system (gastroenterologist) or a colon and rectal surgeon — for evaluation and treatment.
Here are some suggestions to help you get ready for your appointment.
What you can do
Be aware of any pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance.
Make a list of:
- Your symptoms and how long you've noticed them
- Key personal information, including typical bowel habits and diet, especially your fiber intake
- All medications, vitamins or supplements you take, including doses
- Questions to ask your doctor
For hemorrhoids, some questions to ask your doctor include:
- What's the likely cause of my symptoms?
- Is my condition likely to be temporary or permanent?
- Am I at risk of complications related to this condition?
- What treatment approach do you recommend?
- If treatments we try first don't work, what will you recommend next?
- Am I a candidate for surgery? Why or why not?
- Are there additional self-care steps that might help?
- I have other medical problems. How can I manage these along with hemorrhoids?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you questions, including:
- How uncomfortable are your symptoms?
- What are your typical bowel habits?
- How much fiber does your diet contain?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Has anyone in your family had hemorrhoids or cancer of the colon, rectum or anus?
- Have you had a change in your bowel habits?
- During bowel movements, have you noticed blood on your toilet paper, dripping into the toilet or mixed into your stools?
What you can do in the meantime
Before your appointment, take steps to soften your stools. Eat more high-fiber foods, such as fruits, vegetables and whole grains, and consider an over-the-counter fiber supplement, such as Metamucil or Citrucel. Drinking six to eight glasses of water a day also might help relieve your symptoms.
Copyright © 1998-2026 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.