Hypercalcemia is a condition in which the calcium level in your blood is above normal. Too much calcium in your blood can weaken your bones, create kidney stones, and interfere with how your heart and brain work.
Hypercalcemia is usually a result of overactive parathyroid glands. These four tiny glands are situated in the neck, near the thyroid gland. Other causes of hypercalcemia include cancer, certain other medical disorders, some medications, and taking too much of calcium and vitamin D supplements.
Signs and symptoms of hypercalcemia range from nonexistent to severe. Treatment depends on the cause.
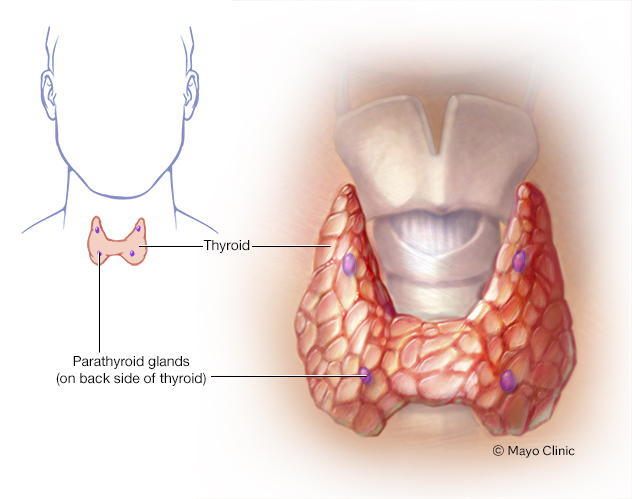
The parathyroid glands lie behind the thyroid. They produce parathyroid hormone, which plays a role in regulating the body's blood level of calcium and phosphorus.
Symptoms
You might not have signs or symptoms if your hypercalcemia is mild. More-severe cases produce signs and symptoms related to the parts of your body affected by the high calcium levels in your blood. Examples include:
- Kidneys. Excess calcium makes your kidneys work harder to filter it. This can cause excessive thirst and frequent urination.
- Digestive system. Hypercalcemia can cause stomach upset, nausea, vomiting and constipation.
- Bones and muscles. In most cases, the excess calcium in your blood was leached from your bones, which weakens them. This can cause bone pain and muscle weakness.
- Brain. Hypercalcemia can interfere with how your brain works, resulting in confusion, lethargy and fatigue. It can also cause depression.
- Heart. Rarely, severe hypercalcemia can interfere with your heart function, causing palpitations and fainting, indications of cardiac arrhythmia, and other heart problems.
When to see a doctor
Contact your doctor if you develop signs and symptoms that might indicate hypercalcemia, such as being extremely thirsty, urinating frequently and having abdominal pain.
Causes
Besides building strong bones and teeth, calcium helps muscles contract and nerves transmit signals. Normally, if there isn't enough calcium in your blood, your parathyroid glands secrete a hormone that triggers:
- Your bones to release calcium into your blood
- Your digestive tract to absorb more calcium
- Your kidneys to excrete less calcium and activate more vitamin D, which plays a vital role in calcium absorption
This delicate balance between too little calcium in your blood and hypercalcemia can be disrupted by a variety of factors. Hypercalcemia is caused by:
- Overactive parathyroid glands (hyperparathyroidism). This most common cause of hypercalcemia can stem from a small, noncancerous (benign) tumor or enlargement of one or more of the four parathyroid glands.
- Cancer. Lung cancer and breast cancer, as well as some blood cancers, can increase your risk of hypercalcemia. Spread of cancer (metastasis) to your bones also increases your risk.
- Other diseases. Certain diseases, such as tuberculosis and sarcoidosis, can raise blood levels of vitamin D, which stimulates your digestive tract to absorb more calcium.
- Hereditary factors. A rare genetic disorder known as familial hypocalciuric hypercalcemia causes an increase of calcium in your blood because of faulty calcium receptors in your body. This condition doesn't cause symptoms or complications of hypercalcemia.
- Immobility. People who have a condition that causes them to spend a lot of time sitting or lying down can develop hypercalcemia. Over time, bones that don't bear weight release calcium into the blood.
- Severe dehydration. A common cause of mild or transient hypercalcemia is dehydration. Having less fluid in your blood causes a rise in calcium concentrations.
- Medications. Certain drugs — such as lithium, used to treat bipolar disorder — might increase the release of parathyroid hormone.
- Supplements. Taking excessive amounts of calcium or vitamin D supplements over time can raise calcium levels in your blood above normal.
Complications
Hypercalcemia complications can include:
- Osteoporosis. If your bones continue to release calcium into your blood, you can develop the bone-thinning disease osteoporosis, which could lead to bone fractures, spinal column curvature and loss of height.
- Kidney stones. If your urine contains too much calcium, crystals might form in your kidneys. Over time, the crystals can combine to form kidney stones. Passing a stone can be extremely painful.
- Kidney failure. Severe hypercalcemia can damage your kidneys, limiting their ability to cleanse the blood and eliminate fluid.
- Nervous system problems. Severe hypercalcemia can lead to confusion, dementia and coma, which can be fatal.
- Abnormal heart rhythm (arrhythmia). Hypercalcemia can affect the electrical impulses that regulate your heartbeat, causing your heart to beat irregularly.
Diagnosis
Because hypercalcemia can cause few, if any, signs or symptoms, you might not know you have the disorder until routine blood tests reveal a high level of blood calcium. Blood tests can also show whether your parathyroid hormone level is high, indicating that you have hyperparathyroidism.
To determine if your hypercalcemia is caused by a disease such as cancer or sarcoidosis, your doctor might recommend imaging tests of your bones or lungs.
Treatment
If your hypercalcemia is mild, you and your doctor might choose to watch and wait, monitoring your bones and kidneys over time to be sure they remain healthy.
For more severe hypercalcemia, your doctor might recommend medications or treatment of the underlying disease, including surgery.
Medications
In some cases, your doctor might recommend:
- Calcitonin (Miacalcin). This hormone from salmon controls calcium levels in the blood. Mild nausea might be a side effect.
- Calcimimetics. This type of drug can help control overactive parathyroid glands. Cinacalcet (Sensipar) has been approved for managing hypercalcemia.
- Bisphosphonates. Intravenous osteoporosis drugs, which can quickly lower calcium levels, are often used to treat hypercalcemia due to cancer. Risks associated with this treatment include breakdown (osteonecrosis) of the jaw and certain types of thigh fractures.
- Denosumab (Prolia, Xgeva). This drug is often used to treat people with cancer-caused hypercalcemia who don't respond well to bisphosphonates.
- Prednisone. If your hypercalcemia is caused by high levels of vitamin D, short-term use of steroid pills such as prednisone are usually helpful.
- IV fluids and diuretics. Extremely high calcium levels can be a medical emergency. You might need hospitalization for treatment with IV fluids and diuretics to promptly lower the calcium level to prevent heart rhythm problems or damage to the nervous system.
Surgical and other procedures
Problems associated with overactive parathyroid glands often can be cured by surgery to remove the tissue that's causing the problem. In many cases, only one of a person's four parathyroid glands is affected. A special scanning test uses an injection of a small dose of radioactive material to pinpoint the gland or glands that aren't working properly.
Preparing for an appointment
You might start by seeing your primary care provider. However, you'll likely be referred to a doctor who specializes in treating hormonal disorders (endocrinologist).
Here's some information to help you get ready for your appointment.
What you can do
Before your appointment, make a list of:
- Your symptoms, including those that seem unrelated, and when they began
- Key personal information, including major stresses or recent life changes, medical history, and family medical history
- All medications, vitamins and other supplements you take, including doses
- Questions to ask your doctor
Take a family member or friend along, if possible, to help you remember the information you're given.
For hypercalcemia, basic questions to ask your doctor include:
- What's the most likely cause of my symptoms?
- What tests do I need?
- What treatments are available, and which do you recommend?
- What side effects can I expect from treatment?
- Are there alternatives to the primary approach that you're suggesting?
- I have other health conditions. How can I best manage them together?
What to expect from your doctor
Your doctor is likely to ask you questions, including:
- Does anything improve your symptoms?
- What, if anything, worsens your symptoms?
- Have you had kidney stones, bone fractures or osteoporosis?
- Do you have bone pain?
- Do you have unexplained weight loss?
- Have family members had hypercalcemia or kidney stones?
Copyright © 1998-2026 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.