Hypopituitarism is a rare disorder in which your pituitary gland fails to produce one or more hormones, or doesn't produce enough hormones.
The pituitary gland is a kidney-bean-sized gland situated at the base of your brain. It is part of your body's endocrine system, which consists of all the glands that produce and regulate hormones. Despite its small size, the pituitary gland creates and releases a number of hormones that act on nearly every part of your body.
Hypopituitarism is when you have a short supply (deficiency) of one or more of the pituitary hormones. These hormone deficiencies can affect any number of your body's routine functions, such as growth, blood pressure or reproduction. Symptoms typically vary, based on which hormone or hormones you are missing.
If you have hypopituitarism, you'll likely need to take medication for the rest of your life. Medication helps replace the missing hormones, which helps control your symptoms.
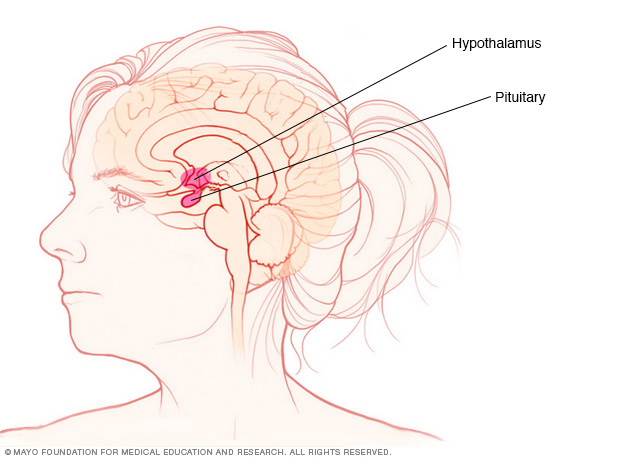
The pituitary gland and the hypothalamus are located within the brain and control hormone production.
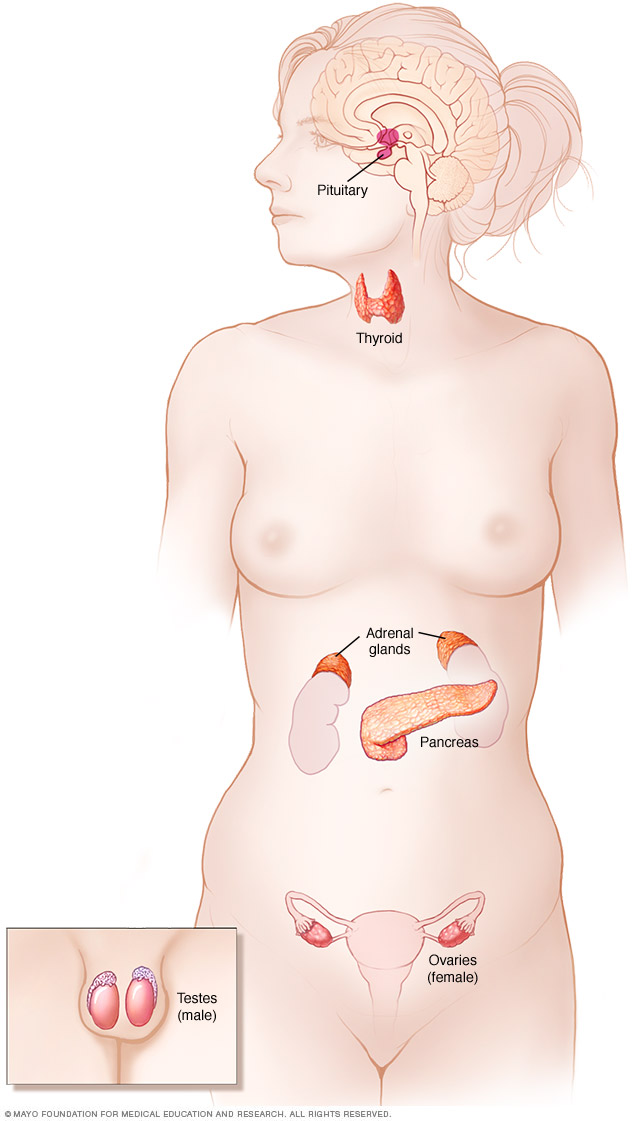
The endocrine system includes the pituitary gland, thyroid gland, parathyroid glands, adrenal glands, pancreas, ovaries and testicles.
Symptoms
The signs and symptoms of hypopituitarism usually develop gradually and get worse over time. They are sometimes subtle and may be overlooked for months or even years. But for some people, signs and symptoms develop suddenly.
Signs and symptoms of hypopituitarism vary from person to person, depending on which pituitary hormones are affected and to what degree. In people who have more than one pituitary hormone deficiency, the second deficiency may increase or, in some cases, hide the symptoms of the first deficiency.
Growth hormone (GH) deficiency
In children, GH deficiency may cause growth problems and short stature. Most adults who have GH deficiency don't have any symptoms, but for some adults it can cause:
- Fatigue
- Muscle weakness
- Changes in body fat composition
- Lack of ambition
- Social isolation
Luteinizing hormone (LH) and follicle-stimulating hormone (FSH) deficiency
Deficiency of these hormones, called gonadotropins, affect the reproductive system. In women, the deficiency decreases egg and estrogen production from the ovaries. In men, the deficiency decreases sperm and testosterone production from the testicles. Women and men may experience a lower sex drive, infertility or fatigue. In children and adolescents, delayed puberty is usually the only symptom.
Women may also have symptoms such as:
- Hot flashes
- Irregular or no periods
- Loss of pubic hair
- An inability to produce milk for breast-feeding
Men may also have symptoms such as:
- Erectile dysfunction
- Decreased facial or body hair
- Mood changes
Thyroid-stimulating hormone (TSH) deficiency
This hormone controls the thyroid gland. A TSH deficiency leads to low levels of thyroid hormones (hypothyroidism). This causes symptoms such as:
- Fatigue
- Weight gain
- Dry skin
- Constipation
- Sensitivity to cold or difficulty staying warm
Adrenocorticotropic hormone (ACTH) deficiency
This hormone helps your adrenal glands work properly, and helps your body react to stress. Symptoms of ACTH deficiency include:
- Severe fatigue
- Low blood pressure, which may lead to fainting
- Frequent and prolonged infections
- Nausea, vomiting or abdominal pain
- Confusion
Anti-diuretic hormone (ADH) deficiency
This hormone, which is also called vasopressin, helps your body balance its fluid levels. An ADH deficiency can cause a disorder called diabetes insipidus, which can cause:
- Excessive urination
- Extreme thirst
- Electrolyte imbalances
Prolactin deficiency
Prolactin is the hormone that tells the body when to start making breast milk. Low levels of prolactin can cause women to have problems making milk for breast-feeding.
When to see a doctor
See your doctor if you develop any of the signs and symptoms associated with hypopituitarism.
Contact your doctor immediately if signs or symptoms of hypopituitarism develop suddenly or are associated with a severe headache, visual disturbances, confusion or a drop in blood pressure. These could be signs and symptoms of sudden destruction of the pituitary gland tissue (pituitary apoplexy), often caused by bleeding into the pituitary gland. Pituitary apoplexy is a medical emergency and requires prompt medical attention.
Causes
Hypopituitarism has a number of causes. In many cases, hypopituitarism is caused by a tumor of the pituitary gland. As a pituitary tumor increases in size, it can compress and damage pituitary tissue, interfering with hormone production. A tumor can also compress the optic nerves, causing visual disturbances.
In addition to tumors, certain diseases or events that cause damage to the pituitary gland may also trigger hypopituitarism. Examples include:
- Head injuries
- Brain surgery
- Radiation treatment to the head or neck
- Lack of blood flow to the brain or pituitary gland (stroke) or bleeding (hemorrhage) into the brain or pituitary gland
- Certain medications, such as narcotics, high-dose corticosteroids or certain cancer drugs called checkpoint inhibitors
- Inflammation of the pituitary gland caused by an abnormal immune system response (hypophysitis)
- Infections of the brain, such as meningitis, or infections that can spread to the brain, such as tuberculosis or syphilis
- Infiltrative diseases, which affect multiple parts of the body, including sarcoidosis, an inflammatory disease occurring in various organs; Langerhans cell histiocytosis, in which abnormal cells cause scarring in numerous parts of the body; and hemochromatosis, which causes excess iron deposits in the liver and other tissues
- Severe loss of blood during childbirth, which may cause damage to the front part of the pituitary gland (Sheehan's syndrome or postpartum pituitary necrosis)
In some cases, hypopituitarism is caused by a genetic mutation (inherited). These mutations affect the pituitary gland's ability to produce one or more of its hormones, often starting at birth or in early childhood.
Tumors or diseases of the hypothalamus, a portion of the brain situated just above the pituitary, also can cause hypopituitarism. The hypothalamus produces hormones of its own that directly affect the activity of the pituitary gland.
In some cases, the cause of hypopituitarism is unknown.
Diagnosis
If your doctor suspects a problem with your pituitary hormones, he or she will likely order several tests to check hormone levels in your body and search for a cause.
Your doctor may order tests including:
- Blood tests. These tests measure your hormone levels. For example, blood tests can identify low levels of thyroid, adrenal or sex hormones. The tests can determine if these low levels are associated with pituitary hormone production.
- Stimulation or dynamic testing. These tests also measure your hormone levels. Your doctor may suggest that you go to a clinic that specializes in endocrine conditions for these tests. These tests check your body's hormone levels after you've taken certain medications to stimulate hormone production.
- Brain imaging. Magnetic resonance imaging (MRI) or high-resolution computerized tomography (CT) of your brain can detect a pituitary tumor or other pituitary gland problems.
- Vision tests. These tests can determine if growth of a pituitary tumor has impaired your sight or visual fields.
Treatment
The first step in treating hypopituitarism is often medication to help your hormone levels return to normal. This is usually called hormone replacement, because the dosages are set to match the amounts that your body would produce if it didn't have a pituitary problem. You may need to take the medication for the rest of your life.
In some cases, treatment of the condition causing hypopituitarism may lead to a complete or partial recovery of your body's ability to produce pituitary hormones.
Medications
Hormone replacement medications may include:
- Corticosteroids. These drugs, such as hydrocortisone (Cortef) or prednisone (Rayos), replace the adrenal hormones that aren't being produced because of an adrenocorticotropic hormone (ACTH) deficiency. You take them by mouth.
- Levothyroxine (Levoxyl, Synthroid, others). This medication treats the low thyroid hormone levels (hypothyroidism) that a thyroid-stimulating hormone (TSH) deficiency can cause.
- Sex hormones. These include testosterone in men and estrogen or a combination of estrogen and progesterone in women. Testosterone is administered either by injection or through the skin with a patch or a gel. Female hormone replacement can be administered with pills, gels or patches.
- Growth hormone. Also called somatropin (Genotropin, Humatrope, others), growth hormone is administered through an injection beneath your skin. It promotes growth, which helps produce a more normal height in children. Adults with symptoms of growth hormone deficiency also may benefit from growth hormone replacement, but they won't grow taller.
- Fertility hormones. If you've become infertile, gonadotropins can be administered by injection to stimulate ovulation in women and sperm production in men.
Monitoring and adjusting medication
A doctor who specializes in endocrine disorders (endocrinologist) may monitor your symptoms and the levels of these hormones in your blood to ensure you're getting the appropriate amounts.
If you're taking corticosteroids, you'll need to work with your doctor to adjust your medication dosage during times of major physical or emotional stress. During these times, your body would usually produce extra cortisol hormone to help you manage the stress.
The same kind of fine-tuning of dosage may be necessary when you have the flu, experience diarrhea or vomiting, or have surgery or dental procedures. Adjustments in dosage may also be necessary during pregnancy or with marked changes in weight.
Surgery or other procedures
You may need periodic CT or MRI scans to monitor a pituitary tumor or other diseases causing hypopituitarism. Treatment for pituitary tumors may involve surgery to remove the growth. In some cases, radiation treatment or medications are recommended to control the underlying cause.
In case of emergency
If you have hypopituitarism, it's important to wear a medical alert bracelet or pendant and carry a special card notifying others — in emergency situations, for example — of your condition. This is especially important if you're taking corticosteroids for an ACTH deficiency.
Preparing for an appointment
You're likely to start by seeing your family doctor. However, in some cases, when you call to set up an appointment, you may be referred to a doctor who specializes in endocrine disorders (endocrinologist).
Here's some information to help you prepare for your appointment.
What you can do
- Be aware of any pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do to prepare for common diagnostic tests.
- Write down all symptoms and changes you're experiencing, even if they seem unrelated to each other.
- Write down key personal information, including any recent life changes or a noticeable difference in your ability to tolerate stress.
- Make a list of your key medical information, including recent surgical procedures, the names of all medications you're taking and any other conditions for which you've been treated. Your doctor will also want to know about any prior injuries to your head or complications during childbirth.
- Take a family member or friend along, if possible. Someone who accompanies you may help you remember what your doctor tells you.
- Write down questions to ask your doctor.
Create a list of questions before your appointment so that you can make the most of your time with your doctor. For hypopituitarism, some basic questions to ask your doctor include:
- What is likely causing my symptoms or condition?
- Other than the most likely cause, what are other possible causes for my symptoms or condition?
- What tests do I need?
- Is my condition likely temporary or long-term?
- What treatment approach do you recommend?
- How long will I need to take medications?
- How will you monitor whether my treatment is working?
- I have other health conditions. How can I best manage them together?
- Are there restrictions I need to follow?
- Is there a generic alternative to the medicine you're prescribing?
- Do you have brochures or other printed material I can take with me? What websites do you recommend?
Don't hesitate to ask any questions you have during your appointment.
What to expect from your doctor
Your doctor is likely to ask you some questions, such as:
- What are your symptoms, and when did you first notice them?
- How have your symptoms changed over time?
- Have you noticed any changes in your vision?
- Do you experience severe headaches?
- Has your appearance changed, including your weight or the amount of your body hair?
- Have you lost interest in sex? Has your menstrual cycle changed?
- Are you currently being treated or have you recently been treated for any other medical conditions?
- Have you recently had a baby?
- Have you had a significant head injury or neurosurgery?
- Have you ever had radiation treatment for a head or neck tumor?
- Have any of your family members been diagnosed with pituitary or hormonal conditions?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
Copyright © 1998-2026 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.