Myocarditis is inflammation of the heart muscle (myocardium). The inflammation can reduce the heart's ability to pump blood. Myocarditis can cause chest pain, shortness of breath, and rapid or irregular heart rhythms (arrhythmias).
Infection with a virus is one cause of myocarditis. Sometimes a drug reaction or general inflammatory condition causes myocarditis.
Severe myocarditis weakens the heart so that the rest of the body doesn't get enough blood. Clots can form in the heart, leading to a stroke or heart attack.
Treatment for myocarditis may include medications, procedures or surgeries.
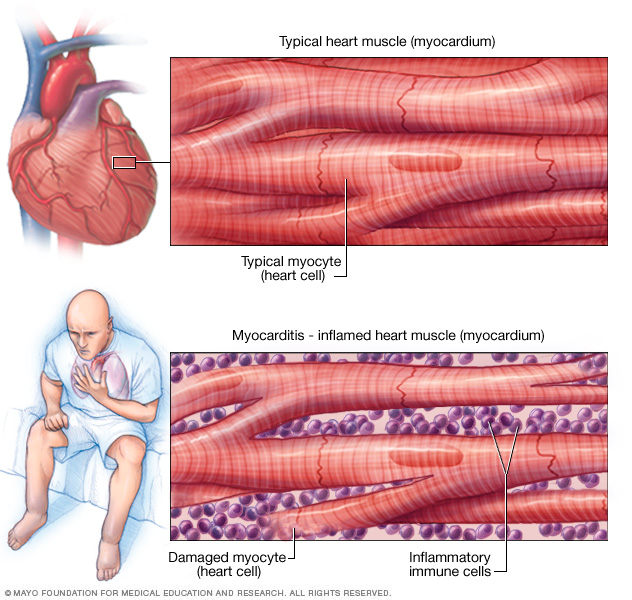
Myocarditis is inflammation of the heart muscle. This illustration shows a typical heart muscle compared to damaged heart muscle due to inflammation.
Symptoms
Some people with early myocarditis don't have symptoms. Others have mild symptoms.
Common myocarditis symptoms include:
- Chest pain
- Fatigue
- Swelling of the legs, ankles and feet
- Rapid or irregular heartbeat (arrhythmias)
- Shortness of breath, at rest or during activity
- Light-headedness or feeling like you might faint
- Flu-like symptoms such as headache, body aches, joint pain, fever or sore throat
Sometimes, myocarditis symptoms are like a heart attack. If you are having unexplained chest pain and shortness of breath, seek emergency medical help.
Myocarditis in children
When children develop myocarditis, symptoms may include:
- Breathing difficulties
- Chest pain
- Fainting
- Fever
- Rapid breathing
- Rapid or irregular heart rhythms (arrhythmias)
When to see a doctor
Contact your health care provider if you have symptoms of myocarditis. Symptoms of myocarditis can seem like a heart attack. Get emergency medical help if you have unexplained chest pain, rapid heartbeats or shortness of breath.
If you have severe symptoms, go to the emergency room or call for emergency medical help.
Causes
Myocarditis may be caused by infections, some drugs and chemicals, or a condition that causes body-wide inflammation. Often, the cause of myocarditis isn't found.
Potential causes of myocarditis include:
-
Viruses. Many viruses have been linked to myocarditis, including those that cause the common cold (adenovirus); COVID-19; hepatitis B and C; parvovirus, which causes a mild rash, usually in children (fifth disease); and herpes simplex virus.
Gastrointestinal infections (echoviruses), mononucleosis (Epstein-Barr virus) and German measles (rubella) also can cause myocarditis. Myocarditis can also be caused by HIV, the virus that causes AIDS.
- Bacteria. Bacteria that can cause myocarditis include staphylococcus, streptococcus, and bacteria that cause diphtheria and Lyme disease.
- Parasites. Among these are Trypanosoma cruzi and toxoplasma. Some parasites are transmitted by insects and can cause a condition called Chagas disease. Chagas disease is much more common in Central and South America than in the United States.
- Fungi. A fungal infection may cause myocarditis, particularly in people with weakened immune systems. Those linked to myocarditis include yeast infections, such as candida; molds, such as aspergillus; and histoplasma, often found in bird droppings.
Myocarditis may also be caused by:
- Certain medications or illegal drugs (drug-induced myocarditis). These include drugs used to treat cancer; antibiotics, such as penicillin and sulfonamide drugs; some anti-seizure medications; and cocaine.
- Chemicals or radiation. Exposure to carbon monoxide and radiation can sometimes cause heart muscle inflammation.
- Other inflammatory diseases. Conditions that may cause myocarditis include lupus, Wegener's granulomatosis, giant cell arteritis and Takayasu's arteritis.
Complications
Usually, myocarditis goes away without permanent complications. However, severe myocarditis can permanently damage the heart muscle.
Potential complications of myocarditis may include:
- Heart failure. Untreated, myocarditis can damage the heart muscle so that it can't pump blood well. In severe cases, myocarditis-related heart failure may require a ventricular assist device or a heart transplant.
- Heart attack or stroke. If the heart muscle is injured and can't pump blood, the blood that collects in the heart can form clots. A heart attack can occur if a clot blocks one of the heart (coronary) arteries. A stroke can occur if a blood clot in the heart travels to an artery leading to the brain.
- Rapid or irregular heart rhythms (arrhythmias). Damage to the heart muscle can change how the heart beats. Certain arrhythmias increase the risk of stroke.
- Sudden cardiac death. Certain serious arrhythmias can cause the heart to stop beating (sudden cardiac arrest). It's deadly if not treated immediately (sudden cardiac death).
Prevention
There's no specific prevention for myocarditis. However, taking these steps to prevent infections might help:
- Avoid close contact with people who are sick. Stay away from people with symptoms of the flu or other respiratory illness until they've recovered. If you're sick with symptoms of a viral infection, try to avoid exposing others.
- Wash your hands regularly. Frequent hand-washing is one of the best ways to avoid getting sick and spreading illness.
- Avoid risky behaviors. To reduce the chances of getting an HIV-related myocardial infection, practice safe sex and don't use illegal drugs.
- Get recommended vaccines. Stay up to date on the recommended vaccines, including those that protect against COVID-19, influenza and rubella — diseases that can cause myocarditis. Rarely, the COVID-19 vaccine can cause inflammation of the heart muscle (myocarditis) and inflammation of the outer heart lining (pericarditis), particularly in males ages 12 to 29. Talk to your health care provider about the benefits and risks of vaccines.
Diagnosis
Early diagnosis of myocarditis is important to preventing long-term heart damage. To diagnose myocarditis, a health care provider will typically examine you and listen to your heart with a stethoscope.
Blood and imaging tests may be done to check your heart health. Imaging tests can help confirm myocarditis and determine its severity.
Tests to diagnose myocarditis include:
- Blood tests. Blood tests are usually done to check for signs of a heart attack, inflammation and infection. A cardiac enzyme test can check for proteins related to heart muscle damage. Antibody blood tests may help determine if you had an infection linked to myocarditis.
- Electrocardiogram (ECG or EKG). This quick and painless test shows how the heart is beating. Your health care provider can look for signal patterns on an ECG to determine if you have irregular heartbeats (arrhythmias). Some personal devices, such as smartwatches, offer electrocardiogram monitoring. Ask your health care provider if this is an option for you.
- Chest X-ray. A chest X-ray shows the size and shape of the heart and lungs. A chest X-ray can tell if there's fluid in or around the heart that might be related to heart failure.
- Heart MRI (Cardiac MRI). This test uses magnetic fields and radio waves to create detailed images of the heart. A cardiac MRI shows the heart's size, shape and structure. It can show signs of heart muscle inflammation.
- Echocardiogram. Sound waves create moving images of the beating heart. An echocardiogram can show the heart's size and how well blood flows through the heart and heart valves. An echocardiogram can help determine if there's fluid around the heart.
- Cardiac catheterization and heart muscle biopsy. A health care provider threads a thin tube (catheter) through a blood vessel in the arm or groin to an artery in the heart. Dye flows through the catheter to help the heart (coronary) arteries show up more clearly on X-rays. A tiny sample of heart muscle tissue (biopsy) may be taken during this test. The sample is sent to a lab to be checked for inflammation or infection.
Treatment
Often, myocarditis improves on its own or with treatment. Myocarditis treatment focuses on the cause and the symptoms, such as heart failure.
Medications
People with mild myocarditis may only need rest and medication. Medications to treat myocarditis may include:
- Corticosteroids. These medicines suppress the immune system. They may be used to treat some rare types of viral myocarditis, such as giant cell and eosinophilic myocarditis.
-
Heart medications. If myocarditis is causing severe heart failure or irregular heartbeats, drugs may be given to reduce the risk of blood clots in the heart.
For a weak heart, medications can help remove extra fluid from the body and reduce the strain on the heart. Some types of medications that may be given are diuretics, beta blockers, angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs).
- Medications to treat chronic conditions. Sometimes another health condition, such as lupus, causes myocarditis. Treating the underlying condition may help reduce heart muscle inflammation.
Some people with myocarditis may need medications for just a few months and then recover completely. Others may have long-term, permanent heart damage that needs lifelong medication. It's important to have regular health checkups after a diagnosis of myocarditis to check for possible complications.
Surgeries and procedures
If you have severe myocarditis, you will need aggressive treatment, which might include:
- IV medications. Medications given through an IV are used to quickly improve the heart's ability to pump.
- Ventricular assist device (VAD). A VAD helps pump blood from the lower chambers of the heart (the ventricles) to the rest of the body. It's a treatment for a weakened heart or heart failure. A VAD may be used to help the heart work while waiting for other treatments, such as a heart transplant.
- Intra-aortic balloon pump. This device helps increase blood flow and lower the strain on the heart. The heart doctor (cardiologist) inserts a thin tube (catheter) into a blood vessel in the leg and guides it to the heart. A balloon attached to the end of the catheter inflates and deflates in the main artery leading out to the body from the heart (aorta).
-
Extracorporeal membrane oxygenation (ECMO). An ECMO machine works like the lungs.It removes carbon dioxide and adds oxygen to the blood. If you have severe heart failure, this device can send oxygen to your body. During ECMO, blood is removed from the body, passed through the machine and then returned to the body.
ECMO may be used to help the heart to recover or while waiting for other treatments, such as a heart transplant.
- Heart transplant. An urgent heart transplant may be needed for those who have very severe myocarditis.
Lifestyle and home remedies
Rest and reducing the strain on the heart is an important part of myocarditis recovery. If you have or had myocarditis, ask your health care provider which type and amount of physical activity is safe for you.
If you have myocarditis, you should avoid competitive sports for at least 3 to 6 months.
Following a healthy lifestyle is an important part of myocarditis treatment and recovery. Try these heart-healthy strategies:
- Limit salt.
- Avoid or limit alcohol.
- Don't smoke.
Some people may need to restrict fluids. Ask your care provider what your fluid intake should be.
Preparing for an appointment
If you have mild myocarditis symptoms, you may start with your primary care provider. If symptoms are severe, you may first be seen by an emergency room care provider. You'll likely be referred to a doctor trained in heart conditions (cardiologist) and possibly a doctor trained in infectious disease.
What you can do
Here's some information to help you get ready for your appointment. Write down the following details:
- Your symptoms, including any that might seem unrelated to myocarditis, and when they began
- Important personal information, including recent illnesses and the symptoms, recent travel locations, and your and your family's medical history
- All medications, vitamins or other supplements you take, including doses
- Questions to ask your health care provider
For myocarditis, basic questions to ask your care provider include:
- What's the most likely cause of my symptoms?
- What are other possible causes?
- What tests do I need?
- How is myocarditis treated?
- What side effects can I expect from treatment?
- Are there alternatives to the primary approach you're suggesting?
- I have other health conditions. How can I best manage these conditions together?
- Do I need to restrict my activities or diet?
- Are there brochures or other printed material I can have? What websites do you recommend?
Don't hesitate to ask other questions. Take a family member or friend along to your appointment, if possible, to help you remember the information you'll receive.
What to expect from your doctor
Your care provider is likely to ask many questions, including:
- Have you recently been sick or have you recovered from another illness?
- Have you traveled out of the country recently?
- What, if anything, makes symptoms better?
- What, if anything, makes your symptoms worse?
Copyright © 1998-2026 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.