Vocal cord paralysis is a condition in which you can't control the movement of the muscles that control your voice. It happens when the nerve impulses to your voice box (larynx) are disrupted. This results in paralysis of the vocal cord muscles.
Vocal cord paralysis can make it hard to speak and even breathe. That's because your vocal cords, also called vocal folds, do more than just produce sound. They also protect your airway by preventing food, drink and even your saliva from entering your windpipe (trachea) and causing you to choke.
Possible causes of vocal cord paralysis include nerve damage during surgery, viral infections and certain cancers. Treatment for vocal cord paralysis usually involves surgery, and sometimes voice therapy.
Symptoms
Your vocal cords are two flexible bands of muscle tissue that sit at the entrance to the windpipe (trachea). When you speak, the bands come together and vibrate to make sound. The rest of the time, the vocal cords are relaxed in an open position so that you can breathe.
In most cases of vocal cord paralysis, only one vocal cord is paralyzed. Paralysis of both of your vocal cords is a rare but serious condition. This can cause difficulties with speech and significant problems with breathing and swallowing.
Signs and symptoms of vocal cord paralysis may include:
- A breathy quality to the voice
- Hoarseness
- Noisy breathing
- Shortness of breath
- Loss of vocal pitch
- Choking or coughing while swallowing food, drink or saliva
- The need to take frequent breaths while speaking
- Inability to speak loudly
- Loss of your gag reflex
- Ineffective coughing
- Frequent throat clearing
When to see a doctor
If you have unexplained hoarseness that lasts for more than 2 to 4 weeks, or if you notice any unexplained voice changes or discomfort, contact your health care provider.
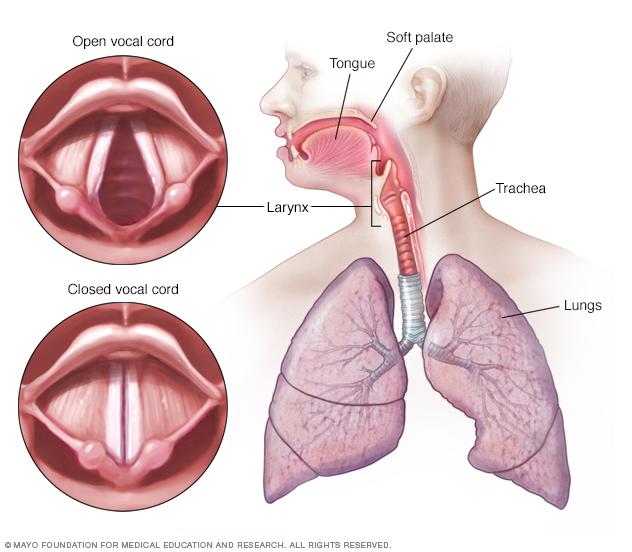
Vocal cords open when you breathe and then close to produce sound when vibrating together.
Causes
In vocal cord paralysis, the nerve impulses to your voice box (larynx) are disrupted, causing paralysis of the muscle. Health care providers often can't determine the exact cause of vocal cord paralysis. But some known causes may include:
- Injury to the vocal cord during surgery. Surgery on or near the neck or upper chest can result in damage to the nerves that serve the voice box. Surgeries that carry a risk of damage include surgeries to the thyroid or parathyroid glands, esophagus, neck, and chest.
- Neck or chest injury. Trauma to the neck or chest may injure the nerves that serve the vocal cords or the voice box itself.
- Stroke. A stroke interrupts blood flow in the brain and may damage the part of the brain that sends messages to the voice box.
- Tumors. Tumors, both cancerous and noncancerous, can grow in or around the muscles, cartilage or nerves controlling the function of the voice box and can cause vocal cord paralysis.
- Infections. Some infections, such as Lyme disease, Epstein-Barr virus and herpes, can cause inflammation and directly damage the nerves in the voice box. There's some evidence that infection with COVID-19 may cause vocal cord paralysis.
- Neurological conditions. Certain neurological conditions, such as multiple sclerosis or Parkinson's disease, can lead to vocal cord paralysis.
Risk factors
Factors that may increase your risk of developing vocal cord paralysis include:
- Undergoing throat or chest surgery. People who need surgery on their thyroid, throat or upper chest have an increased risk of vocal cord nerve damage. Sometimes the breathing tubes used in surgery or to help you breathe if you're having serious respiratory trouble can damage the vocal cord nerves.
- Having a neurological condition. People with certain neurological conditions — such as Parkinson's disease or multiple sclerosis — are more likely to develop vocal cord weakness or paralysis.
Complications
Breathing problems associated with vocal cord paralysis may be so mild that you just have a hoarse-sounding voice, or they can be so serious that they're life-threatening.
Because vocal cord paralysis keeps the opening to the airway from completely opening or closing, other complications may include choking on or inhaling (aspirating) food or liquid. Aspiration that leads to severe pneumonia is rare but serious and requires immediate medical care.
Diagnosis
Your health care provider likely asks about your symptoms and lifestyle, listens to your voice, and asks you how long you've had voice problems. To further evaluate your voice problems, the following tests may be performed:
-
Laryngoscopy. Your health care provider looks at your vocal cords using a mirror or a thin, flexible tube (known as a laryngoscope or endoscope) or both. You may also have a test called videostrobolaryngoscopy. It uses a special scope that contains a tiny camera at its tip or a larger camera connected to the scope's viewing piece.
These special high-magnification endoscopes allow your care provider to view your vocal cords directly or on a video monitor to determine the movement and position of the vocal cords and whether one or both vocal cords are affected.
-
Laryngeal electromyography. This test measures the electrical currents in your voice box muscles. To do this, the health care provider typically inserts small needles into the vocal cord muscles through the skin of the neck.
This test isn't used to guide treatment, but it may give your provider information about how well you may recover. This test is most useful when it's done between six weeks and six months after your symptoms began.
- Blood tests and scans. Because a number of diseases may cause nerve injuries, you may need additional tests to identify the cause of the paralysis. Tests may include blood work, X-rays, MRI or CT scans.
Treatment
Treatment of vocal cord paralysis depends on the cause, the severity of symptoms and the time from the onset of symptoms. Treatment may include voice therapy, bulk injections, surgery or a combination of treatments.
In some instances, you may get better without surgical treatment. For this reason, your health care provider may delay permanent surgery for at least a year from the beginning of your vocal cord paralysis.
However, surgical treatment with various bulk injections is often done within the first three months of voice loss.
During the waiting period for surgery, your provider may suggest voice therapy to help keep you from using your voice improperly while the nerves heal.
Voice therapy
Voice therapy sessions involve exercises or other activities to strengthen your vocal cords, improve breath control during speech, prevent tension in other muscles around the paralyzed vocal cord or cords, and protect your airway during swallowing. Occasionally, voice therapy may be the only treatment you need if your vocal cords were paralyzed in a location that doesn't require additional bulk or repositioning.
Surgery
If your vocal cord paralysis symptoms don't fully recover on their own, surgical treatments may be offered to improve your ability to speak and to swallow.
Surgical options include:
- Bulk injection. Paralysis of the nerve to your vocal cord will probably leave the vocal cord muscle thin and weak. To add bulk to a paralyzed vocal cord, a doctor who specializes in disorders of the larynx (laryngologist) may inject your vocal cord with a substance such as body fat, collagen or another approved filler substance. This added bulk brings the affected vocal cord closer to the middle of your voice box so that the opposite functioning and moving vocal cord can make closer contact with the paralyzed cord when you speak, swallow or cough.
- Structural implants. Instead of using a bulk injection, this procedure — known as thyroplasty, medialization laryngoplasty or laryngeal framework surgery — relies on the use of an implant in the larynx to reposition the vocal cord. Rarely, people who have this surgery may need to have a second surgery to reposition the implant.
- Vocal cord repositioning. In this procedure, a surgeon moves a window of your own tissue from the outside of your voice box inward, pushing the paralyzed vocal cord toward the middle of your voice box. This allows your unimpaired vocal cord to better vibrate against its paralyzed partner.
- Replacing the damaged nerve (reinnervation). In this surgery, a healthy nerve is moved from a different area of the neck to replace the damaged vocal cord. It can take as long as 6 to 9 months before your voice gets better. Some health care providers combine this surgery with a bulk injection.
-
Tracheotomy. If both of your vocal cords are paralyzed and positioned closely together, your airflow will be decreased. This causes a lot of trouble breathing and requires a surgery called a tracheotomy.
In a tracheotomy, an incision is made in the front of your neck to create an opening in the windpipe (trachea). A breathing tube is inserted, allowing air to bypass the vocal cords.
Emerging treatments
Linking the vocal cords to another source of electrical stimulation — perhaps a nerve from another part of the body or a device similar to a cardiac pacemaker — may restore opening and closing of the vocal cords that can't move. Researchers continue to study this and other options.
Coping and support
Vocal cord paralysis can be frustrating and affect your daily life. It can be hard to communicate with other people. A speech therapist can help you develop the skills you need to communicate.
Even if you're not able to get back the voice you once had, voice therapy can help you learn effective ways to make up for it. In addition, a speech-language pathologist can teach you how to use your voice without causing further damage to the vocal cords.
Preparing for an appointment
You're likely to first see your primary care provider unless both vocal cords are paralyzed. In that case, you'll probably first be seen in a hospital emergency department.
After the initial assessment, you'll likely be referred to a doctor who specializes in ear, nose and throat disorders. You may also be referred to a speech-language pathologist for voice assessment and therapy.
It's helpful to arrive well prepared for your appointment. Here's some information to help you get ready and what to expect from your care provider.
What you can do
- Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent illnesses or life changes.
- Make a list of all medications, vitamins or supplements that you're taking, including the dose of each.
- Ask a family member or friend to come with you, if possible. Sometimes it can be difficult to remember all of the information provided to you during an appointment. Someone who is with you may remember something that you missed or forgot.
- Write down questions to ask your provider.
Your time with your health care provider may be limited. Preparing a list of questions can help you make the most of your time together. For vocal cord paralysis, some basic questions to ask your provider include:
- What's the most likely cause of my vocal cord paralysis?
- What kinds of tests do I need? Do these tests require any special preparation?
- Is this condition temporary, or will my vocal cords always be paralyzed?
- What treatments are available, and which do you recommend?
- What types of side effects can I expect from treatment?
- Are there any alternatives to the treatment that you're suggesting?
- Are there any restrictions on using my voice after treatment? If so, for how long?
- Will I be able to talk or sing after treatment?
- Are there any brochures or other printed material that I can take home with me?
In addition to the questions that you've prepared to ask, don't hesitate to ask any additional questions that occur to you during your appointment.
What to expect from your doctor
Your health care provider is likely to ask you a number of questions, such as:
- When did your symptoms start?
- Did any special events or circumstances happen before or at the same time that your symptoms developed?
- Have you received any treatment yet?
- Have your symptoms been continuous or do they come and go?
- How are your symptoms affecting your lifestyle?
- Does anything seem to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Do you have any other medical conditions?
Copyright © 1998-2026 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.