Coughing, wheezing, difficulty taking a deep breath — having an asthma attack can be frightening.
The key to asthma treatment is prevention. That means avoiding things that trigger your attacks and taking medication as needed to help prevent future attacks. You also should know what to do if your symptoms suddenly get worse.
Everyone with asthma should work with their doctor to create an individualized asthma action plan, to keep their asthma in check.
What is asthma?
Asthma is a chronic (long-term) lung condition that can make it difficult to breathe.
Normally when you take a breath, air passes easily from your nose and mouth into your trachea, which divides into tubes called bronchi. The bronchi enter the lungs and divide into a system of increasingly smaller airways.
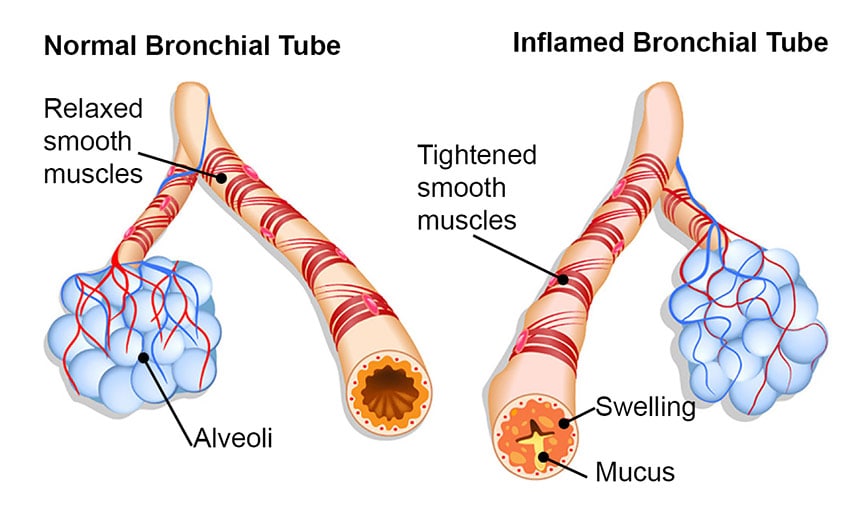
During an asthma attack, the airways narrow and become inflamed. This leads to breathing difficulties and wheezing. Mucus produced by the inflammation fills the narrowed passageways. As a result, the flow of air is partially or completely blocked.
Asthma usually first appears in childhood. But it can also develop for the first time later in life. We don’t know why some people get asthma. You may be more likely to develop it, though, if others in your family have asthma or allergies.
Symptoms of asthma
Asthma ranges from mild to severe.
Some people have only occasional, mild symptoms. Others have nearly constant symptoms with severe, life-threatening flare-ups.
Symptoms of asthma can include:
- wheezing
- tight sensation in the chest
- shortness of breath or difficulty breathing
- coughing, especially at night
For some people with asthma, a chronic cough is the main symptom.
Symptoms of a severe asthma attack, or flare-up, can include:
- extreme shortness of breath
- a rapid pulse
- sweating
- flared nostrils and pursed lips
- a need to sit upright
- blue tinge to lips and fingernails
People with asthma tend to have more severe symptoms when they have an upper respiratory infection, such as a cold or the flu.
What to expect from treatment
Asthma treatment focuses as much on preventing asthma attacks as it does on treating attacks if they do occur.
The main components of asthma treatment are:
- Identifying and avoiding asthma triggers
- Taking preventive medications as needed
- Using rescue medications when you have signs or symptoms of an asthma attack
Asthma symptoms tend to vary over time. When you visit your doctor for a check-up, describe how your asthma has been for the past few weeks to months.
For example:
- Have you had to go to the emergency room because of a severe asthma attack?
- How often have you had to miss work or cancel plans because of asthma?
- How often do you awaken at night due to coughing or shortness of breath?
- How often does asthma limit your physical activities?
- How often do you need to use your rescue medications?
Depending on your answers, your doctor may re-evaluate your asthma treatment regimen.
Asthma triggers
An important part of managing your asthma is to identify and try to avoid the triggers that make your symptoms flare.
By avoiding or limiting your exposure to anything that triggers your asthma symptoms, you may be able to minimize or perhaps even eliminate the need for some asthma medicines.
The following are common asthma triggers:
- allergens such as dust mites, mold and mildew, pet dander, and pollen
- irritants in the air, like exhaust fumes, smoke from burning tobacco or wood, strong odors, pollution, chemicals, or dust
- respiratory infections such as bronchitis, a cold, or the flu
- exercise
- cold, dry weather
- certain medications, including beta blockers and other medicines used to treat high blood pressure
Some people with asthma can’t identify any triggers.
Medications
Control medications
Control medications are taken every day, even when you don’t have symptoms, to help prevent asthma attacks.
Some people with asthma need to take a controller medicine only during allergy season or following a respiratory infection. Others need to take preventive medicines year-round.
Your doctor will likely ask you to take controller medicines if you have frequent or severe asthma flare-ups.
Anti-inflammatory medicines—usually a corticosteroid—reduce swelling and inflammation of the bronchial tubes. This makes the airways less sensitive to asthma triggers. These medicines are usually inhaled. They also can be taken as pills when the inhaled version is not effective.
Long-acting bronchodilators relax the bronchial muscles. This helps to improve airflow by preventing muscle spasms that narrow the bronchial tubes. These medicines are usually inhaled. They must be taken together with an anti-inflammatory inhaler.
Some controller medications both reduce inflammation and help keep the airways open. Controller medications also help reduce mucus production.
Preventive medicines don’t ease symptoms right away. But they provide long-term control.
Rescue medicines
Rescue medicines, or “quick relievers,” work fast to ease wheezing, coughing, and chest tightness.
Rescue medicines are fast-acting bronchodilators that you inhale. They provide relief within minutes by relaxing the muscles that surround the bronchial tubes, allowing the airways to open wider.
These medicines should be taken at the first sign of an asthma attack. For example, you would use a rescue medication if you:
- have more wheezing
- are coughing more often
- have more mucus or phlegm
- are becoming short of breath quickly with exertion or exercise
If you are using your rescue medication often, your asthma is not well-controlled. Your doctor may need to adjust your control medication.
Using an Inhaler
Most asthma medications are breathed in through an inhaler or nebulizer.
Inhalers are small canisters that deliver puffs of medication. You must inhale at the right moment, to ensure the medicine passes into your lower airways.

A spacer can make it easier to use an inhaler. A spacer is a hollow chamber that fits onto your inhaler. Instead of spraying the medication into your mouth, you spray it into the chamber. You then inhale the medicine from the chamber, without the need for perfect timing.

Nebulizers deliver a fine mist of medicine through a mouthpiece or face mask as you breathe normally for several minutes.

If you don’t use an inhaler or nebulizer correctly, little or no medicine reaches your lungs. Ask your doctor if you are using your device properly.
Your asthma action plan
Everyone with asthma should have an asthma action plan.
This is a written plan that details what you need to do to control your asthma. It also explains what to do when you experience asthma symptoms or in case of an emergency.
Asthma action plans are often divided into “zones.” You should be able to tell what zone you are in from your symptoms. The action plan will tell you what you need to do in each zone.
For example:
Green Zone: Doing well. No coughing, wheezing, chest tightness, or shortness of breath; can do all usual activities. Take long-term controller medicine as prescribed.
Yellow Zone: Getting worse. Coughing, wheezing, chest tightness, or shortness of breath; waking at night; can do some, but not all, usual activities. Add quick-relief medicine.
Red Zone: Medical alert! Very short of breath; quick-relief medicines don’t help; cannot do usual activities; symptoms no better after 24 hours in yellow zone. Get medical help now.
It’s a good idea to make sure your asthma action plan includes the nearest emergency department and its contact information.
Asthma and allergies
Some people with asthma notice their asthma acts up after exposure to allergic triggers.
These triggers may include pollen, pet dander, or dusty environments. In other people, asthma symptoms are not triggered by allergens.
You can take steps to minimize your exposure to some common allergens.
Dust mites
Dust mites are tiny bugs that are typically found anywhere dust accumulates. Encase mattresses in airtight covers.
- Clean your home frequently.
- Wash bedding frequently in very hot water.
- Remove carpets and heavy draperies from bedrooms.
Pollen or outdoor mold
Stay indoors as much as possible. Close the windows and keep the air conditioner on — at home and in your car. Remove your shoes and outer garments after coming into the house from outdoors. Shower before going to bed.
Pet dander and saliva
Keep pets out of bedrooms and bathe them regularly. Vacuum your home frequently. If this isn’t sufficient, you may need to find another loving home for your pet.
Your doctor may also suggest allergy medicines to reduce asthma symptoms triggered by allergies.
Exercise-induced asthma
For some people, physical activity triggers asthma symptoms. This is called exercise-induced asthma.
An attack of asthma brought on by exercise is generally short-lived. The bronchial muscles usually begin to relax within minutes. And breathing tends to return to normal within an hour.
Staying calm is a good strategy for any asthma attack. Breathe slowly and deeply. Try inhaling for a count of one and exhaling for a count of three.
If you have exercise-induced asthma:
- Ask your doctor if you should use your rescue inhaler before exercise.
- Warm up before exercising.
- Always keep your rescue inhaler with you when you exercise.
- If you start to have symptoms during exercise, stop exercising.
- Use your rescue inhaler if needed.
- Don’t exercise on days when your asthma is bad.
How to exercise safely with asthma
Everyone with asthma should take precautions when exercising.
Even if physical activity does not trigger your asthma symptoms, other triggers in your exercise environment—like cold weather or pollen—could be a problem. Always carry your rescue inhaler with you when you exercise.
If cold, dry air triggers your symptoms:
- Wear a face mask or scarf over your nose and mouth to trap some warm, moist air.
- Exercise indoors in cold weather.
- Consider swimming during the winter months. Indoor pool areas are usually warm and humid.
If pollen triggers your symptoms:
- Breathe in through your nose, which filters the air.
- Exercise indoors, with the air conditioner on, when the pollen count is high.
- Don’t let the fear of an asthma attack keep you from exercising.
Living well with asthma
Adopt healthy habits to reduce asthma symptoms—and improve your overall health.
Say goodbye to tobacco. Don’t smoke, and don’t allow others to smoke in your home. Tobacco smoke of any kind can irritate your airways. Even secondhand smoke can trigger asthma attacks.
Treat acid reflux. Also known as GERD, acid reflux can make asthma symptoms worse. Ask your doctor about lifestyle changes and medications to treat it.
Avoid respiratory infections. Respiratory infections like a cold, the flu, or pneumonia can worsen your asthma and lead to serious complications. The following steps can help reduce your risk of infection:
- Wash your hands frequently with soap and warm water. If you can’t get to a sink, use an alcohol-based hand sanitizer.
- Try not to touch your eyes, nose, or mouth. Germs often spread when you touch something that is contaminated and then touch those areas of your face.
- Get a flu shot every year.
- Ask your doctor if you should get a pneumococcal vaccine to protect against bacterial pneumonia.
With a specific asthma control plan from your doctor and steps to avoid things that trigger your attacks, you can control your asthma. Take your medications as prescribed and ask your doctor what to do if your symptoms suddenly worsen. Remember, the key to asthma treatment is prevention.
Talk with your doctor
The more your doctor knows about your symptoms, the better he or she can help you manage them.
Describe your symptoms to your doctor at every appointment. Your doctor will want to know:
- What seems to trigger your symptoms?
- Have your symptoms improved or gotten worse since your last visit?
- Do your symptoms keep you from your normal activities?
- Are you waking up at night because of trouble breathing?
- How often do you use your rescue inhaler?
Ask your doctor:
- Am I using my inhaler correctly?
- What precautions should I take when I exercise?
- Do I need to adjust my medications during allergy or cold and flu season?
Tell your doctor if you think your medicines are causing side effects.