
Rheumatoid arthritis is a long-lasting inflammatory disease that causes painful, stiff, red, and swollen joints. Rheumatoid arthritis can get in the way of doing things you enjoy. But it doesn’t have to be disabling. Self-care strategies, medications, and non-drug treatments can help you protect your joints, ease pain, and stay active.
What is rheumatoid arthritis?
Rheumatoid arthritis is a disease that affects multiple joints.
A healthy immune system protects the body. A healthy immune system fights harmful invaders like viruses and bacteria. If you have an injury, the immune system helps it heal.
In rheumatoid arthritis, the immune system attacks the joints. In rheumatoid arthritis, the immune system mistakenly attacks healthy joint tissue. This causes inflammation. The joints swell and become painful, red, and stiff.
Rheumatoid arthritis causes joint damage. Over time, inflammation can permanently damage joints and nearby tissues. Rheumatoid arthritis tends to affect many joints at once, especially in the hands and feet. As it gets worse, the disease can make it hard to do simple daily activities, such as dressing, bathing, and walking.
Rheumatoid arthritis is a lifelong condition. Rheumatoid arthritis usually begins during middle age. It is a chronic (ongoing) disease that tends to get worse over time.

A closer look at the joints
Joints are places where bones meet.
Rheumatoid arthritis affects synovial joints.
Synovial joints are movable joints. The shoulders, elbows, wrists, fingers, hips, knees, ankles, and toes all have synovial joints. So do your neck and jaw. These joints allow a range of movements. They make it possible to do a variety of activities, from tying your shoes to playing tennis.
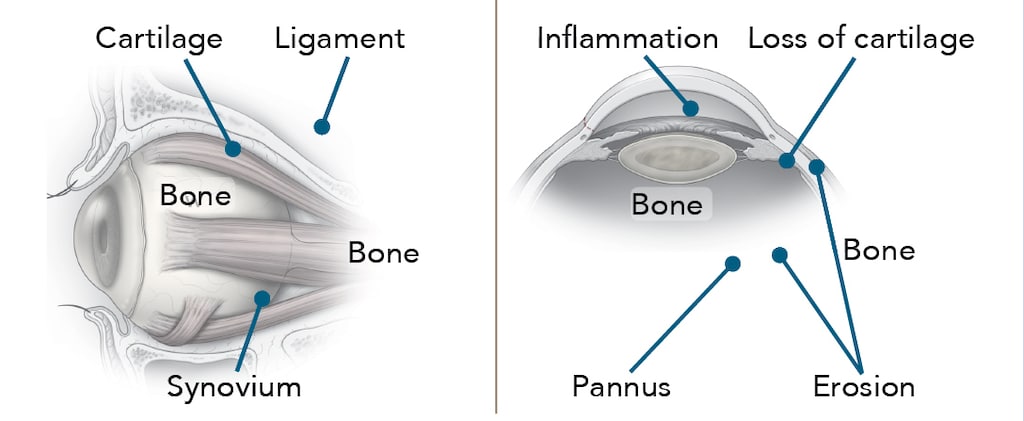
Synovial joints take their name from the synovium, the tissue that lines the joint. The synovium produces synovial fluid. This thick liquid lubricates the joint and reduces friction. It also forms a sticky seal that lets neighboring bones slide freely against each other without pulling apart.
A tough and somewhat elastic tissue called cartilage covers the ends of the bones where they meet in the joints. Cartilage acts as a protective cushion.
Joint changes in rheumatoid arthritis
Inflammation caused by rheumatoid arthritis can damage joints.
Rheumatoid arthritis occurs when the immune system mistakenly attacks the joints. In a normal immune response, inflammation dies down when an infection clears or an injury heals. But in rheumatoid arthritis, the immune system continues to attack the joints.
When inflammation begins in the synovium of an otherwise normal joint, synovial cells begin to multiply and form a rough, grainy tissue called pannus. This tissue eventually grows into the space between the bones.
Cells in the pannus release substances that eat away at cartilage and bone. This causes the bone to break down.
The damage often does not stop there. Nearby structures within the joint may also become inflamed. All of this damage can cause pain, instability, deformity, weakness, and loss of motion.
Symptoms of rheumatoid arthritis
Joints in the hands, wrists, and feet are the most common targets of rheumatoid arthritis.
You may experience the following symptoms around affected joints:
- pain
- swelling
- limited range of motion
- warmth
- tightness
- prolonged stiffness in the morning
Eventually, joint pain may become constant. Joints become so damaged that it is hard to move them.
Other, body-wide symptoms may include:
- fatigue, soreness, stiffness, and aching
- weight loss
- low-grade fever and sweats
In addition to the joints, the disease can affect the skin, eyes, lungs, blood vessels, and the lining of the heart.
How is rheumatoid arthritis diagnosed?
Clearly and accurately describing your symptoms will help your doctor diagnose your condition.
Your doctor will do a physical examination to look for:
- joint swelling, redness, and tenderness
- limited range of motion
- joint deformities
He or she will ask if anyone in your family has arthritis or another related condition. You may have blood and imaging tests.
Your symptoms provide important clues for diagnosis. Be prepared to discuss the following:
- How do your joints feel? Are they swollen? Stiff? Painful?
- Are you particularly stiff in the morning? How long does the stiffness last?
- Does activity increase your pain, or relieve it?
- Did your symptoms start gradually or suddenly? Have they worsened over time?
- Did any notable event — like an illness, injury, or infection — occur when your joint symptoms first appeared?
- Have you had fever, fatigue, weight loss, or skin problems?
Keep a record of your symptoms starting two weeks before your appointment. Note the intensity of your pain, how long it lasts, and what it feels like.
What else could it be?
Early symptoms of other conditions can look like rheumatoid arthritis.
Before diagnosing rheumatoid arthritis, your doctor will want to rule out these conditions:
- Osteoarthritis. This condition, the most common form of arthritis, causes joint pain that can be similar to the pain of rheumatoid arthritis.
- Lupus. Lupus is another inflammatory immune disease. Fever and joint pain are common early symptoms.
- Scleroderma. This disease causes skin to thicken, tighten, and shine.
- Sjögren’s syndrome. This immune disease causes dry eyes and dry mouth. It can also cause joint pain and swelling that mimic rheumatoid arthritis.
- Gout and pseudogout. These painful forms of arthritis develop when tiny crystals accumulate in joints, causing swelling and extreme joint sensitivity.
Medical treatments for rheumatoid arthritis
Treatment prevents or slows joint damage and loss of function and reduces pain.
There is no cure for rheumatoid arthritis. But medications can help most people with rheumatoid arthritis avoid disability.
Disease-modifying antirheumatic drugs (DMARDs)
Rheumatoid arthritis begins to damage joints early in the course of the disease. Starting disease-modifying treatment as soon as possible can help reduce or prevent joint damage and preserve joint function. DMARDs provide good symptom relief. They let many people maintain normal or near-normal function. As with all drugs, they have possible side effects, and some may be serious.
Most people start taking DMARDs soon after they learn they have rheumatoid arthritis. There are three main types:
- Non-biologic DMARDs. Non-biologic DMARDs help suppress an overactive immune system. This reduces inflammation.
- Biologic DMARDs. So-called “biologics” are genetically engineered proteins. They block specific steps in the process of inflammation. This group includes drugs known as TNF inhibitors as well as non-TNF biologics.
- JAK inhibitor. This drug blocks a specific pathway involved in the body’s immune response.
- The particular combination of DMARD drugs needed to control rheumatoid arthritis varies from person to person.
Medications that reduce pain and inflammation
These drugs relieve pain, swelling, and other symptoms, but they cannot stop the disease from getting worse.
NSAIDs. Nonsteroidal anti-inflammatory drugs (NSAIDs) relieve pain. They also reduce inflammation, which contributes to pain, swelling, and stiffness.
There are two types of NSAIDs: non-selective NSAIDs and selective COX-2 inhibitors. COX-2 inhibitors tend to cause less stomach and intestinal irritation. Both types are associated with an increased risk of heart disease.
Corticosteroids. These drugs decrease inflammation. They may be taken as a pill or injected into a joint. They have many potential side effects.
Surgery
Thanks to earlier use of disease-slowing drugs nowadays, surgery usually isn’t needed to treat rheumatoid arthritis.
Surgery may be helpful when drug treatment alone doesn’t improve pain or mobility. Surgery can help reduce pain, improve function, or correct a deformity.
Surgery may be used to:
- remove inflamed tissue within a joint
- fuse bones together to relieve pain, correct deformities, or improve appearance
- replace damaged joints with artificial joints to relieve pain and restore function
Non-drug treatment strategies
Non-drug treatments are important for managing rheumatoid arthritis.
Treatments like these can help you be an active participant in your own care.
Physical and occupational therapy
Physical activity strengthens joints and improves range of motion.
Work with a physical therapist to find exercises that build strength and flexibility while protecting vulnerable joints.
An occupational therapist can show you how to ease pressure on your joints during routine activities at work or at home.
Heat therapy
Heat makes pain more tolerable and relaxes muscles. Try taking a warm bath or shower, or place a heating pad on a painful joint.
Cold therapy
Cold can relieve joint pain and decrease inflammation and muscle spasms. Gel-filled cold packs work well, as does a bag of frozen vegetables.
Splints, braces, orthotics, and canes
Splints immobilize an injured or inflamed body part (such as the hand or wrist). Splints can relieve pain, realign joints, and help you function. Braces and orthotics can help improve balance and normalize your walking pattern when foot and ankle joints are affected. Knee braces reduce the strain of walking on the knee. A cane can take pressure off the hip.
Alternative and complementary therapies
Some people find extra relief through alternative and complementary therapies.
Talk to your doctor before trying any of these therapies.
- Acupuncture involves inserting tiny, sterile needles into the skin to relieve pain. It causes little to no pain.
- With mindfulness meditation, you focus your attention on the present moment. It helps some people cope with pain.
- Relaxation training uses breathing and other techniques to create a sense of calm and to decrease pain and tension.
- Tai chi is a low-impact exercise that emphasizes breathing and mental focus while moving through a series of motions.
- Yoga combines physical postures, breathing exercises, and meditation. You may need to modify certain positions to avoid stressing affected joints.
- Omega-3 fatty acids, found in fish oil supplements, may help dampen inflammation.
Adjust your routine to protect your joints
Simple adjustments can help you protect your joints.
Not using arthritic joints enough, overusing them, or using them incorrectly can all worsen pain and swelling and cause additional joint damage.
Tips to protect your joints
The following strategies can help you avoid stiffness and unnecessary stress on joints.
- Avoid holding one position for too long.
- Get up and stretch every 15 minutes when reading, watching TV, or working at your desk.
- Modify tasks to ease the workload on your joints.
- For example, if opening tight lids is difficult, purchase a wall-mounted jar opener.
- Use your strongest joints and muscles.
- To protect finger and wrist joints, push open heavy doors with the side of your arm or shoulder.
- To reduce hip or knee stress on stairs, lead with the stronger leg going up and the weaker leg going down.
- Prevent falls, which can further damage your joints and cause disability.
- Remove throw rugs.
- Place a suction mat and grab bar in the bathtub.
- Use night lights in the bedroom, hallway, and bathroom.
Make use of helpful gadgets
Simple gadgets and devices can make it easier to perform daily activities.
In the kitchen
- mini-chopper
- electric mixer
- utensils with built-up, padded handles
- faucet handles that can be turned with the arm, wrist, or heel of the hand
In the bathroom
- electric toothbrush
- pump-style toothpaste and soap dispensers
- electric razor
- raised toilet seat
In your closet
- slip-on shoes
- clothing with elastic waistbands, large buttons, Velcro fastenings, and zipper pulls
- magnetic jewelry clasps
Throughout your home
- doorknob turners
- phone with voice commands
- voice recognition software for your computer
Talk with your doctor
Whether this is your first visit or a follow-up, ask your doctor:
- What are my drug treatment options? Which one is best for me, and why?
- What non-drug treatments can help relieve my symptoms?
- What lifestyle changes should I make to prevent further joint damage and to relieve my discomfort?
Describe your symptoms to your doctor at every appointment. What symptoms do you have?
How long do they last? To what extent do they affect your daily activities?
Tell your doctor if:
- your symptoms have changed (for better or worse) since your last visit
- you have had to increase the amount of pain medication you take
- you think your medications are causing any side effects
- you are trying any alternative or complementary therapies.
As with any disease, it’s most important that you get an accurate diagnosis from your physician. Treatments for rheumatoid arthritis are available, and the sooner you’re able to begin, the easier things will become.




