Boxed Warning
Serious GI adverse reactions:
Infrequent but serious GI adverse reactions have been reported with the use of alosetron. These reactions, including ischemic colitis and serious complications of constipation, have resulted in hospitalization, and, rarely, blood transfusion, surgery, and death.
Alosetron is indicated only for women with severe diarrhea-predominant irritable bowel syndrome (IBS) who have not responded adequately to conventional therapy.
Alosetron should be discontinued immediately in patients who develop constipation or symptoms of ischemic colitis. Patients should immediately report constipation or symptoms of ischemic colitis to their health care provider. Alosetron should not be resumed in patients who develop ischemic colitis. Patients who have constipation should immediately contact their health care provider if the constipation does not resolve after alosetron is discontinued. Patients with resolved constipation should resume alosetron only on the advice of their treating health care provider.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
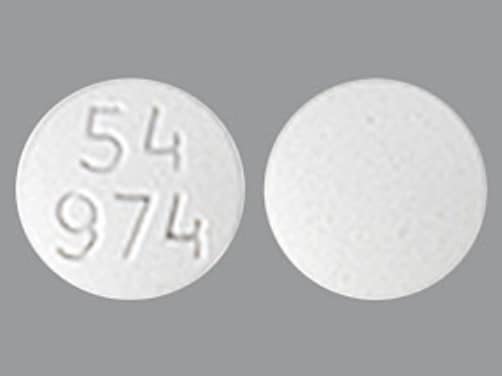
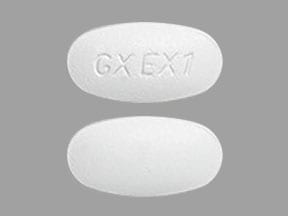
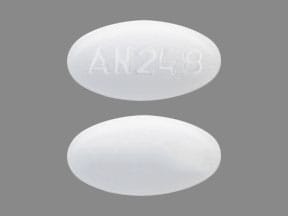
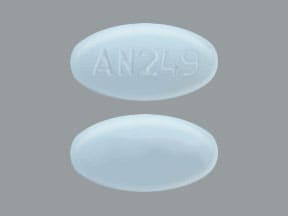
Tablet, Oral:
Lotronex: 0.5 mg, 1 mg
Generic: 0.5 mg, 1 mg
Pharmacology
Mechanism of Action
Alosetron is a potent and selective antagonist of a subtype of the serotonin 5-HT3 receptor. 5-HT3 receptors are ligand-gated ion channels extensively distributed on enteric neurons in the human gastrointestinal tract, as well as other peripheral and central locations. Activation of these channels affect the regulation of visceral pain, colonic transit, and gastrointestinal secretions. In patients with irritable bowel syndrome, blockade of these channels may reduce pain, abdominal discomfort, urgency, and diarrhea.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
Vd: 65 to 95 L
Metabolism
Extensive hepatic metabolism via CYP2C9, 3A4, and 1A2. Thirteen metabolites have been detected in the urine. Biological activity of these metabolites in unknown.
Excretion
Urine (74%, 13% of total dose as unchanged drug); feces (11%, 1% of total dose as unchanged drug)
Time to Peak
1 hour
Half-Life Elimination
1.5 hours
Protein Binding
82%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Exposure to alosetron is increased.
Special Populations: Elderly
Plasma levels are elevated by about 40% in patients 65 years and older.
Special Populations: Gender
Plasma concentrations are 30% to 50% lower and less variable in men.
Use: Labeled Indications
Irritable bowel syndrome: Treatment of women with severe diarrhea-predominant irritable bowel syndrome (IBS) who have chronic IBS symptoms (generally lasting 6 months or longer), have had anatomic or biochemical abnormalities of the GI tract excluded, and who have not responded adequately to conventional therapy.
Contraindications
Do not initiate in patients with constipation. History of chronic or severe constipation or sequelae from constipation; history of ischemic colitis, intestinal obstruction, stricture, toxic megacolon, GI perforation, adhesions, diverticulitis, Crohn disease, ulcerative colitis, history of severe hepatic impairment; history of impaired intestinal circulation, thrombophlebitis, or hypercoagulable state; coadministration with fluvoxamine.
Dosage and Administration
Dosing: Adult
Irritable bowel syndrome (IBS): Females: Oral: Initial: 0.5 mg twice daily for 4 week; if tolerated, but response is inadequate, may be increased after 4 weeks to 1 mg twice daily (maximum dose: 2 mg/day). If response is inadequate after 4 weeks of 1 mg twice-daily dosing, discontinue treatment.
Dosing: Geriatric
Refer to adult dosing. Dosage adjustment is not required; however, postmarketing experience suggests that elderly patients may be at greater risk for complications of constipation.
Dosing: Adjustment for Toxicity
Constipation: Patients experiencing constipation with 0.5 mg twice daily should discontinue therapy until constipation resolves. Therapy may be reinitiated at 0.5 mg once daily. Discontinue immediately if constipation recurs at lower dose.
Ischemic colitis: Discontinue therapy immediately; do not restart
Administration
May be administered with or without food.
Storage
Store at 20°C to 25°C (68°F to 77°F). Protect from light and moisture.
Alosetron Images
Drug Interactions
Apomorphine: Antiemetics (5HT3 Antagonists) may enhance the hypotensive effect of Apomorphine. Avoid combination
CYP1A2 Inhibitors (Moderate): May increase the serum concentration of Alosetron. Management: Avoid concomitant use of alosetron and moderate CYP1A2 inhibitors whenever possible. If combined use is necessary, monitor for increased alosetron effects/toxicities. Consider therapy modification
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Alosetron. Monitor therapy
Eluxadoline: Alosetron may enhance the constipating effect of Eluxadoline. Avoid combination
FluvoxaMINE: May decrease the metabolism of Alosetron. Avoid combination
Serotonergic Agents (High Risk): Alosetron may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: FluvoxaMINE; TraMADol. Monitor therapy
Tapentadol: Antiemetics (5HT3 Antagonists) may diminish the analgesic effect of Tapentadol. Monitor therapy
Tobacco (Smoked): May decrease the serum concentration of Alosetron. Monitor therapy
TraMADol: Antiemetics (5HT3 Antagonists) may enhance the serotonergic effect of TraMADol. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Adverse Reactions
>10%: Gastrointestinal: Constipation (9% to 29%; dose related)
1% to 10%:
Central nervous system: Fatigue (≥3%), headache (≥3%)
Gastrointestinal: Abdominal distress (≤1% to 7%), abdominal pain (≤1% to 7%), nausea (6%), gastrointestinal distress (≤5%), gastrointestinal pain (≤5%), gastroenteritis (≥3%), vomiting (≥3%), diarrhea (2% to 3%), flatulence (1% to 3%), hemorrhoids (1% to 3%), abdominal distention (2%), acid regurgitation (≤2%), gastroesophageal reflux disease (≤2%)
Genitourinary: Urinary tract infection (≥3%)
Neuromuscular & skeletal: Muscle spasm (≥3%)
Respiratory: Cough (≥3%), nasopharyngitis (≥3%), upper respiratory tract infection (≥3%)
<1%, postmarketing, and/or case reports: Abnormal bilirubin levels, abnormal erythrocytes, active gastrointestinal lesion, allergic skin reaction, alopecia, anxiety, cardiac arrhythmia, cholecystitis, cognitive dysfunction, colitis, confusion, cystitis, decreased gastrointestinal motility, depression, dermatitis, diaphoresis, disruption of body temperature regulation, disturbance in fluid balance, diverticulitis, drowsiness, dyspepsia, extrasystoles, fecal impaction, gastrointestinal obstruction, gastrointestinal perforation, gastrointestinal spasm, gastrointestinal ulcer, hematoma, hemoglobinopathy, hemorrhage, hepatitis, hyperacidity, hyperglycemia, hypertension, hypoesthesia, hypoglycemia, hypothalamic disease, intestinal obstruction, intussusception, ischemic colitis, memory impairment, mesenteric ischemia (small bowel), muscle cramps, muscle rigidity, myalgia, occult blood in stools, ostealgia, pain, pituitary insufficiency, proctitis, respiratory tract disease, sedation, sexual disorder, skeletal pain, skin rash, tachyarrhythmia, tremor, ulcerative colitis, urinary frequency, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Constipation: [US Boxed Warning]: Discontinue immediately in patients who develop constipation; infrequent but serious complications of constipation, have resulted in hospitalization, and rarely, blood transfusion, surgery, or death have been reported (obstruction, ileus, perforation [rare], impaction, toxic megacolon, secondary bowel ischemia). Constipation is a frequent, dose-related side effect; risk for complications from constipation may be increased in elderly, debilitated patients, or with concurrent use of other medications which decrease GI motility. Nonsevere constipation may be managed by temporarily interrupting therapy and decreasing the dose. Do not initiate in patients with constipation.
- Ischemic colitis: [US Boxed Warning]: Ischemic colitis has been reported during treatment without warning. Discontinue and evaluate immediately in patients who experience rectal bleeding, bloody diarrhea, or a sudden worsening of abdominal pain, and do not restart therapy if ischemic colitis is diagnosed.
Disease-related concerns:
- Hepatic impairment: Use caution in mild to moderate hepatic impairment (Child-Pugh class A or B) (extensively metabolized); contraindicated in severe impairment (Child-Pugh class C).
Special populations:
- Debilitated patients: Use with caution in debilitated patients due to increased risk of complications from constipation.
- Elderly: Use with caution in the elderly due to increased risk of complications from constipation.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate use: [US Boxed Warning]: Only indicated for women with severe diarrhea-predominant irritable bowel syndrome who have not responded adequately to conventional therapy who have chronic IBS symptoms (lasting ≥6 months) and are without anatomic or biochemical abnormalities of the GI tract. Severe diarrhea-predominant IBS includes at least one of the following: frequent and severe abdominal pain/discomfort, frequent bowel urgency or fecal incontinence, and disability or restriction of daily activities due to IBS.
Pregnancy
Pregnancy Considerations
Adverse events have not been observed in animal reproduction studies.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience abdominal pain and nausea. Have patient report immediately to prescriber signs of gastrointestinal problems (constipation, new or severe abdominal pain, or blood in stools), bloating, mood changes, rectal bleeding, rectal pain, vomiting, or fast heartbeat (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for healthcare professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience and judgment in diagnosing, treating and advising patients.