Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
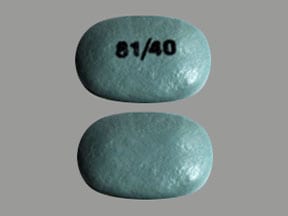
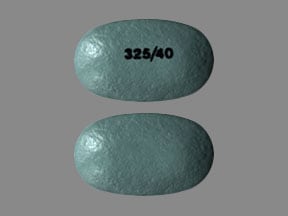
Tablet Delayed Release, Oral:
Yosprala: Aspirin 81 mg and omeprazole 40 mg, Aspirin 325 mg and omeprazole 40 mg [contains corn starch, fd&c blue #2 (indigotine)]
Generic: Aspirin 325 mg and omeprazole 40 mg, Aspirin 81 mg and omeprazole 40 mg
Pharmacology
Mechanism of Action
Aspirin: Irreversibly inhibits cyclooxygenase-1 and 2 (COX-1 and 2) enzymes, via acetylation, which results in decreased formation of prostaglandin precursors; irreversibly inhibits formation of prostaglandin derivative, thromboxane A2, via acetylation of platelet cyclooxygenase, thus inhibiting platelet aggregation; has antipyretic, analgesic, and anti-inflammatory properties.
Omeprazole: Suppresses gastric basal and stimulated acid secretion by inhibiting the parietal cell H+/K+ ATP pump
Use: Labeled Indications
Secondary prevention of cardiovascular and cerebrovascular events: Reduction of the risk of aspirin-associated gastric ulcers in patients at risk of developing gastric ulcers due to age (≥55 years) or documented history of gastric ulcers who require aspirin for the secondary prevention of cardiovascular and cerebrovascular events.
Limitations of use: Not for use as the initial dose of aspirin therapy during onset of acute coronary syndrome, acute myocardial infarction or before percutaneous coronary intervention; has not been shown to reduce the risk of gastrointestinal bleeding due to aspirin.
Contraindications
Hypersensitivity to aspirin, other nonsteroidal anti-inflammatory drugs (NSAIDs), omeprazole, other substituted benzimidazole proton pump inhibitors, or to any component of the formulation; history of asthma, urticaria, rhinitis, and nasal polyps or other allergic-type reactions after taking aspirin or other NSAIDs; pediatric patients with suspected viral infections, with or without fever; concurrent use with rilpivirine-containing products.
Documentation of allergenic cross-reactivity for salicylates is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Secondary prevention of cardiovascular and cerebrovascular events: Oral: One tablet (aspirin 81 mg/omeprazole 40 mg or aspirin 325 mg/omeprazole 40 mg) once daily. Note: Generally 81 mg of aspirin has been accepted as an effective dose for secondary cardiovascular prevention; refer to current clinical practice guidelines when considering the need for 325 mg of aspirin.
Dosing: Geriatric
Refer to adult dosing.
Administration
Administer at least 1 hour before a meal. Swallow tablet whole with liquid; do not split, chew, crush, or dissolve.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Store in original container. Protect from moisture.
Aspirin and Omeprazole Images
Drug Interactions
Acalabrutinib: Proton Pump Inhibitors may decrease the serum concentration of Acalabrutinib. Avoid combination
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the antiplatelet effect of other Agents with Antiplatelet Properties. Monitor therapy
Ajmaline: Salicylates may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Alcohol (Ethyl): May enhance the adverse/toxic effect of Aspirin. Specifically, alcohol may increase the bleeding risk of aspirin. Alcohol (Ethyl) may diminish the therapeutic effect of Aspirin. Specifically, alcohol may interfere with the controlled release mechanism of extended release aspirin. Management: Monitor patients who drink 3 or more alcoholic drinks a day for increased bleeding while taking aspirin. Counsel patients about the risk of bleeding and discourage such consumption. Give extended release aspirin 2 hours before, or 1 hour after, alcohol. Consider therapy modification
Alendronate: Aspirin may enhance the adverse/toxic effect of Alendronate. Specifically, the incidence of upper gastrointestinal adverse events may be increased Monitor therapy
Ammonium Chloride: May increase the serum concentration of Salicylates. Monitor therapy
Amphetamine: Proton Pump Inhibitors may increase the absorption of Amphetamine. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Salicylates may enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Salicylates may diminish the therapeutic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Anticoagulants: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Anticoagulants. Exceptions: Bemiparin; Enoxaparin; Heparin. Monitor therapy
Anticoagulants: Salicylates may enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Antihepaciviral Combination Products: May decrease the serum concentration of Omeprazole. Monitor therapy
Apixaban: Aspirin may enhance the adverse/toxic effect of Apixaban. Specifically, the risk for bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely. Consider therapy modification
Atazanavir: Proton Pump Inhibitors may decrease the serum concentration of Atazanavir. Management: See full drug interaction monograph for details. Consider therapy modification
Bemiparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin with antiplatelet agents. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Benzbromarone: Salicylates may diminish the therapeutic effect of Benzbromarone. Monitor therapy
Bisphosphonate Derivatives: Proton Pump Inhibitors may diminish the therapeutic effect of Bisphosphonate Derivatives. Monitor therapy
Blood Glucose Lowering Agents: Salicylates may enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Bosutinib: Proton Pump Inhibitors may decrease the serum concentration of Bosutinib. Management: Consider alternatives to proton pump inhibitors, such as short-acting antacids or histamine-2 receptor antagonists. Administer alternative agents more than 2 hours before or after bosutinib. Consider therapy modification
Calcium Channel Blockers (Nondihydropyridine): May enhance the antiplatelet effect of Aspirin. Monitor therapy
Capecitabine: Proton Pump Inhibitors may diminish the therapeutic effect of Capecitabine. Monitor therapy
Carbonic Anhydrase Inhibitors: Salicylates may enhance the adverse/toxic effect of Carbonic Anhydrase Inhibitors. Salicylate toxicity might be enhanced by this same combination. Management: Avoid these combinations when possible.Dichlorphenamide use with high-dose aspirin as contraindicated. If another combination is used, monitor patients closely for adverse effects. Tachypnea, anorexia, lethargy, and coma have been reported. Exceptions: Brinzolamide; Dorzolamide. Consider therapy modification
Carisoprodol: Aspirin may increase serum concentrations of the active metabolite(s) of Carisoprodol. Specifically, Meprobamate concentrations may be increased. Aspirin may decrease the serum concentration of Carisoprodol. Monitor therapy
Cefditoren: Proton Pump Inhibitors may decrease the serum concentration of Cefditoren. Management: If possible, avoid use of cefditoren with proton pump inhibitors (PPIs). Consider alternative methods to minimize/control acid reflux (eg, diet modification) or alternative antimicrobial therapy if use of PPIs can not be avoided. Consider therapy modification
Cefpodoxime: Proton Pump Inhibitors may decrease the serum concentration of Cefpodoxime. Monitor therapy
Cefuroxime: Proton Pump Inhibitors may decrease the absorption of Cefuroxime. Avoid combination
Cephalothin: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Cephalothin. Specifically, the risk for bleeding may be increased. Monitor therapy
Cilostazol: Omeprazole may increase serum concentrations of the active metabolite(s) of Cilostazol. Omeprazole may increase the serum concentration of Cilostazol. Management: Reduce the cilostazol dose to 50 mg twice daily in patients who are also receiving omeprazole. Monitor clinical response to cilostazol closely. Consider therapy modification
Citalopram: Omeprazole may increase the serum concentration of Citalopram. Management: Limit citalopram dose to a maximum of 20 mg/day if used with omeprazole. Consider therapy modification
CloBAZam: Omeprazole may increase serum concentrations of the active metabolite(s) of CloBAZam. Monitor therapy
Clopidogrel: Omeprazole may diminish the antiplatelet effect of Clopidogrel. Omeprazole may decrease serum concentrations of the active metabolite(s) of Clopidogrel. Management: Clopidogrel labeling recommends avoiding concurrent omeprazole due to a possible decrease in clopidogrel effectiveness. Rabeprazole or pantoprazole may be lower-risk alternatives to omeprazole. Consider therapy modification
CloZAPine: Omeprazole may decrease the serum concentration of CloZAPine. Omeprazole may increase the serum concentration of CloZAPine. Monitor therapy
Collagenase (Systemic): Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
Corticosteroids (Systemic): Salicylates may enhance the adverse/toxic effect of Corticosteroids (Systemic). These specifically include gastrointestinal ulceration and bleeding. Corticosteroids (Systemic) may decrease the serum concentration of Salicylates. Withdrawal of corticosteroids may result in salicylate toxicity. Monitor therapy
CycloSPORINE (Systemic): Omeprazole may increase the serum concentration of CycloSPORINE (Systemic). Monitor therapy
CYP2C19 Inducers (Moderate): May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
CYP2C19 Inducers (Strong): May increase the metabolism of CYP2C19 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
Cysteamine (Systemic): Proton Pump Inhibitors may diminish the therapeutic effect of Cysteamine (Systemic). Monitor therapy
Dabigatran Etexilate: Aspirin may enhance the adverse/toxic effect of Dabigatran Etexilate. Specifically, the risk for bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling states that low dose aspirin could be considered, but the use of antiplatelets are not recommended for stroke prevention in patients with atrial fibrillation. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C19 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dacomitinib: Proton Pump Inhibitors may decrease the serum concentration of Dacomitinib. Management: Avoid concurrent use of dacomitinib with proton pump inhibitors. Antacids may be used. Histamine H2-receptor antagonists (HR2A) may be used if dacomitinib is given at least 6 hours before or 10 hours after the H2RA. Avoid combination
Darunavir: May decrease the serum concentration of Omeprazole. Monitor therapy
Dasatinib: Proton Pump Inhibitors may decrease the serum concentration of Dasatinib. Management: Antacids (taken 2 hours before or after dasatinib administration) can be used in place of the proton pump inhibitor if some acid-reducing therapy is needed. Avoid combination
Delavirdine: Proton Pump Inhibitors may decrease the serum concentration of Delavirdine. Management: Chronic therapy with proton pump inhibitors (PPIs) should be avoided in patients treated with delavirdine. The clinical significance of short-term PPI therapy with delavirdine is uncertain, but such therapy should be undertaken with caution. Avoid combination
Deoxycholic Acid: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Dexibuprofen: Aspirin may enhance the adverse/toxic effect of Dexibuprofen. Dexibuprofen may diminish the cardioprotective effect of Aspirin. Avoid combination
Dexketoprofen: Salicylates may enhance the adverse/toxic effect of Dexketoprofen. Dexketoprofen may diminish the therapeutic effect of Salicylates. Salicylates may decrease the serum concentration of Dexketoprofen. Management: The use of high-dose salicylates (3 g/day or more in adults) together with dexketoprofen is inadvisable. Consider administering dexketoprofen 30-120 min after or at least 8 hrs before cardioprotective doses of aspirin to minimize any possible interaction. Avoid combination
Dexmethylphenidate: Proton Pump Inhibitors may increase the absorption of Dexmethylphenidate. Specifically, proton pump inhibitors may interfere with the normal release of drug from the extended-release capsules (Focalin XR brand), which could result in both increased absorption (early) and decreased delayed absorption. Monitor therapy
Dextroamphetamine: Proton Pump Inhibitors may increase the absorption of Dextroamphetamine. Specifically, the dextroamphetamine absorption rate from mixed amphetamine salt extended release (XR) capsules may be increased in the first hours after dosing. Monitor therapy
Doxycycline: Proton Pump Inhibitors may decrease the bioavailability of Doxycycline. Monitor therapy
Edoxaban: Aspirin may enhance the adverse/toxic effect of Edoxaban. Specifically, the risk of bleeding may be increased. Aspirin may increase the serum concentration of Edoxaban. Management: Carefully consider the anticipated risks and benefits of this combination. If combined, increased monitoring for bleeding is recommended. Consider therapy modification
Elagolix: May increase the serum concentration of Omeprazole. Management: No action required for omeprazole doses of 40 mg daily or lower. If elagolix is used concomitantly with omeprazole doses higher than 40 mg daily, consider reducing the dose of omeprazole. Consider therapy modification
Enoxaparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue antiplatelet agents prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Conversely, concentrations of active metabolites may be increased for those drugs activated by CYP2C19. Management: Concurrent use of enzalutamide with CYP2C19 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C19 substrate should be performed with caution and close monitoring. Consider therapy modification
Erlotinib: Proton Pump Inhibitors may decrease the serum concentration of Erlotinib. Avoid combination
Escitalopram: Omeprazole may increase the serum concentration of Escitalopram. Management: Monitor for increased escitalopram toxicity with concomitant use of omeprazole. Recommendations for management of this interaction found in product labeling may differ by country. Consult appropriate labeling. Consider therapy modification
Fat Emulsion (Fish Oil Based): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Felbinac: May enhance the adverse/toxic effect of Aspirin. Monitor therapy
Floctafenine: May enhance the adverse/toxic effect of Aspirin. An increased risk of bleeding may be associated with use of this combination. Floctafenine may diminish the cardioprotective effect of Aspirin. Avoid combination
Fluconazole: May increase the serum concentration of Proton Pump Inhibitors. Monitor therapy
Fosphenytoin: Omeprazole may increase the serum concentration of Fosphenytoin. Fosphenytoin may decrease the serum concentration of Omeprazole. Monitor therapy
Gefitinib: Proton Pump Inhibitors may decrease the serum concentration of Gefitinib. Management: Avoid use of proton pump inhibitors (PPIs) with gefitinib when possible. If required, administer gefitinib 12 hours after administration of the PPI or 12 hours before the next dose of the PPI. Consider therapy modification
Ginkgo Biloba: May enhance the anticoagulant effect of Salicylates. Management: Consider alternatives to this combination of agents. Monitor for signs and symptoms of bleeding (especially intracranial bleeding) if salicylates are used in combination with ginkgo biloba. Consider therapy modification
Glucosamine: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Gold Sodium Thiomalate: Aspirin may enhance the adverse/toxic effect of Gold Sodium Thiomalate. Specifically, liver function tests may be elevated when these agents are combined. Monitor therapy
Heparin: Aspirin may enhance the anticoagulant effect of Heparin. Monitor therapy
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Bleeding may occur. Management: Avoid combination when possible. If used, monitor more closely for evidence of bleeding. Discontinue herbal products with anticoagulant or antiplatelet actions 2 weeks prior to surgical, dental, or invasive procedures. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Salicylates. Bleeding may occur. Consider therapy modification
Hyaluronidase: Salicylates may diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving salicylates (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. Consider therapy modification
Ibritumomab Tiuxetan: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to impaired platelet function and an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Indinavir: Proton Pump Inhibitors may decrease the serum concentration of Indinavir. Monitor therapy
Influenza Virus Vaccine (Live/Attenuated): May enhance the adverse/toxic effect of Salicylates. Specifically, Reye's syndrome may develop. Avoid combination
Inotersen: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Iron Preparations: Proton Pump Inhibitors may decrease the absorption of Iron Preparations. Exceptions: Ferric Carboxymaltose; Ferric Citrate; Ferric Derisomaltose; Ferric Gluconate; Ferric Hydroxide Polymaltose Complex; Ferric Pyrophosphate Citrate; Ferumoxytol; Iron Dextran Complex; Iron Sucrose. Monitor therapy
Itraconazole: Proton Pump Inhibitors may increase the serum concentration of Itraconazole. Proton Pump Inhibitors may decrease the serum concentration of Itraconazole. Management: Exposure to Tolsura brand itraconazole may be increased by PPIs; consider itraconazole dose reduction. Exposure to Sporanox brand itraconazole capsules may be decreased by PPIs. Give Sporanox brand itraconazole at least 2 hrs before or 2 hrs after PPIs Consider therapy modification
Ketoconazole (Systemic): Proton Pump Inhibitors may decrease the absorption of Ketoconazole (Systemic). Ketoconazole (Systemic) may increase the serum concentration of Proton Pump Inhibitors. Management: Administer ketoconazole with an acidic beverage, such as non-diet cola, to increase gastric acidity and improve absorption if concomitant use with proton pump inhibitors is necessary. Consider therapy modification
Ketorolac (Nasal): May enhance the adverse/toxic effect of Aspirin. An increased risk of bleeding may be associated with use of this combination. Ketorolac (Nasal) may diminish the cardioprotective effect of Aspirin. Avoid combination
Ketorolac (Systemic): May enhance the adverse/toxic effect of Aspirin. An increased risk of bleeding may be associated with use of this combination. Ketorolac (Systemic) may diminish the cardioprotective effect of Aspirin. Avoid combination
Ledipasvir: Proton Pump Inhibitors may decrease the serum concentration of Ledipasvir. Management: PPI doses equivalent to omeprazole 20 mg or lower may be given with ledipasvir under fasted conditions. Administration with higher doses of PPIs, 2 hours after a PPI, or in combination with food and PPIs may reduce ledipasvir bioavailability. Consider therapy modification
Lesinurad: Aspirin may diminish the therapeutic effect of Lesinurad. Monitor therapy
Limaprost: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Loop Diuretics: Salicylates may diminish the diuretic effect of Loop Diuretics. Loop Diuretics may increase the serum concentration of Salicylates. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of Proton Pump Inhibitors. Monitor therapy
Macimorelin: Aspirin may diminish the diagnostic effect of Macimorelin. Avoid combination
Mesalamine: Proton Pump Inhibitors may diminish the therapeutic effect of Mesalamine. Proton pump inhibitor-mediated increases in gastrointestinal pH may cause the premature release of mesalamine from specific sustained-release mesalamine products. Management: Consider avoiding concurrent administration of high-dose proton pump inhibitors (PPIs) with sustained-release mesalamine products. Consider therapy modification
Methotrexate: Salicylates may increase the serum concentration of Methotrexate. Salicylate doses used for prophylaxis of cardiovascular events are not likely to be of concern. Consider therapy modification
Methylphenidate: Proton Pump Inhibitors may increase the absorption of Methylphenidate. Specifically, proton pump inhibitors may interfere with the normal release of drug from the extended-release capsules (Ritalin LA brand), which could result in both increased absorption (early) and decreased delayed absorption. Monitor therapy
Multivitamins/Fluoride (with ADE): May enhance the antiplatelet effect of Aspirin. Aspirin may decrease the serum concentration of Multivitamins/Fluoride (with ADE). Specifically, aspirin may decrease the absorption of ascorbic acid. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the antiplatelet effect of Aspirin. Aspirin may decrease the serum concentration of Multivitamins/Minerals (with ADEK, Folate, Iron). Specifically, aspirin may decrease absorption of ascorbic acid. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the antiplatelet effect of Aspirin. Aspirin may decrease the serum concentration of Multivitamins/Minerals (with AE, No Iron). Specifically, aspirin may decrease the absorption of ascorbic acid. Monitor therapy
Mycophenolate: Proton Pump Inhibitors may decrease the serum concentration of Mycophenolate. Specifically, concentrations of the active mycophenolic acid may be reduced. Monitor therapy
Nalmefene: Omeprazole may decrease the serum concentration of Nalmefene. Monitor therapy
Nelfinavir: Proton Pump Inhibitors may decrease serum concentrations of the active metabolite(s) of Nelfinavir. Proton Pump Inhibitors may decrease the serum concentration of Nelfinavir. Avoid combination
Neratinib: Proton Pump Inhibitors may decrease the serum concentration of Neratinib. Specifically, proton pump inhibitors may reduce neratinib absorption. Avoid combination
Nicorandil: Aspirin may enhance the adverse/toxic effect of Nicorandil. Specifically, the risk of gastrointestinal ulceration and hemorrhage may be increased. Monitor therapy
Nilotinib: Proton Pump Inhibitors may decrease the serum concentration of Nilotinib. Management: Avoid this combination when possible since separation of doses is not likely to be an adequate method of minimizing the interaction. Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): Aspirin may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Management: Concurrent use of aspirin at doses beyond cardioprotective levels is not recommended. While concurrent use of low-dose aspirin with a COX-2 inhibitor is permissable, patients should be monitored closely for signs/symptoms of GI ulceration/bleeding. Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents (Nonselective): May enhance the adverse/toxic effect of Salicylates. An increased risk of bleeding may be associated with use of this combination. Nonsteroidal Anti-Inflammatory Agents (Nonselective) may diminish the cardioprotective effect of Salicylates. Salicylates may decrease the serum concentration of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Consider therapy modification
Obinutuzumab: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Omacetaxine: Aspirin may enhance the adverse/toxic effect of Omacetaxine. Specifically, the risk for bleeding-related events may be increased. Management: Avoid concurrent use of aspirin with omacetaxine in patients with a platelet count of less than 50,000/uL. Avoid combination
Omega-3 Fatty Acids: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
PAZOPanib: Proton Pump Inhibitors may decrease the serum concentration of PAZOPanib. Avoid combination
Pentosan Polysulfate Sodium: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Specifically, the risk of bleeding may be increased by concurrent use of these agents. Monitor therapy
Pentoxifylline: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Pexidartinib: Proton Pump Inhibitors may decrease the serum concentration of Pexidartinib. Management: If acid-reduction is needed, consider administering an antacid 2 hours before or after pexidartinib, or administer pexidartinib 2 hours before or 10 hours after an H2 receptor antagonist. Avoid combination
Phenytoin: May decrease the serum concentration of Omeprazole. Omeprazole may increase the serum concentration of Phenytoin. Monitor therapy
Posaconazole: Proton Pump Inhibitors may decrease the serum concentration of Posaconazole. Consider therapy modification
Potassium Phosphate: May increase the serum concentration of Salicylates. Monitor therapy
PRALAtrexate: Salicylates may increase the serum concentration of PRALAtrexate. Salicylate doses used for prophylaxis of cardiovascular events are unlikely to be of concern. Consider therapy modification
Probenecid: Salicylates may diminish the therapeutic effect of Probenecid. Monitor therapy
Prostacyclin Analogues: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Raltegravir: Proton Pump Inhibitors may increase the serum concentration of Raltegravir. Monitor therapy
RifAMPin: May decrease the serum concentration of Omeprazole. Avoid combination
Rilpivirine: Proton Pump Inhibitors may decrease the serum concentration of Rilpivirine. Avoid combination
Riociguat: Proton Pump Inhibitors may decrease the serum concentration of Riociguat. Monitor therapy
Risedronate: Proton Pump Inhibitors may diminish the therapeutic effect of Risedronate. Proton Pump Inhibitors may increase the serum concentration of Risedronate. This applies specifically to use of delayed-release risedronate. Consider therapy modification
Rivaroxaban: Aspirin may enhance the adverse/toxic effect of Rivaroxaban. Specifically, the risk of bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely. Consider therapy modification
Salicylates: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Salicylates: May enhance the anticoagulant effect of other Salicylates. Monitor therapy
Saquinavir: Proton Pump Inhibitors may increase the serum concentration of Saquinavir. Monitor therapy
Secretin: Proton Pump Inhibitors may diminish the diagnostic effect of Secretin. Specifically, use of PPIs may cause a hyperresponse in gastrin secretion in response to secretin stimulation testing, falsely suggesting gastrinoma. Management: Avoid concomitant use of proton pump inhibitors (PPIs) and secretin, and discontinue PPIs several weeks prior to secretin administration, with the duration of separation determined by the specific PPI. See full monograph for details. Consider therapy modification
Selective Serotonin Reuptake Inhibitors: May enhance the antiplatelet effect of Aspirin. Monitor therapy
Serotonin/Norepinephrine Reuptake Inhibitors: May enhance the antiplatelet effect of Aspirin. Monitor therapy
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
SORAfenib: Proton Pump Inhibitors may decrease the absorption of SORAfenib. Monitor therapy
Spironolactone: Aspirin may diminish the therapeutic effect of Spironolactone. Monitor therapy
St John's Wort: May decrease the serum concentration of Omeprazole. Avoid combination
Sucroferric Oxyhydroxide: May decrease the serum concentration of Aspirin. Management: Administer aspirin at least 1 hour before administration of sucroferric oxyhydroxide. Consider therapy modification
Sulfinpyrazone: Salicylates may decrease the serum concentration of Sulfinpyrazone. Avoid combination
Tacrolimus (Systemic): Proton Pump Inhibitors may increase the serum concentration of Tacrolimus (Systemic). Management: Tacrolimus dose adjustment may be required. Rabeprazole, pantoprazole, or selected H2-receptor antagonists (i.e., ranitidine or famotidine) may be less likely to interact. Genetic testing may predict patients at highest risk. Consider therapy modification
Talniflumate: Aspirin may enhance the adverse/toxic effect of Talniflumate. Management: When possible, consider alternatives to this combination. Concurrent use is generally not recommended. Consider therapy modification
Thiopental: Aspirin may decrease the protein binding of Thiopental. Monitor therapy
Thrombolytic Agents: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Thrombolytic Agents. Monitor therapy
Thrombolytic Agents: Salicylates may enhance the adverse/toxic effect of Thrombolytic Agents. An increased risk of bleeding may occur. Monitor therapy
Ticagrelor: Aspirin may enhance the antiplatelet effect of Ticagrelor. Aspirin may diminish the therapeutic effect of Ticagrelor. More specifically, the benefits of ticagrelor relative to clopidogrel may be diminished in adult patients receiving daily aspirin doses greater than 100-150 mg daily. Management: Avoid daily aspirin doses greater than 100 mg in adults receiving ticagrelor. Canadian recommendations are to avoid adult daily aspirin doses greater than 150 mg. Daily low-dose aspirin (U.S.: 75-100 mg; Canada: 75-150 mg) is recommended. Consider therapy modification
Tiludronate: Aspirin may decrease the serum concentration of Tiludronate. Monitor therapy
Tipranavir: May decrease the serum concentration of Proton Pump Inhibitors. These data are derived from studies with Ritonavir-boosted Tipranavir. Monitor therapy
Tipranavir: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Tricyclic Antidepressants (Tertiary Amine): May enhance the antiplatelet effect of Aspirin. Monitor therapy
Urokinase: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Urokinase. Avoid combination
Valproate Products: Salicylates may increase the serum concentration of Valproate Products. Monitor therapy
Varicella Virus-Containing Vaccines: Salicylates may enhance the adverse/toxic effect of Varicella Virus-Containing Vaccines. Specifically, the risk for Reye's syndrome may increase. Avoid combination
Velpatasvir: Proton Pump Inhibitors may decrease the serum concentration of Velpatasvir. Avoid combination
Vitamin E (Systemic): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Salicylates may enhance the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Voriconazole: Omeprazole may increase the serum concentration of Voriconazole. Voriconazole may increase the serum concentration of Omeprazole. Monitor therapy
Zanubrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Adverse Reactions
Also see individual agents.
>10%: Gastrointestinal: Gastritis (18%)
1% to 10%:
Central nervous system: Noncardiac chest pain (2%)
Gastrointestinal: Diarrhea (3%), nausea (3%), gastric polyp (2%)
<1%, postmarketing, and/or case reports: Gastrointestinal hemorrhage (including hematochezia and large intestinal hemorrhage), intestinal obstruction (small bowel), upper gastrointestinal hemorrhage (gastric or duodenal)
Warnings/Precautions
Concerns related to adverse effects:
- Atrophic gastritis: Long-term omeprazole therapy has caused atrophic gastritis (identified by biopsy).
- Carcinoma: In long-term (2-year) studies in rats, omeprazole produced a dose-related increase in gastric carcinoid tumors. While available endoscopic evaluations and histologic examinations of biopsy specimens from human stomachs have not detected a risk from short-term exposure to omeprazole, further human data on the effect of sustained hypochlorhydria and hypergastrinemia are needed to rule out the possibility of an increased risk for the development of tumors in humans receiving long-term therapy.
- Clostridioides (formerly Clostridium) difficile-associated diarrhea: Use of proton pump inhibitors (PPIs) may increase risk of Clostridioides (formerly Clostridium) difficile-associated diarrhea (CDAD), especially in hospitalized patients; consider CDAD diagnosis in patients with persistent diarrhea that does not improve. Use the lowest dose and shortest duration of PPI therapy appropriate for the condition being treated.
- Cutaneous and systemic lupus erythematosus: Has been reported as new onset or exacerbation of existing autoimmune disease; most cases were cutaneous lupus erythematosus (CLE), most commonly, subacute CLE (occurring within weeks to years after continuous therapy). Systemic lupus erythematosus (SLE) is less common (typically occurs within days to years after initiating treatment) and occurred primarily in young adults up to the elderly. Discontinue therapy if signs or symptoms of CLE or SLE occur and refer to specialist for evaluation; most patients improve 4 to 12 weeks after discontinuation of omeprazole.
- Fractures: Increased incidence of osteoporosis-related bone fractures of the hip, spine, or wrist may occur with PPI therapy. Patients on high-dose (multiple daily doses) or long-term (≥1 year) therapy should be monitored. Use the lowest effective dose for the shortest duration of time, use vitamin D and calcium supplementation, and follow appropriate guidelines to reduce risk of fractures in patients at risk.
- Fundic gland polyps: Use of PPIs increases risk of fundic gland polyps, especially with long-term use (>1 year). May occur without symptoms, but nausea, vomiting, or abdominal pain may occur; GI bleeding and/or anemia may occur with ulcerated polyps. Diagnosis of polyps may also increase risk for small intestinal blockage. Use the lowest dose and shortest duration of PPI therapy appropriate for the condition being treated.
- GI effects: Aspirin may cause serious GI adverse reactions, including inflammation, bleeding ulceration and perforation. Other adverse reactions include stomach pain, heartburn, nausea, and vomiting. Monitor patients for signs of ulceration and bleeding. Discontinue therapy if active and significant bleeding occurs. Use aspirin with caution in patients with erosive gastritis; avoid use in patients with active peptic ulcer disease.
- Hypomagnesemia: Reported rarely, usually with prolonged PPI use of >3 months (most cases >1 year of therapy). May be symptomatic or asymptomatic; severe cases may cause tetany, seizures, and cardiac arrhythmias. Consider obtaining serum magnesium concentrations prior to beginning long-term therapy, especially if taking concomitant digoxin, diuretics, or other drugs known to cause hypomagnesemia; and periodically thereafter. Hypomagnesemia may be corrected by magnesium supplementation, although discontinuation of omeprazole may be necessary; magnesium levels typically return to normal within 1 week of stopping.
- Interstitial nephritis: Acute interstitial nephritis has been observed in patients taking PPIs; may occur at any time during therapy and is generally due to an idiopathic hypersensitivity reaction. Discontinue if acute interstitial nephritis develops.
- Salicylate sensitivity: Patients with sensitivity to tartrazine dyes, nasal polyps, and asthma may have an increased risk of salicylate sensitivity.
- Tinnitus: Discontinue use if tinnitus or impaired hearing occurs.
- Upper gastrointestinal events (eg, symptomatic or complicated ulcers): Low-dose aspirin for cardioprotective effects is associated with a two- to fourfold increase in upper gastrointestinal (UGI) events. The risks of these events increase with increasing aspirin dose; during the chronic phase of aspirin dosing, doses >81 mg are not recommended unless indicated (Bhatt 2008).
- Vitamin B12 deficiency: Prolonged treatment (>3 years) of PPIs may lead to vitamin B12 malabsorption and subsequent vitamin B12 deficiency. The magnitude of the deficiency is dose-related and the association is stronger in females and those younger in age (<30 years); prevalence is decreased after discontinuation of therapy (Lam 2013).
Disease-related concerns:
- Bleeding disorders: Use aspirin with caution in patients with platelet and bleeding disorders.
- Dehydration: Use aspirin with caution in patients with dehydration.
- Gastric malignancy: Relief of gastric symptoms does not preclude the presence of a gastric malignancy.
- Gastrointestinal infection (eg, Salmonella, Campylobacter): Use of PPIs may increase risk of these infections.
- Hepatic impairment: Avoid use in patients with hepatic impairment.
- Renal impairment: Avoid use in patients with glomerular filtration rate (GFR) <10 mL/minute.
Concurrent drug therapy issues:
- Clopidogrel: PPIs may diminish the therapeutic effect of clopidogrel, thought to be due to reduced formation of the active metabolite of clopidogrel. The manufacturer of clopidogrel recommends either avoidance of both omeprazole (even when scheduled 12 hours apart) and esomeprazole or use of a PPI with comparatively less effect on the active metabolite of clopidogrel (eg, pantoprazole). In contrast to these warnings, others have recommended the continued use of PPIs, regardless of the degree of inhibition, in patients with a history of GI bleeding or multiple risk factors for GI bleeding who are also receiving clopidogrel since no evidence has established clinically meaningful differences in outcome; however, a clinically significant interaction cannot be excluded in those who are poor metabolizers of clopidogrel (Abraham 2010; Levine 2011).
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Asian ethnicity: Avoid use in Asian patients with unknown CYP2C19 genotype or those who are known to be poor metabolizers.
Dosage form specific issues:
- Interchangeability: Aspirin/omeprazole combination product is not interchangeable with the individual components of aspirin and omeprazole.
Other warnings/precautions:
- Laboratory test interference: Serum chromogranin A (CgA) levels increase secondary to drug-induced decreases in gastric acid; may cause false-positive results in diagnostic investigations for neuroendocrine tumors. Temporarily stop omeprazole treatment at least 14 days before CgA test; if initial CgA levels are high, repeat test to confirm. Use same commercial laboratory for testing to prevent variable results.
Monitoring Parameters
Magnesium levels (prior to initiation of therapy and periodically thereafter).
Pregnancy
Pregnancy Considerations
Use of aspirin in women ≥30 weeks gestation is associated with an increased risk for premature closure of the fetal ductus arteriosus; third trimester use may be also associated with an increased risk of neonatal complications. In addition, use of aspirin during labor may increase the risk for excessive blood loss at delivery. Use of this combination should be avoided in women ≥30 weeks gestation. Refer to individual monographs for additional information.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience nausea, vomiting, abdominal pain, or heartburn. Have patient report immediately to prescriber signs of low vitamin B-12 levels (dyspnea, dizziness, abnormal heartbeat, muscle weakness, pale skin, fatigue, mood changes, or numbness or tingling in arms or legs), signs of bleeding (vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding), signs of low magnesium (mood changes; muscle pain or weakness; muscle cramps or spasms; seizures; tremors; lack of appetite; severe nausea or vomiting; or an abnormal heartbeat), signs of kidney problems (unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain), signs of infection, signs of liver problems (dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin), signs of pancreatitis (severe abdominal pain, severe back pain, severe nausea, or vomiting), signs of lupus (rash on the cheeks or other body parts, sunburn easy, muscle or joint pain, chest pain or shortness of breath, or swelling in the arms or legs), bone pain, edema, severe dizziness, passing out, noise or ringing in the ears, signs of Clostridium difficile (C. diff)-associated diarrhea (abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools), or signs of Stevens-Johnson syndrome/toxic epidermal necrolysis (red, swollen, blistered, or peeling skin [with or without fever]; red or irritated eyes; or sores in mouth, throat, nose, or eyes) (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.