Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Caplet, oral: 500 mg
Bayer Aspirin Extra Strength: 500 mg
Bayer Genuine Aspirin: 325 mg
Bayer Women's Low Dose Aspirin: 81 mg [contains elemental calcium 300 mg]
Caplet, oral [buffered]:
Ascriptin Maximum Strength: 500 mg [contains aluminum hydroxide, calcium carbonate, magnesium hydroxide] [DSC]
Bayer Plus Extra Strength: 500 mg [contains calcium carbonate]
Caplet, enteric coated, oral:
Bayer Aspirin Regimen Regular Strength: 325 mg
Capsule Extended Release, oral:
Durlaza: 162.5 mg
Suppository, rectal: 300 mg (12s); 600 mg (12s)
Tablet, oral: 325 mg
Aspercin: 325 mg
Aspirtab: 325 mg
Bayer Genuine Aspirin: 325 mg
Tablet, oral [buffered]: 325 mg
Ascriptin Regular Strength: 325 mg [contains aluminum hydroxide, calcium carbonate, magnesium hydroxide]
Buffasal: 325 mg [contains magnesium oxide]
Bufferin: 325 mg [contains calcium carbonate, magnesium carbonate, magnesium oxide]
Bufferin Extra Strength: 500 mg [contains calcium carbonate, magnesium carbonate, magnesium oxide]
Buffinol: 324 mg [sugar free; contains magnesium oxide]
Tri-Buffered Aspirin: 325 mg [contains calcium carbonate, magnesium carbonate, magnesium oxide]
Tablet, chewable, oral: 81 mg
Bayer Aspirin Regimen Children's: 81 mg [cherry flavor]
Bayer Aspirin Regimen Children's: 81 mg [orange flavor]
St Joseph Adult Aspirin: 81 mg
Tablet, delayed release, oral: 81 mg, 325 mg
Aspirin Adult Low Dose: 81 mg
Aspirin Adult Low Strength: 81 mg
Aspirin EC Low Strength: 81 mg
Bayer Aspirin: 325 mg
Bayer Aspirin EC Low Dose: 81 mg
GoodSense Low Dose: 81 mg
Tablet, enteric coated, oral: 81 mg, 325 mg, 650 mg
Aspir-low: 81 mg
Bayer Aspirin Regimen Adult Low Strength: 81 mg
Ecotrin: 325 mg
Ecotrin Arthritis Strength: 500 mg
Ecotrin Low Strength: 81 mg
Halfprin: 81 mg [DSC]
St Joseph Adult Aspirin: 81 mg
Pharmacology
Mechanism of Action
Irreversibly inhibits cyclooxygenase-1 and 2 (COX-1 and 2) enzymes, via acetylation, which results in decreased formation of prostaglandin precursors; irreversibly inhibits formation of prostaglandin derivative, thromboxane A2, via acetylation of platelet cyclooxygenase, thus inhibiting platelet aggregation; has antipyretic, analgesic, and anti-inflammatory properties
Pharmacokinetics/Pharmacodynamics
Absorption
Immediate release: Rapidly absorbed in stomach and upper intestine (Eikelboom, 2012); Extended-release capsule: Rate of absorption is dependent upon food, alcohol, and gastric pH.
Distribution
Vd: 10 L; readily distributes into most body fluids and tissues; hydrolyzed to salicylate (active) by esterases in the GI mucosa, red blood cells, synovial fluid and blood
Metabolism
Hydrolyzed to salicylate (active) by esterases in GI mucosa, red blood cells, synovial fluid, and blood; metabolism of salicylate occurs primarily by hepatic conjugation; metabolic pathways are saturable
Excretion
Urine (75% as salicyluric acid, 10% as salicylic acid)
Onset of Action
Immediate release: Platelet inhibition: Nonenteric-coated: <1 hour; enteric-coated: 3 to 4 hours (Eikelboom 2012). Note: Chewing nonenteric-coated or enteric-coated tablets results in inhibition of platelet aggregation within 20 minutes (Eikelboom 2012; Feldman 1999; Sai 2011).
Time to Peak
Serum: Immediate release: ~1 to 2 hours (nonenteric-coated), 3 to 4 hours (enteric-coated) (Eikelboom, 2012); Extended-release capsule: ~2 hours. Note: Chewing nonenteric-coated tablets results in a time to peak concentration of 20 minutes (Feldman, 1999). Chewing enteric-coated tablets results in a time to peak concentration of 2 hours (Sai, 2011).
Duration of Action
Immediate release: 4 to 6 hours; however, platelet inhibitory effects last the lifetime of the platelet (~10 days) due to its irreversible inhibition of platelet COX-1 (Eikelboom, 2012).
Half-Life Elimination
Parent drug: Plasma concentration: 15 to 20 minutes; Salicylates (dose dependent): 3 hours at lower doses (300 to 600 mg), 5 to 6 hours (after 1 g), 10 hours with higher doses
Protein Binding
Concentration dependent; as salicylate concentration increases, protein binding decreases: ~90% to 94% (to albumin) at concentrations ≤80 mcg/mL (Rosenberg, 1981; Juurlink, 2015); ~30% with concentrations seen in overdose (Juurlink, 2015).
Use: Labeled Indications
Immediate release:
Analgesic, antipyretic, and anti-inflammatory: For the temporary relief of headache, pain, and fever caused by colds, muscle aches and pains, menstrual pain, toothache pain, and minor aches and pains of arthritis.
Revascularization procedures: For use in patients who have undergone revascularization procedures (ie, coronary artery bypass graft, percutaneous transluminal coronary angioplasty, or carotid endarterectomy).
Vascular indications, including ischemic stroke, transient ischemic attack, acute coronary syndromes (ST-elevation myocardial infarction or non-ST-elevation acute coronary syndromes [non-ST-elevation myocardial infarction or unstable angina]), secondary prevention after acute coronary syndromes, and management of stable ischemic heart disease: To reduce the combined risk of death and nonfatal stroke in patients who have had ischemic stroke or transient ischemia of the brain due to fibrin platelet emboli; to reduce the risk of vascular mortality in patients with a suspected acute myocardial infarction (MI); to reduce the combined risk of death and nonfatal MI in patients with a previous MI or unstable angina; to reduce the combined risk of MI and sudden death in patients with stable ischemic heart disease.
ER capsules:
Ischemic stroke or transient ischemic attack: To reduce the risk of death and recurrent stroke in patients who have had an ischemic stroke or transient ischemic attack.
Stable ischemic heart disease: To reduce the risk of death and MI in patients with stable ischemic heart disease.
Limitations of use: Do not use ER capsules in situations for which a rapid onset of action is required (such as acute treatment of MI or before percutaneous coronary intervention); use IR formulations instead.
Use: Off Label
Atherosclerotic cardiovascular disease, primary preventionyes
Based on the 2019 American College of Cardiology/American Heart Association (ACC/AHA) guideline on the primary prevention of cardiovascular disease and the 2019 American Diabetes Association standards of medical care in diabetes, aspirin may be used for the primary prevention of cardiovascular disease in select patients after weighing the cardiovascular disease risk versus benefits.
Carotid artery atherosclerosis, asymptomatic or symptomaticyes
Based on the 2012 American College of Chest Physicians (ACCP) guidelines for antithrombotic therapy and prevention of thrombosis (9th edition), daily aspirin is suggested in patients with asymptomatic or symptomatic carotid artery atherosclerosis based on a slight reduction in total mortality observed when aspirin is taken over 10 years (regardless of cardiovascular risk profile). The AHA/American Stroke Association guidelines for the primary prevention of stroke recommend daily aspirin for patients with asymptomatic or symptomatic carotid atherosclerosis to reduce the risk of a first stroke.
Carotid artery stentingc
A randomized, controlled trial with blinded end point adjudication evaluated carotid artery stenting versus carotid endarterectomy in patients with carotid artery stenosis. In this trial, aspirin in combination with clopidogrel was used for patients who underwent carotid artery stenting, which suggests that this antiplatelet combination is effective Brott 2010. Clinical experience also suggests the utility of this antiplatelet regimen around the time of carotid artery stenting Fairman 2019a.
Colorectal cancer risk reduction, primary preventionb
Two meta-analyses support the long-term (≥5 year) use of aspirin for primary prevention of colorectal cancer Rothwell 2010, Ye 2013.
Percutaneous coronary intervention for stable ischemic heart diseaseyes
Based on the 2011 American College of Cardiology Foundation/AHA/Society for Cardiovascular Angiography and Interventions guideline for percutaneous coronary intervention (PCI), aspirin in conjunction with other antiplatelet agents (eg, P2Y12 inhibitors and possibly glycoprotein IIb/IIIa inhibitors) is effective in reducing the frequency of ischemic complications after PCI and recommended for use prior to the procedure and indefinitely following the procedure.
Pericarditis, acute or recurrent (treatment)cyes
Data from a prospective, open-label clinical trial support the use of high-dose aspirin treatment in patients with acute low-risk pericarditis Imazio 2004.
Based on the 2015 European Society of Cardiology guidelines for the diagnosis and management of pericardial diseases, aspirin is effective and recommended for the treatment of acute or recurrent pericarditis.
Peripheral atherosclerotic disease (upper or lower extremity; with or without a revascularization procedure)yes
Based on the 2016 AHA/ACC guidelines for the management of lower extremity peripheral arterial disease (PAD), aspirin is recommended to reduce the risk of vascular events (ie, myocardial infarction, stroke, vascular death) in patients with symptomatic PAD. The use of aspirin is reasonable in asymptomatic PAD patients with an ankle-to-brachial index ≤0.9 to reduce the risk of vascular events.
Based on the ACCP guidelines for antithrombotic therapy in PAD (9th edition), aspirin is recommended for patients with symptomatic or asymptomatic PAD to prevent cardiovascular events ACCP [Alonso-Coello 2012].
Polycythemia vera, prevention of thrombosisbyes
Aspirin may be used in all patients with polycythemia vera without a history of major bleeding or gastric intolerance. Aspirin has been studied in more than 1,000 patients and is recommended in multiple polycythemia vera guidelines
Preeclampsia preventionyes
Based on the American College of Obstetricians and Gynecologists committee opinion on low-dose aspirin use during pregnancy, low-dose aspirin is effective and recommended for use in patients at risk of preeclampsia ACOG 743 2018.
Surgical prosthetic heart valve replacement (thromboprophylaxis)yes
Based on the 2014 AHA/ACC guideline for the management of patients with valvular heart disease and the 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline, aspirin in addition to a vitamin K antagonist (eg, warfarin) is effective and recommended in patients with a surgically placed mechanical prosthetic valve or bioprosthetic valve (ie, aortic or mitral position) to reduce the risk of thromboembolism (eg, stroke) and mortality.
Transcatheter aortic valve replacement (thromboprophylaxis)byes
Data from multiple clinical trials support the use of aspirin in combination with clopidogrel as an antithrombotic strategy for transcatheter aortic valve replacement (TAVR) Adams 2014, Leon 2010, Leon 2016, Reardon 2017, Smith 2011.
Based on the 2014 AHA/ACC guideline for the management of patients with valvular heart disease and 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline, life-long aspirin is effective and recommended in patients with TAVR to reduce the risk of thromboembolic events and mortality. Clopidogrel is typically used for up to 6 months after TAVR in addition to aspirin. An expert consensus pathway also suggests the utility of this antiplatelet regimen around the time of TAVR Otto 2017. The optimal postprocedure antithrombotic strategy for TAVR is unknown, especially for patients who require concomitant anticoagulation. Various antithrombotic regimens are still under investigation. Clinicians should consider patient-specific risks for bleeding and thrombosis when making pharmacotherapy plans Kalich 2018, Otto 2017.
Venous thromboembolism prevention, indefinite therapyayes
Data from randomized, double-blind, placebo-controlled trials have demonstrated that low-dose aspirin reduces the overall risk of venous thromboembolism (VTE) recurrence in patients with a first unprovoked VTE (deep vein thrombosis [DVT] or pulmonary embolism [PE]) following completion and discontinuation of oral anticoagulant therapy Becattini 2012, Simes 2014. However, data from a double-blind, randomized, placebo-controlled trial did not demonstrate a significant reduction in the rate of VTE recurrence, although it did show a significant reduction in the rate of major vascular events Brighton 2012.
Based on the ACCP guidelines for antithrombotic therapy for VTE disease, aspirin may be considered for extended treatment, after 3 months of anticoagulant therapy, to prevent VTE recurrence in patients who are stopping anticoagulant therapy following an unprovoked DVT or PE. Aspirin is not considered a reasonable alternative to anticoagulation for extended treatment because aspirin is expected to be much less effective at preventing recurrent VTE; however, in patients who have decided to stop anticoagulants, aspirin may be considered over no aspirin therapy.
Venous thromboembolism prophylaxis for total hip or knee arthroplastya
Data from a large multicenter, randomized, double-blind, controlled trial support the use of aspirin as part of a hybrid VTE prophylaxis strategy after total hip arthroplasty (THA) or total knee arthroplasty (TKA). In this trial, patients undergoing THA or TKA received rivaroxaban for VTE prophylaxis for the first 5 postoperative days then switched to aspirin or continued rivaroxaban for an additional 30 days (35 days total) for THA or an additional 9 days (14 days total) for TKA. Aspirin was found to be noninferior to rivaroxaban at preventing symptomatic VTE, with no difference in bleeding Anderson 2018. Some experts recommend limiting this strategy to low-risk patients who undergo elective unilateral THA or TKA, ambulate within 24 hours after surgery, and have none of the following: additional risk factors for VTE, indications for long-term anticoagulation, lower limb or hip fracture in the previous 3 months, or expected major surgery in the upcoming 3 months Pai 2018.
Contraindications
Hypersensitivity to NSAIDs; patients with asthma, rhinitis, and nasal polyps; use in children or teenagers for viral infections, with or without fever.
Documentation of allergenic cross-reactivity for salicylates is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Note: Ibuprofen, naproxen, and possibly other nonselective nonsteroidal anti-inflammatory drugs (NSAIDs) may reduce the cardioprotective effects of aspirin (Capone 2005; Catella-Lawson 2001; MacDonald 2003). Avoid regular or frequent use of NSAIDs in patients receiving aspirin for cardiovascular protection. An ER formulation exists (162.5 mg capsule); however, it should not be used in situations when a rapid onset of action is necessary (eg, ST-elevation myocardial infarction [MI]); dosing information provided is based on the IR formulations.
Analgesic and antipyretic: Immediate release: Oral: 325 mg to 1 g every 4 to 6 hours as needed; usual maximum daily dose: 4 g/day (Abramson 2019). Note: If patient cannot take orally, rectal suppositories (300 or 600 mg) are available.
Anti-inflammatory for arthritis associated with rheumatic disease: Immediate release: Oral: 4 to 8 g/day in 4 to 5 divided doses as needed; titrate dose based on response and tolerability. Continue treatment until symptoms resolve (typically 1 to 2 weeks, but potentially up to 8 weeks). Use of aspirin at these high doses (4 to 8 g/day) may be limited by adverse effects (tinnitus, diminished auditory acuity, GI intolerance) (Abramson 2019; Carapetis 2012; Steer 2019).
Atherosclerotic cardiovascular disease:
Acute coronary syndrome: Note: For rapid onset, non-enteric-coated IR tablet(s) should be chewed and swallowed upon identification of clinical and ECG findings suggesting an acute coronary syndrome. Enteric-coated aspirin is not preferred since onset of action may be delayed. If it is the only product available, enteric-coated IR tablet(s) may be chewed and swallowed (ACCP [Eikelboom 2012]; Sai 2011). For maintenance therapy, any oral formulation is acceptable for use.
Non-ST-elevation acute coronary syndromes or ST-elevation myocardial infarction: Note: For initial therapy, administer aspirin in combination with an IV anticoagulant and a P2Y12 inhibitor (ACC/AHA [Amsterdam 2014]; ACCF/AHA [O'Gara 2013]).
Initial:
Immediate release (non-enteric-coated): Oral: 162 to 325 mg administered once (chew and swallow) at the time of diagnosis (ACC/AHA [Amsterdam 2014]; ACCF/AHA [O'Gara 2013]).
Rectal (alternative route): 600 mg administered once at the time of diagnosis if an IR oral formulation is unavailable or oral route is not feasible (Maalouf 2009).
Maintenance (secondary prevention): Immediate release: Oral: 75 to 100 mg once daily (ACC/AHA [Levine 2016]; Hennekens 2019; Mehta 2001).
Duration of therapy: Aspirin plus a P2Y12 inhibitor (dual antiplatelet therapy [DAPT]) should be continued for ≥12 months unless bleeding risk is a concern. If there have been no major bleeding complications after 12 months, continuation of DAPT may be considered. Re-evaluate the need for DAPT at regular intervals based on bleeding and thrombotic risks. When DAPT is complete, discontinue the P2Y12 inhibitor and continue aspirin indefinitely (ACC/AHA [Levine 2016]; Bonaca 2015; Cutlip 2019a; Lincoff 2019; Mauri 2014; Mehta 2001; Wallentin 2009; Wiviott 2007; Yusuf 2001).
Percutaneous coronary intervention for stable ischemic heart disease (off-label use):
Initial: Note: For initial therapy, non-enteric-coated IR tablet(s) should be administered. Enteric-coated aspirin is not preferred since onset of action is delayed. For patients who receive a coronary stent during percutaneous coronary intervention, administer aspirin in combination with an IV anticoagulant and clopidogrel (ACCF/AHA/SCAI [Levine 2011]).
Patients chronically taking aspirin ≥325 mg/day prior to percutaneous coronary intervention: Immediate release (non-enteric-coated): Oral: 75 to 100 mg prior to the procedure (Cutlip 2020); some experts recommend doses up to 325 mg (ACCF/AHA/SCAI [Levine 2011]).
Patients not chronically taking aspirin or chronically taking aspirin <325 mg/day prior to percutaneous coronary intervention: Immediate release (non-enteric-coated): Oral: 300 to 325 mg given ≥2 hours (preferably 24 hours) before the procedure (ACCF/AHA/SCAI [Levine 2011]; Cutlip 2020).
Maintenance: Immediate release: Oral: 75 to 100 mg once daily in combination with clopidogrel (DAPT); upon completion of the recommended duration of DAPT, continue aspirin indefinitely (ACC/AHA [Levine 2016]; Cutlip 2019c). Refer to Clopidogrel monograph for information on duration of DAPT.
Atherosclerotic cardiovascular disease, primary prevention (off-label use): Note: Use should be a shared decision between health care professionals and patients after weighing the cardiovascular disease risk versus benefits (ACC/AHA [Arnett 2019]).
Immediate release: Oral: 75 to 100 mg once daily (ACC/AHA [Arnett 2019]).
Atherosclerotic cardiovascular disease, secondary prevention:
Carotid artery atherosclerosis, asymptomatic or symptomatic (off-label use): Immediate release: Oral: 75 to 325 mg once daily (ACCP [Alonso-Coello 2012]; Walker 1995).
Coronary artery bypass graft surgery: Immediate release: Oral: 75 to 81 mg once daily beginning preoperatively; continue indefinitely following surgery (AHA [Kulik 2015]; Aranki 2019).
Off-pump coronary artery bypass graft surgery: Following surgery, consider adding clopidogrel in combination with aspirin for 12 months then discontinue clopidogrel and continue aspirin indefinitely (AHA [Kulik 2015]).
Patients with acute coronary syndrome followed by coronary artery bypass graft surgery: Administer aspirin in combination with a P2Y12 inhibitor for 12 months then continue aspirin indefinitely (AHA [Kulik 2015]). Some experts do not use P2Y12 inhibitors postoperatively in these patients (Aranki 2019).
Ischemic stroke/Transient ischemic attack:
Cardioembolic stroke (alternative agent): Note: Oral anticoagulation is preferred. For patients who cannot take an oral anticoagulant, may consider aspirin as an alternative (AHA/ASA [Kernan 2014]).
Immediate release: Oral: 75 to 100 mg once daily (AHA/ASA [Kernan 2014]).
Intracranial atherosclerosis (50% to 99% stenosis of a major intracranial artery), secondary prevention: Immediate release: Oral: 325 mg once daily; for patients with recent stroke or transient ischemic attack (within 30 days) may consider short-term use of clopidogrel (for 21 or 90 days depending on degree of stenosis) in combination with aspirin (AHA/ASA [Kernan 2014]; Chimowitz 2011) followed by single-agent antiplatelet therapy with aspirin, clopidogrel, or aspirin/ER dipyridamole indefinitely (ACCP [Lansberg 2012]; AHA/ASA [Kernan 2014]; Cucchiara 2019).
Noncardioembolic ischemic stroke/transient ischemic attack: Note: For patients with a minor stroke (National Institutes of Health Stroke Scale score ≤3) or high-risk transient ischemic attack (ABCD2 score ≥4), may consider short-term use of clopidogrel (for 21 days) in combination with aspirin (AHA/ASA [Kernan 2014]; AHA/ASA [Powers 2018]) followed by single-agent antiplatelet therapy with aspirin, clopidogrel, or aspirin/ER dipyridamole indefinitely (ACCP [Lansberg 2012]; AHA/ASA [Kernan 2014]; Cucchiara 2019).
Initial:
Immediate release: Oral: 162 to 325 mg administered once at the time of diagnosis; in patients who receive IV alteplase, antiplatelet therapy is generally delayed for ≥24 hours, but administered as soon as possible thereafter (AHA/ASA [Kernan 2014]; AHA/ASA [Powers 2018]; Filho 2019).
Rectal (alternative route): 300 mg administered once at the time of diagnosis if oral route is not feasible (IST 1997; Sandercock 2014).
Maintenance (alternative agent): Note: Some experts prefer clopidogrel over aspirin or combination aspirin/ER dipyridamole over aspirin alone for long-term secondary prevention (ACCP [Lansberg 2012]; Cucchiara 2019).
Immediate release: Oral: 50 to 100 mg once daily (ACCP [Lansberg 2012]; AHA/ASA [Kernan 2014]; Cucchiara 2019).
Peripheral atherosclerotic disease (upper or lower extremity; with or without a revascularization procedure) (off-label use): Immediate release: Oral: 75 to 100 mg once daily (ACCP [Alonso-Coello 2012]; AHA/ACC [Gerhard-Herman 2017]).
Stable ischemic heart disease: Immediate release: Oral: 75 to 100 mg once daily (ACCF/AHA [Fihn 2012]; Kannam 2019).
Carotid artery stenting (off-label use):
Initial:
Initiation ≥48 hours before procedure: Immediate release: Oral: 325 to 650 mg once daily in combination with clopidogrel (Brott 2010; Fairman 2019a).
Initiation <48 hours before procedure: Immediate release: Oral: 650 mg once ≥4 hours before procedure in combination with clopidogrel (Brott 2010; Fairman 2019a).
Maintenance: Immediate release: Oral: 325 mg once daily in combination with clopidogrel for 6 weeks, then discontinue clopidogrel and continue aspirin 325 mg once daily indefinitely thereafter. In patients with history of neck irradiation, some experts recommend continuing aspirin plus clopidogrel indefinitely (Brott 2010; Fairman 2019a).
Carotid endarterectomy: Immediate release: Oral: 75 to 325 mg once daily starting prior to surgery and continued indefinitely (ACCP [Alonso-Coello 2012]; Fairman 2019b).
Colorectal cancer risk reduction, primary prevention (off-label use): Note: The optimal dose and duration of therapy for colorectal cancer risk reduction are unknown. Utilization should be a shared decision between health care professionals and patients that weighs the risk versus benefits of treatment (Chan 2019).
Immediate release: Oral: 75 to 325 mg once daily (Chan 2019; Rothwell 2010; Ye 2013).
Pericarditis, acute or recurrent (treatment) (off-label use): Note: Preferred over other NSAIDs in patients with ischemic heart disease since aspirin is required. If pericarditis occurs after an MI, avoid anti-inflammatory doses for 7 to 10 days unless symptoms require acute treatment (LeWinter 2019).
Immediate release: Oral: Initial: 650 mg to 1 g every 8 hours until resolution of symptoms; gradually taper off over several weeks by decreasing the dose by 250 to 500 mg every 1 to 2 weeks (ESC [Adler 2015]; Imazio 2020). Use in combination with colchicine. In patients at risk of NSAID-related GI toxicity, prophylaxis (generally with a proton pump inhibitor) is recommended (Adler 2019; ESC [Adler 2015]; Imazio 2020).
Polycythemia vera, prevention of thrombosis (off-label use): Note: Avoid use in patients with concurrent acquired von Willebrand syndrome (Tefferi 2019).
Immediate release: Oral: 75 to 100 mg once or twice daily (Barbui 2006; Landolfi 2004; McMullin 2005; Pascale 2012; Tefferi 2017).
Preeclampsia prevention (off-label use): Note: Consider for use in pregnant women with ≥2 moderate risk factors or ≥1 high risk factor for preeclampsia (ACOG 743 2018).
Immediate release: Oral: 81 to 162 mg once daily, ideally beginning between 12 to 16 weeks' gestation but may be started up to 28 weeks' gestation; continue therapy until delivery (ACOG 743 2018; Rolnik 2017).
Valvular heart disease:
Surgical prosthetic heart valve replacement (thromboprophylaxis):
Bioprosthetic aortic or mitral heart valve replacement (off-label use): Immediate release: Oral: 75 to 100 mg once daily; use in combination with warfarin for the first 3 to 6 months after surgery; continue aspirin indefinitely (ACC [Otto 2017]; AHA/ACC [Nishimura 2014]; AHA/ACC [Nishimura 2017]).
Mechanical aortic or mitral heart valve replacement (off-label use): Immediate release: Oral: 75 to 100 mg once daily in combination with warfarin (AHA/ACC [Nishimura 2014]; AHA/ACC [Nishimura 2017]).
Transcatheter aortic valve replacement (thromboprophylaxis) (off-label use): Immediate release: Oral: 75 to 100 mg once daily; use in combination with clopidogrel for 3 to 6 months after transcatheter aortic valve replacement depending on the type of valve that was implanted; continue aspirin indefinitely (AHA/ACC [Nishimura 2014]; AHA/ACC [Nishimura 2017]).
Venous thromboembolism prevention, indefinite therapy (off-label use): Note: For use in select patients to prevent recurrent venous thromboembolism (VTE) if unable to take an anticoagulant. In patients who have completed ≥6 months of anticoagulation and in whom indefinite therapeutic anticoagulation is indicated, aspirin is not recommended since it is less effective (Lip 2019).
Immediate release: Oral: 100 mg once daily after completion of a conventional treatment course with therapeutic anticoagulation (Becattini 2012; Brighton 2012; Lip 2019; Simes 2014).
Venous thromboembolism prophylaxis for total hip or total knee arthroplasty (off-label use): Note: This is a hybrid strategy using rivaroxaban followed by aspirin. Limit this strategy to low-risk patients who undergo elective unilateral total hip arthroplasty (THA) or total knee arthroplasty (TKA), ambulate within 24 hours after surgery, and do not have additional risk factors for VTE, indications for long-term anticoagulation, lower limb or hip fracture in the previous 3 months, or expected major surgery in the upcoming 3 months (Pai 2018).
Immediate release: Oral: After a 5-day course of postoperative rivaroxaban prophylaxis, initiate aspirin 81 mg once daily on postoperative day 6 and continue for 9 days for TKA (total duration: 14 days) or 30 days for THA (total duration: 35 days) (Anderson 2018).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Doses are typically rounded to a convenient amount (eg, 1/4 of 81 mg tablet):
Analgesic: Oral, rectal: Note: Do not use aspirin in pediatric patients <18 years who have or who are recovering from chickenpox or flu symptoms (eg, viral illness) due to the association with Reye syndrome (APS 2016):
Infants, Children, and Adolescents weighing <50 kg: Limited data available: 10 to 15 mg/kg/dose every 4 to 6 hours; maximum daily dose: 90 mg/kg/day or 4,000 mg/day whichever is less (APS 2016)
Children ≥12 years and Adolescents weighing ≥50 kg: 325 to 650 mg every 4 to 6 hours; maximum daily dose: 4,000 mg/day
Anti-inflammatory: Limited data available: Infants, Children, and Adolescents: Oral: Initial: 60 to 90 mg/kg/day in divided doses; usual maintenance: 80 to 100 mg/kg/day divided every 6 to 8 hours; monitor serum concentrations (Levy 1978)
Antiplatelet effects: Limited data available: Infants, Children, and Adolescents: Oral: Adequate pediatric studies have not been performed; pediatric dosage is derived from adult studies. Usual adult maximum daily dose for antiplatelet effects is 325 mg/day.
Acute ischemic stroke (AIS):
Noncardioembolic: 1 to 5 mg/kg/dose once daily for ≥2 years; patients with recurrent AIS or TIAs should be transitioned to clopidogrel, LMWH, or warfarin (ACCP [Monagle 2012])
Secondary to Moyamoya and non-Moyamoya vasculopathy: 1 to 5 mg/kg/dose once daily; Note: In non-Moyamoya vasculopathy, continue aspirin for 3 months, with subsequent use guided by repeat cerebrovascular imaging (ACCP [Monagle 2012]).
Prosthetic heart valve:
Bioprosthetic aortic valve (with normal sinus rhythm): 1 to 5 mg/kg/dose once daily for 3 months (AHA [Giglia 2013]; ACCP [Guyatt 2012]; ACCP [Monagle 2012])
Mechanical aortic and/or mitral valve: 1 to 5 mg/kg/dose once daily combined with vitamin K antagonist (eg, warfarin) is recommended as first-line antithrombotic therapy (ACCP [Guyatt 2012]; ACCP [Monagle 2012]). Alternative regimens: 6 to 20 mg/kg/dose once daily in combination with dipyridamole (Bradley 1985; el Makhlouf 1987; LeBlanc 1993; Serra 1987; Solymar 1991)
Shunts: Blalock-Taussig; Glenn; postoperative; primary prophylaxis: 1 to 5 mg/kg/dose once daily (ACCP [Monagle 2012]; AHA [Giglia 2013])
Norwood, Fontan surgery, postoperative; primary prophylaxis: 1 to 5 mg/kg/dose once daily (ACCP [Monagle 2012]; AHA [Giglia 2013])
Transcatheter Atrial Septal Defect (ASD) or Ventricular Septal Defect (VSD) devices, postprocedure prophylaxis: 1 to 5 mg/kg/dose once daily starting one to several days prior to implantation and continued for at least 6 months. For older children and adolescents, after device closure of ASD, an additional anticoagulant may be given with aspirin for 3 to 6 months, but the aspirin should continue for at least 6 months (AHA [Giglia 2013]).
Ventricular assist device (VAD) placement: 1 to 5 mg/kg/dose once daily initiated within 72 hours of VAD placement; should be used with heparin (initiated between 8 to 48 hours following implantation) and with or without dipyridamole (ACCP [Monagle 2012])
Kawasaki disease: Limited data available; optimal dose not established: Note: Patients with Kawasaki disease and presenting with influenza or viral illness should not receive aspirin; acetaminophen is suggested as an antipyretic in these patients and an alternate antiplatelet agent suggested for a minimum of 2 weeks (AHA [McCrindle 2017]).
Infants, Children, and Adolescents: Oral:
Initial therapy (acute phase): Recommended dosing regimens vary. Use in combination with IV immune globulin (within first 10 days of symptom onset) and corticosteroids in some cases.
High dose: 80 to 100 mg/kg/day divided every 6 hours for up to 14 days until fever resolves for at least 48 to 72 hours (AAP [Red Book 2015]; ACCP [Monagle 2012]; AHA [Giglia 2013]; AHA [McCrindle 2017])
Moderate dose: 30 to 50 mg/kg/day divided every 6 hours for up to 14 days until fever resolves for at least 48 to 72 hours (AHA [McCrindle 2017])
Subsequent therapy (low-dose; antiplatelet effects): 3 to 5 mg/kg/day once daily; reported dosing range: 1 to 5 mg/kg/day; initiate after fever resolves for at least 48 to 72 hours (or after 14 days). In patients without coronary artery abnormalities, administer the lower dose for 6 to 8 weeks. In patients with coronary artery abnormalities, low-dose aspirin should be continued indefinitely (in addition to therapy with warfarin) (AAP [Red Book 2015]; ACCP [Monagle 2012]; AHA [Giglia 2013]; AHA [McCrindle 2017]).
Rheumatic fever: Limited data available: Infants, Children, and Adolescents: Oral: Initial: 100 mg/kg/day divided into 4 to 5 doses; if response inadequate, may increase dose to 125 mg/kg/day; continue for 2 weeks; then decrease dose to 60 to 70 mg/kg/day in divided doses for an additional 3 to 6 weeks (WHO Guidelines 2004)
Migratory polyarthritis, with carditis without cardiomegaly or congestive heart failure: Initial: 100 mg/kg/day in 4 divided doses for 3 to 5 days, followed by 75 mg/kg/day in 4 divided doses for 4 weeks
Carditis and cardiomegaly or congestive heart failure: At the beginning of the tapering of the prednisone dose, aspirin should be started at 75 mg/kg/day in 4 divided doses for 6 weeks
Administration
Oral:
IR tablets: Administer with food or a full glass of water to minimize GI distress. In situations for which a rapid onset of action is required (eg, acute treatment of myocardial infarction), have patient chew IR tablet.
Preeclampsia (prevention): Administration as an evening dose may be more beneficial than administration in the morning (Ayala 2013; Rolnik 2017)
ER capsules: Do not cut, crush, or chew. Administer with a full glass of water at the same time each day. Do not administer 2 hours before or 1 hour after alcohol consumption.
Rectal: Remove suppository from plastic packet and insert into rectum as far as possible.
Storage
Store oral dosage forms (caplets, tablets, capsules) at room temperature; protect from moisture; see product-specific labeling for details. Keep suppositories in refrigerator; do not freeze. Hydrolysis of aspirin occurs upon exposure to water or moist air, resulting in salicylate and acetate, which possess a vinegar-like odor. Do not use if a strong odor is present.
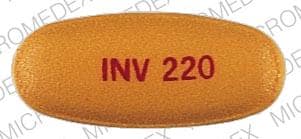
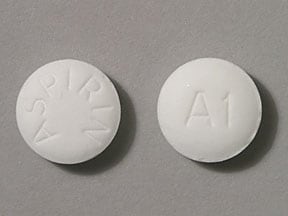
Aspirin Images
Drug Interactions
Acalabrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the antiplatelet effect of other Agents with Antiplatelet Properties. Monitor therapy
Ajmaline: Salicylates may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Alcohol (Ethyl): May enhance the adverse/toxic effect of Aspirin. Specifically, alcohol may increase the bleeding risk of aspirin. Alcohol (Ethyl) may diminish the therapeutic effect of Aspirin. Specifically, alcohol may interfere with the controlled release mechanism of extended release aspirin. Management: Monitor patients who drink 3 or more alcoholic drinks a day for increased bleeding while taking aspirin. Counsel patients about the risk of bleeding and discourage such consumption. Give extended release aspirin 2 hours before, or 1 hour after, alcohol. Consider therapy modification
Alendronate: Aspirin may enhance the adverse/toxic effect of Alendronate. Specifically, the incidence of upper gastrointestinal adverse events may be increased Monitor therapy
Ammonium Chloride: May increase the serum concentration of Salicylates. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Salicylates may enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Salicylates may diminish the therapeutic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Anticoagulants: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Anticoagulants. Exceptions: Bemiparin; Enoxaparin; Heparin. Monitor therapy
Anticoagulants: Salicylates may enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Apixaban: Aspirin may enhance the adverse/toxic effect of Apixaban. Specifically, the risk for bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely. Consider therapy modification
Bemiparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin with antiplatelet agents. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Benzbromarone: Salicylates may diminish the therapeutic effect of Benzbromarone. Monitor therapy
Blood Glucose Lowering Agents: Salicylates may enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Calcium Channel Blockers (Nondihydropyridine): May enhance the antiplatelet effect of Aspirin. Monitor therapy
Carbonic Anhydrase Inhibitors: Salicylates may enhance the adverse/toxic effect of Carbonic Anhydrase Inhibitors. Salicylate toxicity might be enhanced by this same combination. Management: Avoid these combinations when possible.Dichlorphenamide use with high-dose aspirin as contraindicated. If another combination is used, monitor patients closely for adverse effects. Tachypnea, anorexia, lethargy, and coma have been reported. Exceptions: Brinzolamide; Dorzolamide. Consider therapy modification
Carisoprodol: Aspirin may increase serum concentrations of the active metabolite(s) of Carisoprodol. Specifically, Meprobamate concentrations may be increased. Aspirin may decrease the serum concentration of Carisoprodol. Monitor therapy
Cephalothin: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Cephalothin. Specifically, the risk for bleeding may be increased. Monitor therapy
Collagenase (Systemic): Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
Corticosteroids (Systemic): Salicylates may enhance the adverse/toxic effect of Corticosteroids (Systemic). These specifically include gastrointestinal ulceration and bleeding. Corticosteroids (Systemic) may decrease the serum concentration of Salicylates. Withdrawal of corticosteroids may result in salicylate toxicity. Monitor therapy
Dabigatran Etexilate: Aspirin may enhance the adverse/toxic effect of Dabigatran Etexilate. Specifically, the risk for bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling states that low dose aspirin could be considered, but the use of antiplatelets are not recommended for stroke prevention in patients with atrial fibrillation. Consider therapy modification
Dasatinib: May enhance the anticoagulant effect of Agents with Antiplatelet Properties. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Deoxycholic Acid: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Dexibuprofen: Aspirin may enhance the adverse/toxic effect of Dexibuprofen. Dexibuprofen may diminish the cardioprotective effect of Aspirin. Avoid combination
Dexketoprofen: Salicylates may enhance the adverse/toxic effect of Dexketoprofen. Dexketoprofen may diminish the therapeutic effect of Salicylates. Salicylates may decrease the serum concentration of Dexketoprofen. Management: The use of high-dose salicylates (3 g/day or more in adults) together with dexketoprofen is inadvisable. Consider administering dexketoprofen 30-120 min after or at least 8 hrs before cardioprotective doses of aspirin to minimize any possible interaction. Avoid combination
Edoxaban: Aspirin may enhance the adverse/toxic effect of Edoxaban. Specifically, the risk of bleeding may be increased. Aspirin may increase the serum concentration of Edoxaban. Management: Carefully consider the anticipated risks and benefits of this combination. If combined, increased monitoring for bleeding is recommended. Consider therapy modification
Enoxaparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue antiplatelet agents prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Fat Emulsion (Fish Oil Based): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Felbinac: May enhance the adverse/toxic effect of Aspirin. Monitor therapy
Floctafenine: May enhance the adverse/toxic effect of Aspirin. An increased risk of bleeding may be associated with use of this combination. Floctafenine may diminish the cardioprotective effect of Aspirin. Avoid combination
Ginkgo Biloba: May enhance the anticoagulant effect of Salicylates. Management: Consider alternatives to this combination of agents. Monitor for signs and symptoms of bleeding (especially intracranial bleeding) if salicylates are used in combination with ginkgo biloba. Consider therapy modification
Glucosamine: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Gold Sodium Thiomalate: Aspirin may enhance the adverse/toxic effect of Gold Sodium Thiomalate. Specifically, liver function tests may be elevated when these agents are combined. Monitor therapy
Heparin: Aspirin may enhance the anticoagulant effect of Heparin. Monitor therapy
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Bleeding may occur. Management: Avoid combination when possible. If used, monitor more closely for evidence of bleeding. Discontinue herbal products with anticoagulant or antiplatelet actions 2 weeks prior to surgical, dental, or invasive procedures. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Salicylates. Bleeding may occur. Consider therapy modification
Hyaluronidase: Salicylates may diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving salicylates (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. Consider therapy modification
Ibritumomab Tiuxetan: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to impaired platelet function and an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Influenza Virus Vaccine (Live/Attenuated): May enhance the adverse/toxic effect of Salicylates. Specifically, Reye's syndrome may develop. Avoid combination
Inotersen: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Ketorolac (Nasal): May enhance the adverse/toxic effect of Aspirin. An increased risk of bleeding may be associated with use of this combination. Ketorolac (Nasal) may diminish the cardioprotective effect of Aspirin. Avoid combination
Ketorolac (Systemic): May enhance the adverse/toxic effect of Aspirin. An increased risk of bleeding may be associated with use of this combination. Ketorolac (Systemic) may diminish the cardioprotective effect of Aspirin. Avoid combination
Lesinurad: Aspirin may diminish the therapeutic effect of Lesinurad. Monitor therapy
Limaprost: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Loop Diuretics: Salicylates may diminish the diuretic effect of Loop Diuretics. Loop Diuretics may increase the serum concentration of Salicylates. Monitor therapy
Macimorelin: Aspirin may diminish the diagnostic effect of Macimorelin. Avoid combination
Methotrexate: Salicylates may increase the serum concentration of Methotrexate. Salicylate doses used for prophylaxis of cardiovascular events are not likely to be of concern. Consider therapy modification
Multivitamins/Fluoride (with ADE): May enhance the antiplatelet effect of Aspirin. Aspirin may decrease the serum concentration of Multivitamins/Fluoride (with ADE). Specifically, aspirin may decrease the absorption of ascorbic acid. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the antiplatelet effect of Aspirin. Aspirin may decrease the serum concentration of Multivitamins/Minerals (with ADEK, Folate, Iron). Specifically, aspirin may decrease absorption of ascorbic acid. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the antiplatelet effect of Aspirin. Aspirin may decrease the serum concentration of Multivitamins/Minerals (with AE, No Iron). Specifically, aspirin may decrease the absorption of ascorbic acid. Monitor therapy
Nicorandil: Aspirin may enhance the adverse/toxic effect of Nicorandil. Specifically, the risk of gastrointestinal ulceration and hemorrhage may be increased. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): Aspirin may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Management: Concurrent use of aspirin at doses beyond cardioprotective levels is not recommended. While concurrent use of low-dose aspirin with a COX-2 inhibitor is permissable, patients should be monitored closely for signs/symptoms of GI ulceration/bleeding. Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents (Nonselective): May enhance the adverse/toxic effect of Salicylates. An increased risk of bleeding may be associated with use of this combination. Nonsteroidal Anti-Inflammatory Agents (Nonselective) may diminish the cardioprotective effect of Salicylates. Salicylates may decrease the serum concentration of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Consider therapy modification
Obinutuzumab: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Omacetaxine: Aspirin may enhance the adverse/toxic effect of Omacetaxine. Specifically, the risk for bleeding-related events may be increased. Management: Avoid concurrent use of aspirin with omacetaxine in patients with a platelet count of less than 50,000/uL. Avoid combination
Omega-3 Fatty Acids: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Pentosan Polysulfate Sodium: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Specifically, the risk of bleeding may be increased by concurrent use of these agents. Monitor therapy
Pentoxifylline: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Potassium Phosphate: May increase the serum concentration of Salicylates. Monitor therapy
PRALAtrexate: Salicylates may increase the serum concentration of PRALAtrexate. Salicylate doses used for prophylaxis of cardiovascular events are unlikely to be of concern. Consider therapy modification
Probenecid: Salicylates may diminish the therapeutic effect of Probenecid. Monitor therapy
Prostacyclin Analogues: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Rivaroxaban: Aspirin may enhance the adverse/toxic effect of Rivaroxaban. Specifically, the risk of bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely. Consider therapy modification
Salicylates: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Salicylates: May enhance the anticoagulant effect of other Salicylates. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the antiplatelet effect of Aspirin. Monitor therapy
Serotonin/Norepinephrine Reuptake Inhibitors: May enhance the antiplatelet effect of Aspirin. Monitor therapy
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Spironolactone: Aspirin may diminish the therapeutic effect of Spironolactone. Monitor therapy
Sucroferric Oxyhydroxide: May decrease the serum concentration of Aspirin. Management: Administer aspirin at least 1 hour before administration of sucroferric oxyhydroxide. Consider therapy modification
Sulfinpyrazone: Salicylates may decrease the serum concentration of Sulfinpyrazone. Avoid combination
Talniflumate: Aspirin may enhance the adverse/toxic effect of Talniflumate. Management: When possible, consider alternatives to this combination. Concurrent use is generally not recommended. Consider therapy modification
Thiopental: Aspirin may decrease the protein binding of Thiopental. Monitor therapy
Thrombolytic Agents: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Thrombolytic Agents. Monitor therapy
Thrombolytic Agents: Salicylates may enhance the adverse/toxic effect of Thrombolytic Agents. An increased risk of bleeding may occur. Monitor therapy
Ticagrelor: Aspirin may enhance the antiplatelet effect of Ticagrelor. Aspirin may diminish the therapeutic effect of Ticagrelor. More specifically, the benefits of ticagrelor relative to clopidogrel may be diminished in adult patients receiving daily aspirin doses greater than 100-150 mg daily. Management: Avoid daily aspirin doses greater than 100 mg in adults receiving ticagrelor. Canadian recommendations are to avoid adult daily aspirin doses greater than 150 mg. Daily low-dose aspirin (U.S.: 75-100 mg; Canada: 75-150 mg) is recommended. Consider therapy modification
Tiludronate: Aspirin may decrease the serum concentration of Tiludronate. Monitor therapy
Tipranavir: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Tricyclic Antidepressants (Tertiary Amine): May enhance the antiplatelet effect of Aspirin. Monitor therapy
Urokinase: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Urokinase. Avoid combination
Valproate Products: Salicylates may increase the serum concentration of Valproate Products. Monitor therapy
Varicella Virus-Containing Vaccines: Salicylates may enhance the adverse/toxic effect of Varicella Virus-Containing Vaccines. Specifically, the risk for Reye's syndrome may increase. Avoid combination
Vitamin E (Systemic): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Salicylates may enhance the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Zanubrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Test Interactions
False-negative results for glucose oxidase urinary glucose tests (Clinistix); false-positives using the cupric sulfate method (Clinitest); also, interferes with Gerhardt test, VMA determination; 5-HIAA, xylose tolerance test and T3 and T4; may lead to false-positive aldosterone/renin ratio (ARR) (Funder 2016)
Adverse Reactions
As with all drugs which may affect hemostasis, bleeding is associated with aspirin. Hemorrhage may occur at virtually any site. Risk is dependent on multiple variables including dosage, concurrent use of multiple agents which alter hemostasis, and patient susceptibility. Many adverse effects of aspirin are dose related, and are rare at low dosages. Other serious reactions are idiosyncratic, related to allergy or individual sensitivity. Accurate estimation of frequencies is not possible. The reactions listed below have been reported for aspirin.
Cardiovascular: Cardiac arrhythmia, edema, hypotension, tachycardia
Central nervous system: Agitation, cerebral edema, coma, confusion, dizziness, fatigue, headache, hyperthermia, insomnia, lethargy, nervousness, Reye's syndrome
Dermatologic: Skin rash, urticaria
Endocrine & metabolic: Acidosis, dehydration, hyperglycemia, hyperkalemia, hypernatremia (buffered forms), hypoglycemia (children)
Gastrointestinal: Gastrointestinal ulcer (6% to 31%), duodenal ulcer, dyspepsia, epigastric distress, gastritis, gastrointestinal erosion, heartburn, nausea, stomach pain, vomiting
Genitourinary: Postpartum hemorrhage, prolonged gestation, prolonged labor, proteinuria, stillborn infant
Hematologic & oncologic: Anemia, blood coagulation disorder, disseminated intravascular coagulation, hemolytic anemia, hemorrhage, iron deficiency anemia, prolonged prothrombin time, thrombocytopenia
Hepatic: Hepatitis (reversible), hepatotoxicity, increased serum transaminases
Hypersensitivity: Anaphylaxis, angioedema
Neuromuscular & skeletal: Acetabular bone destruction, rhabdomyolysis, weakness
Otic: Hearing loss, tinnitus
Renal: Increased blood urea nitrogen, increased serum creatinine, interstitial nephritis, renal failure (including cases caused by rhabdomyolysis), renal insufficiency, renal papillary necrosis
Respiratory: Asthma, bronchospasm, dyspnea, hyperventilation, laryngeal edema, noncardiogenic pulmonary edema, respiratory alkalosis, tachypnea
Miscellaneous: Low birth weight
Postmarketing and/or case reports: Anorectal stenosis (suppository), atrial fibrillation (toxicity), cardiac conduction disturbance (toxicity), cerebral infarction (ischemic), cholestatic jaundice, colitis, colonic ulceration, coronary artery vasospasm, delirium, esophageal obstruction, esophagitis (with esophageal ulcer), hematoma (esophageal), macular degeneration (age-related) (Li 2015), periorbital edema, rhinosinusitis
Warnings/Precautions
Concerns related to adverse effects:
- Salicylate sensitivity: Patients with sensitivity to tartrazine dyes, nasal polyps, and asthma may have an increased risk of salicylate sensitivity.
- Tinnitus: Discontinue use if tinnitus or impaired hearing occurs.
- Upper gastrointestinal (UGI) events (eg, symptomatic or complicated ulcers): Low-dose aspirin for cardioprotective effects is associated with a two- to fourfold increase in UGI events. The risks of these events increase with increasing aspirin dose; during the chronic phase of aspirin dosing, doses >81 mg are not recommended unless indicated (Bhatt 2008).
Disease-related concerns:
- Bariatric surgery:
– Altered absorption and efficacy: Altered absorption and efficacy may occur. The Tmax of salicylic acid after gastric bypass was observed to be significantly shorter after surgery. Cmax and AUC0-24 were also significantly higher (Mitrov-Winkelmolen 2016). In a mixed surgery population (80% gastric bypass, 20% sleeve), aspirin-induced platelet reactivity was significantly reduced and correlated to the extent of weight loss after surgery (Norgard 2017).
– Gastric ulceration: Evaluate the risk vs benefit of aspirin after surgery; if aspirin therapy is continued (eg, cardiovascular indications), use the lowest possible dose with concurrent administration of proton pump inhibitor (PPI); risk of gastric ulceration after gastric bypass and sleeve gastrectomy may be increased. A population-based study of over 20,000 patients identifying risk factors for marginal ulceration after gastric bypass suggests limited doses of aspirin may not increase risk whereas higher doses may (Sverden 2016). Another study identified that following gastric bypass, there is no significant difference in marginal ulceration rate between those given low-dose aspirin and those not on aspirin; however, long-term PPI therapy (>90 days) was found to significantly reduce marginal ulceration rate in both groups (Kang 2017).
- Bleeding disorders: Use with caution in patients with platelet and bleeding disorders.
- Dehydration: Use with caution in patients with dehydration.
- Ethanol use: Heavy ethanol use (>3 drinks/day) can increase bleeding risks and may enhance gastric mucosal damage.
- Gastrointestinal disease: Use with caution in patients with erosive gastritis. Avoid use in patients with active peptic ulcer disease.
- Hepatic impairment: Avoid use in severe hepatic failure.
- Renal impairment: When using high dosages (eg, analgesic or anti-inflammatory uses), use with caution and monitor renal function or consider the use of an alternative analgesic/anti-inflammatory agent (NKF [Henrich 1996]; Whelton 2000). Low-dose aspirin (eg, 75 to 162 mg daily) may be safely used in patients with any degree of renal impairment (KDOQI 2005; KDOQI 2007).
Concurrent drug therapy issues:
- Alteplase: In the treatment of acute ischemic stroke, avoid aspirin for 24 hours following administration of alteplase; administration within 24 hours increases the risk of hemorrhagic transformation (Jauch 2013).
- Cyclooxygenase-2 (COX-2) inhibitors/nonsteroidal anti-inflammatory drugs (NSAIDs): When used concomitantly with ≤325 mg of aspirin, NSAIDs (including selective COX-2 inhibitors) substantially increase the risk of GI complications (eg, ulcer); concomitant gastroprotective therapy (eg, PPIs) is recommended (Bhatt 2008).
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Lower GI bleed patients: An individualized and multidisciplinary approach should be used to manage patients with an acute lower GI bleed (LGIB) who are on antiplatelet medications. Aspirin for primary prevention of cardiovascular events should be avoided in most patients with LGIB who do not have high risk factors for cardiovascular events. However, aspirin for secondary cardiovascular prevention should generally not be discontinued in patients with established cardiovascular disease and a history of lower GI bleeding (Strate 2016).
- Pediatric: When used for self-medication (OTC labeling): Children and teenagers who have or are recovering from chickenpox or flu-like symptoms should not use this product. Changes in behavior (along with nausea and vomiting) may be an early sign of Reye syndrome; patients should be instructed to contact their healthcare provider if these occur.
- Surgical patients: Aspirin should be avoided (if possible) in surgical patients for 1 to 2 weeks prior to elective surgery, to reduce the risk of excessive bleeding. Patients who have recently undergone percutaneous coronary intervention with stenting or balloon angioplasty should continue antiplatelet therapy until it is safe to temporarily hold treatment. Elective surgery for these patients should be delayed. Patient specific situations should be discussed with cardiologist (ACC/AHA [Fleisher 2014]; ACC/AHA [Levine 2016]; AHA/ACC/SCAI/ACS/ADA [Grines 2007]).
Dosage form specific issues:
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer's labeling.
Other warnings/precautions:
- Resistance: Aspirin resistance is defined as measurable, persistent platelet activation that occurs in patients prescribed a therapeutic dose of aspirin. Clinical aspirin resistance, the recurrence of some vascular event despite a regular therapeutic dose of aspirin, is considered aspirin treatment failure. Proposed mechanisms of aspirin resistance include poor adherence with therapy, poor absorption, inadequate dosage, drug interactions, increased isoprostane activity, platelet hypersensitivity to agonists, increased COX-2 activity, COX-1 polymorphism, and platelet alloantigen 2 polymorphism of platelet glycoprotein IIIa. Estimates of biochemical aspirin resistance range from 5.5% to 60% depending on the population studied and the assays used (Gasparyan 2008). Patients with aspirin resistance may have a higher risk of cardiovascular events compared to those who are aspirin sensitive (Gum 2003). Aspirin resistance is likely dose-related but may be influenced by dynamic factors yet to be identified; further research is required.
Pregnancy
Pregnancy Considerations
Salicylate is present in umbilical cord and newborn serum following maternal use of aspirin prior to delivery (Garrettson 1975; Levy 1975; Palmisano 1969); salicylic acid and other metabolites can also be detected in the newborn urine following in utero exposure (Garrettson 1975).
Fetal outcomes are influenced by maternal dose; low dose aspirin (≤150 mg/day) is not associated with the same risks as higher doses and has a positive effect on some pregnancy outcomes (ACOG 743 2018; Turner 2019). Adverse effects reported in the fetus following maternal use of high dose aspirin include mortality, intrauterine growth retardation, salicylate intoxication, bleeding abnormalities, and neonatal acidosis. Use of aspirin close to delivery may cause premature closure of the ductus arteriosus. Adverse effects reported in the mother include anemia, hemorrhage, prolonged gestation, and prolonged labor (Corby 1978; Østensen 1998).
Due to pregnancy-induced physiologic changes, some pharmacokinetic properties of aspirin may be altered (Rymark 1994; Shanmugalingam 2019).
Low-dose aspirin may be used to prevent preeclampsia in women at high risk (history of preeclampsia, multifetal gestation, chronic hypertension, type 1 or type 2 diabetes mellitus, renal disease, autoimmune disease [systemic lupus erythematosus, antiphospholipid syndrome]) (ACOG 203 2019; ACOG 743 2018; ESC [Regitz-Zagrosek 2018]; EULAR [Andreoli 2017]). Use of low-dose aspirin may be considered to prevent preeclampsia in women with moderate risk factors (including but not limited to BMI >30, family history of preeclampsia, maternal age ≥35 years) (ACOG 743 2018). Treatment is started between 12 and 28 weeks' gestation (optimally before 16 weeks' gestation) (ACCP [Bates 2012]; ACOG 743 2018; LeFevre 2014). Low-dose aspirin to prevent thrombosis may also be used during the second and third trimesters in women with prosthetic valves (mechanical or bioprosthetic). The use of warfarin is recommended throughout pregnancy, along with low-dose aspirin during second and third trimesters, in patients with mechanical prosthetic valves (AHA/ACC [Nishimura 2014]). Low-dose aspirin may also be used after the first trimester in women with low-risk conditions requiring antiplatelet therapy (AHA/ASA [Kernan 2014]). When needed in doses required for the management of pain, agents other than aspirin are preferred in pregnant women and use in the third trimester is not recommended (Källén 2016; Shah 2015).
Patient Education
What is this drug used for?
- It is used to treat rheumatic fever.
- It is used to ease pain and fever.
- It is used to treat some types of arthritis.
- It is used to protect bypass grafts and stents in the heart.
- It is used to lower the chance of heart attack, stroke, and death in some people.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Abdominal pain
- Heartburn
- Vomiting
- Nausea
- Rectal irritation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Abdominal ulcers like severe abdominal or back pain; black, tarry, or bloody stools; vomiting blood or vomit that looks like coffee grounds; or weight gain or abnormal swelling
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- High potassium like abnormal heartbeat, confusion, dizziness, passing out, weakness, shortness of breath, or numbness or tingling feeling
- Acidosis like confusion, fast breathing, fast heartbeat, abnormal heartbeat, severe abdominal pain, nausea, vomiting, fatigue, shortness of breath, or loss of strength and energy
- Severe cerebrovascular disease like change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes
- Severe dizziness
- Passing out
- Severe headache
- Noise or ringing in the ears
- Trouble hearing
- Agitation
- Seizures
- Severe rectal pain
- Rectal bleeding
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.