Boxed Warning
Serious dermatologic reactions and HLA-B*1502 allele:
Serious and sometimes fatal dermatologic reactions, including toxic epidermal necrolysis (TEN) and Stevens-Johnson syndrome, have been reported during treatment with carbamazepine. These reactions are estimated to occur in 1 to 6 per 10,000 new users in countries with mainly Caucasian populations, but the risk in some Asian countries is estimated to be about 10 times higher. Studies in patients of Chinese ancestry have found a strong association between the risk of developing Stevens-Johnson syndrome/TEN and the presence of HLA-B*1502, an inherited allelic variant of the HLA-B gene. HLA-B*1502 is found almost exclusively in patients with ancestry across broad areas of Asia. Patients with ancestry in genetically at-risk populations should be screened for the presence of HLA-B*1502 prior to initiating treatment with carbamazepine. Patients testing positive for the allele should not be treated with carbamazepine unless the benefit clearly outweighs the risk.
Aplastic anemia and agranulocytosis:
Aplastic anemia and agranulocytosis have been reported in association with the use of carbamazepine. Data from a population-based case-control study demonstrate that the risk of developing these reactions is 5 to 8 times greater than in the general population. However, the overall risk of these reactions in the untreated general population is low, approximately 6 patients per 1 million population per year for agranulocytosis and 2 patients per 1 million population per year for aplastic anemia.
Although reports of transient or persistent decreased platelet or white blood cell counts (WBCs) are not uncommon in association with the use of carbamazepine, data are not available to accurately estimate their incidence or outcome. However, the vast majority of the cases of leukopenia have not progressed to the more serious conditions of aplastic anemia or agranulocytosis.
Because of the very low incidence of agranulocytosis and aplastic anemia, the vast majority of minor hematological changes observed in monitoring of patients on carbamazepine are unlikely to signal the occurrence of either abnormality. Nonetheless, complete pretreatment hematological testing should be obtained as a baseline. If a patient in the course of treatment exhibits low or decreased white blood cell or platelet counts, the patient should be monitored closely. Discontinuation of the drug should be considered if any evidence of significant bone marrow depression develops.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule Extended Release 12 Hour, Oral:
Carbatrol: 100 mg [contains fd&c blue #2 (indigotine)]
Carbatrol: 200 mg, 300 mg
Equetro: 100 mg, 200 mg, 300 mg [contains fd&c blue #2 (indigotine)]
Generic: 100 mg, 200 mg, 300 mg
Suspension, Oral:
TEGretol: 100 mg/5 mL (450 mL) [contains fd&c yellow #6 (sunset yellow), propylene glycol; citrus-vanilla flavor]
Generic: 100 mg/5 mL (450 mL)
Tablet, Oral:
Epitol: 200 mg [scored]
TEGretol: 200 mg [scored; contains fd&c red #40]
Generic: 200 mg
Tablet Chewable, Oral:
Generic: 100 mg
Tablet Extended Release 12 Hour, Oral:
TEGretol-XR: 100 mg, 200 mg, 400 mg
Generic: 100 mg, 200 mg, 400 mg
Pharmacology
Mechanism of Action
In addition to anticonvulsant effects, carbamazepine has anticholinergic, antineuralgic, antidiuretic, muscle relaxant, antimanic, antidepressive, and antiarrhythmic properties; may depress activity in the nucleus ventralis of the thalamus or decrease synaptic transmission or decrease summation of temporal stimulation leading to neural discharge by limiting influx of sodium ions across cell membrane or other unknown mechanisms; stimulates the release of ADH and potentiates its action in promoting reabsorption of water; chemically related to tricyclic antidepressants
Pharmacokinetics/Pharmacodynamics
Absorption
Slowly from the GI tract
Distribution
Vd: Neonates: 1.52 ± 0.5 L/kg (Rey 1979); Children: 1.94 ± 0.8 L/kg (Rey 1979); Adults: 0.59 to 2 L/kg
Metabolism
Induces liver enzymes to increase metabolism and shorten half-life over time; metabolized in the liver by cytochrome P450 3A4 to active epoxide metabolite; epoxide metabolite is metabolized by epoxide hydrolase to the trans-diol metabolite; ratio of serum epoxide to carbamazepine concentrations may be higher in patients receiving polytherapy (vs monotherapy) and in infants (vs older children); boys may have faster carbamazepine clearances and may, therefore, require higher mg/kg/day doses of carbamazepine compared to girls of similar age and weight
Excretion
Urine 72% (1% to 3% as unchanged drug); feces (28%)
Time to Peak
Unpredictable:
Immediate release: Suspension: Multiple doses: 1.5 hour; tablet: 4 to 5 hours
Extended release: Carbatrol, Equetro: 12 to 26 hours (single dose), 4 to 8 hours (multiple doses); Tegretol®-XR: 3 to 12 hours
Half-Life Elimination
Half-life is variable because of autoinduction which is usually complete 3 to 5 weeks after initiation of a fixed carbamazepine regimen.
Carbamazepine: Initial: 25 to 65 hours; Extended release: 35 to 40 hours; Multiple doses: Children and Adolescents: Mean range: 3.1 to 20.8 hours (Battino 1995); Adults: 12 to 17 hours
Epoxide metabolite: Initial: 34 ± 9 hours
Protein Binding
Carbamazepine: 75% to 90%, bound to alpha1-acid glycoprotein and nonspecific binding sites on albumin; may be decreased in newborns; Epoxide metabolite: 50%
Use: Labeled Indications
Bipolar disorder: Monotherapy in the acute treatment of hypomania and mild to moderate manic or mixed episodes associated with bipolar disorder
Focal (partial) onset seizures and generalized onset seizures: Monotherapy and adjunctive therapy in the treatment of patients with focal onset seizures and generalized onset seizures
Limitations of use: Carbamazepine is not indicated for the treatment of nonmotor (absence) seizures; it has been associated with increased frequency of generalized convulsions in these patients.
Neuropathic pain: Treatment of trigeminal or glossopharyngeal neuralgia
Use: Off Label
Bipolar major depressioncyes
Data from a double-blind, randomized, placebo-controlled trial suggest that carbamazepine monotherapy may decrease time to response for patients with bipolar major depression Zhang 2007.
Based on the Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) guidelines for the management of patients with bipolar disorder, carbamazepine is recommended as an alternative to preferred agents for patients with bipolar major depression CANMAT [Yatham 2018].
Maintenance treatment for bipolar disordercyes
Data from a randomized, controlled trial suggest that carbamazepine may prevent hospitalization caused by a mood episode in patients with bipolar disorder, particularly those with type II bipolar disorder Kleindienst 2000.
Based on the CANMAT and ISBD guidelines for the management of patients with bipolar disorder and the British Association for Psychopharmacology evidence-based guidelines for treating bipolar disorder, carbamazepine is recommended as an alternative to preferred agents for maintenance treatment of bipolar disorder BAP [Goodwin 2016], CANMAT [Yatham 2018].
Contraindications
Hypersensitivity to carbamazepine, tricyclic antidepressants, or any component of the formulation; bone marrow depression; with or within 14 days of MAO inhibitor use; concomitant use of nefazodone, delavirdine, or other non-nucleoside reverse transcriptase inhibitors that are substrate of CYP3A4.
Canadian labeling: Additional contraindications (not in US labeling): Atrioventricular (AV) heart block; hepatic disease; history of hepatic porphyria (acute intermittent porphyria, variegate porphyria, porphyria cutanea tarda); serious blood disorder; concurrent use with itraconazole and voriconazole.
Dosage and Administration
Dosing: Adult
Note: Safety: Before prescribing carbamazepine, test for HLA-B*1502 allele in patients at increased risk of developing serious cutaneous adverse reactions (SCAR) (ie, those of Asian ancestry, including South Asian Indians). A negative HLA-B*1502 genetic test does not entirely rule out the possibility of SCAR, so patients should still be monitored for cutaneous reactions and other forms of hypersensitivity (Leckband 2013). Although other alleles (eg, HLA-A*3101, HLA-A*24:02) may also increase the risk of hypersensitivity in a broader range of ethnic groups, testing recommendations are not well established (Amstutz 2014; Schachter 2019a; Shi 2017). Therapeutic drug monitoring: May be useful, particularly in patients with seizure disorder; monitor more closely during the first few months of therapy because carbamazepine induces hepatic enzymes, thereby increasing its own metabolism, which may lead to a decrease in serum levels after ~2 to 3 months and require subsequent dosage adjustment(s). Dosage forms: Dosing recommendations are expressed as the total daily dose (ie, per 24 hours) unless stated otherwise. Total daily oral dose is given in 2 to 4 divided doses per day depending on the type of preparation. Available oral preparations include: Immediate release (suspension, tablet, chewable tablet) (usually dosed 2 to 4 times daily) and 12-hour extended release (dosed twice daily).
Bipolar disorder, hypomania and mild to moderate manic or mixed episodes (alternative agent) and bipolar major depression (alternative agent) (BAP [Goodwin 2016]; Shelton 2019):
Acute treatment (monotherapy): Oral: Initial: 100 to 400 mg/day; may increase dose based on response and tolerability in increments of 200 mg/day every 1 to 4 days; usual dose range: 600 mg/day to 1.2 g/day; maximum dose: 1.6 g/day (Stovall 2019; WFSBP [Grunze 2009]; manufacturer's labeling). Doses up to 1.8 g/day may be necessary in some patients for optimal response (Stoval 2019).
Maintenance (monotherapy) (off-label use): Oral: Continue dose that was used to achieve control of the acute episode (Peselow 2016).
Focal (partial) onset seizures and generalized onset seizures (monotherapy or adjunctivetherapy): Note: Avoid use in nonmotor (absence) seizures.
Oral: Initial 2 to 3 mg/kg/day (100 to 200 mg/day) or up to 400 mg/day (according to manufacturer's labeling), which may not be as well tolerated; may gradually increase dose based on seizure control, tolerability, and serum concentrations every ≥5 days in increments of ≤200 mg/day to a usual maintenance dose of ~10 mg/kg/day (800 mg/day to 1.2 g/day). After 2 to 3 months of treatment, serum concentrations may decrease due to hepatic enzyme autoinduction and dose may need to be further increased to 15 to 20 mg/kg/day; doses up to ~2 g/day may be needed in some patients for optimal effect (Schachter 2019a).
Neuropathic pain: Note: For use in trigeminal or glossopharyngeal neuralgia (Rosenquist 2019). May also be used in critically ill patients with neuropathic pain as a component of multimodal pain control (alternative agent) (Pandey 2005; SCCM [Devlin 2018]).
Oral: Initial: 200 to 400 mg/day, gradually increasing (eg, over several weeks) in increments of 200 mg/day as needed. Usual maintenance dose: 600 to 800 mg/day; maximum dose: 1.2 g/day (Bajwa 2019; manufacturer's labeling).
Discontinuation of therapy: In chronic therapy, withdraw gradually over 2 to 6 months to minimize the potential of increased seizure frequency (in patients with epilepsy) and other withdrawal symptoms (eg, dysphoria, hallucinations, headache, insomnia, tremor) unless safety concerns require more rapid withdrawal (Chen 2014; Medical Research Council Antiepileptic Drug Withdrawal Study Group 1991; Schachter 2019b). In patients discontinuing therapy for treatment of bipolar disorder, close monitoring for several weeks to months for reemergence of mania/hypomania is recommended (Post 2019).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Prior to initiating carbamazepine therapy, test for HLA-B*15:02 allele in patients with increased risk for this genetic variant (eg, Han Chinese, Thai, Malaysian, Indian, or Vietnamese descent); this is associated with a significantly increased risk of Stevens-Johnson syndrome and/or toxic epidermal necrolysis; do NOT initiate in patients with a positive result (Amstutz 2014; Leckband 2013). Although testing recommendations are not well established, consider testing for HLA-A*31:01 and HLA-A*24:02 allele. These alleles are found in a broader range of ethnic groups and also increase the risk for hypersensitivity reactions (Leckband 2013; Shi 2017). A negative genetic test does not entirely rule out the possibility of a hypersensitivity or cutaneous reaction, and patients should be monitored throughout therapy.
Seizure disorder: Dosage must be adjusted according to patient's response and serum concentrations.
Oral:
Infants and Children <6 years:
Immediate-release formulations:
Tablets: Initial: 10 to 20 mg/kg/day in divided doses twice or 3 times daily; titrate at weekly intervals until optimal response; maintenance doses administered 3 or 4 times daily; maximum daily dose: 35 mg/kg/day.
Suspension: Initial: 10 to 20 mg/kg/day in divided doses 4 times daily; titrate at weekly intervals until optimal response; maintenance doses administered 3 or 4 times daily; maximum daily dose: 35 mg/kg/day.
Children ≥6 to 12 years:
Immediate-release formulations:
Tablets: Initial: 100 mg twice daily, titrate by up to 100 mg/day at weekly intervals. Usual maintenance dose range: 400 to 800 mg/day in 3 to 4 divided doses. Maximum daily dose: 1,000 mg/day.
Suspension: Initial: 50 mg 4 times daily, titrate by up to 100 mg/day at weekly intervals. Usual maintenance daily dose range: 400 to 800 mg/day in 3 to 4 divided doses. Maximum daily dose: 1,000 mg/day.
Extended-release formulations: Capsules, tablets: Initial: 100 mg twice daily, titrate by up to 100 mg/day at weekly intervals. Usual maintenance daily dose range: 400 to 800 mg/day in divided doses twice daily. Maximum daily dose: 1,000 mg/day.
Adolescents:
Immediate-release formulations:
Tablets: Initial: 200 mg twice daily, titrate by up to 200 mg/day increments at weekly intervals. Usual maintenance daily dose range: 800 to 1,200 mg/day in divided doses 3 or 4 times daily.
Suspension: Initial: 100 mg 4 times daily, titrate by up to 200 mg/day increments at weekly intervals. Usual maintenance daily dose range: 800 to 1,200 mg/day in divided doses 3 or 4 times daily.
Extended-release formulations: Capsule, tablet: Initial: 200 mg twice daily, titrate by up to 200 mg/day increments at weekly intervals. Usual maintenance daily dose range: 800 to 1,200 mg/day in divided doses twice daily.
Maximum daily doses:
Adolescents ≤15 years: 1,000 mg/day.
Adolescents >15 years: 1,200 mg/day.
Rectal: Limited data available: Infants, Children, and Adolescents: Maintenance dose: Administer the same total daily dose as small, diluted doses administered more frequently than the oral; dilute the oral suspension with an equal volume of water; if defecation occurs within the first 2 hours, repeat the dose (Graves 1987).
Dosing conversions: Close monitoring and possible dosage adjustment may be necessary during any dosage form conversions due to pharmacokinetics differences amongst immediate-release dosage forms (ie, suspension formulation produces higher peak concentrations compared to the tablet) and between the immediate- and extended-release formulations.
Conversion from immediate-release solid dosage form to suspension: Use the same daily dose and divide into 3 daily doses; monitor serum concentrations.
Conversion from immediate-release tablets to extended-release formulations: Use the same daily dose and divide into 2 daily doses; monitor serum concentrations.
Discontinuation of therapy: Discontinuation of treatment for epilepsy is dependent on several factors to minimize chance of seizure relapse. Favorable factors include: Childhood onset, normal EEG at time of discontinuation, idiopathic generalized epilepsy, low seizure frequency before and during treatment, seizure type, normal neurologic exam, and normal intellectual development. Withdrawal of therapy is typically evaluated if patient has been seizure free for 2 years. Abrupt discontinuation is not recommended. Gradual tapers have ranged from 6 weeks to 9 months. The slow discontinuation should be tailored to the patient's preference and needs. Other considerations include the drug pharmacokinetic properties, dosage at the start of withdrawal, dosage forms, and need for follow-up serum concentration monitoring (Beghi 2013; Specchio 2004; Strozzi 2015).
Extemporaneously Prepared
Note: Commercial oral suspension is available (20 mg/mL)
40 mg/mL Oral Suspension
A 40 mg/mL oral suspension may be made with tablets. Crush twenty 200 mg tablets in a mortar and reduce to a fine powder. Add small portions of Simple Syrup, NF and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 100 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add sufficient quantity of vehicle to make 100 mL. Label "shake well" and "refrigerate". Stable for 90 days.
Nahata MC, Pai VB, and Hipple TF, Pediatric Drug Formulations, 5th ed, Cincinnati, OH: Harvey Whitney Books Co, 2004.
Administration
Oral:
Chewable or immediate-release tablets: Administer with food
Suspension: Shake well before administration. Must be given on a 3 to 4 times/day schedule versus tablets, which can be given 2 to 4 times/day. Because a given dose of suspension will produce higher peak and lower trough levels than the same dose given as the tablet form, patients given the suspension should be started on lower doses given more frequently (same total daily dose) and increased slowly to avoid unwanted side effects. When carbamazepine suspension has been combined with chlorpromazine or thioridazine solutions, a precipitate forms, which may result in loss of effect. Therefore, it is recommended that the carbamazepine suspension dosage form not be administered at the same time with other liquid medicinal agents or diluents. Should be administered with meals.
Extended-release capsule (Carbatrol, Equetro): Consists of three different types of beads: immediate release, extended release, and enteric release. The bead types are combined in a ratio to allow twice daily dosing. May be opened and contents sprinkled over food such as a teaspoon of applesauce; may be administered with or without food; do not crush or chew capsule or beads inside capsule.
Extended-release tablet: Should be inspected for damage. Damaged extended-release tablets (without release portal) should not be administered. Should be administered with meals; swallow whole, do not crush or chew.
Dietary Considerations
Folate and vitamin B: Carbamazepine use has been associated with low serum concentrations of folate, vitamin B2 (riboflavin), B6 (pyridoxine) and B12 (cyanocobalamin), which may contribute to hyperhomocysteinemia. Hyperhomocysteinemia may contribute to cardiovascular disease, venous thromboembolic disease, dementia, neuropsychiatric symptoms, and poor seizure control. Some health care providers recommend administering folic acid, riboflavin, pyridoxine, and cyanocobalamin supplements in patients taking carbamazepine (Apeland 2003; Apeland 2008; Belcastro 2012; Bochyńska 2012).
Storage
Carbatrol, Equetro: Store at controlled room temperature (25°C [77°F]); excursions permitted to 15°C to 30°C (59°F to 86°F); protect from light and moisture.
Tegretol-XR: Store at controlled room temperature, 15°C to 30°C (59°F to 86°F); protect from moisture.
Tegretol tablets and chewable tablets: Store at ≤30°C (86°F); protect from light and moisture.
Tegretol suspension: Store at ≤30°C (86°F); shake well before using.
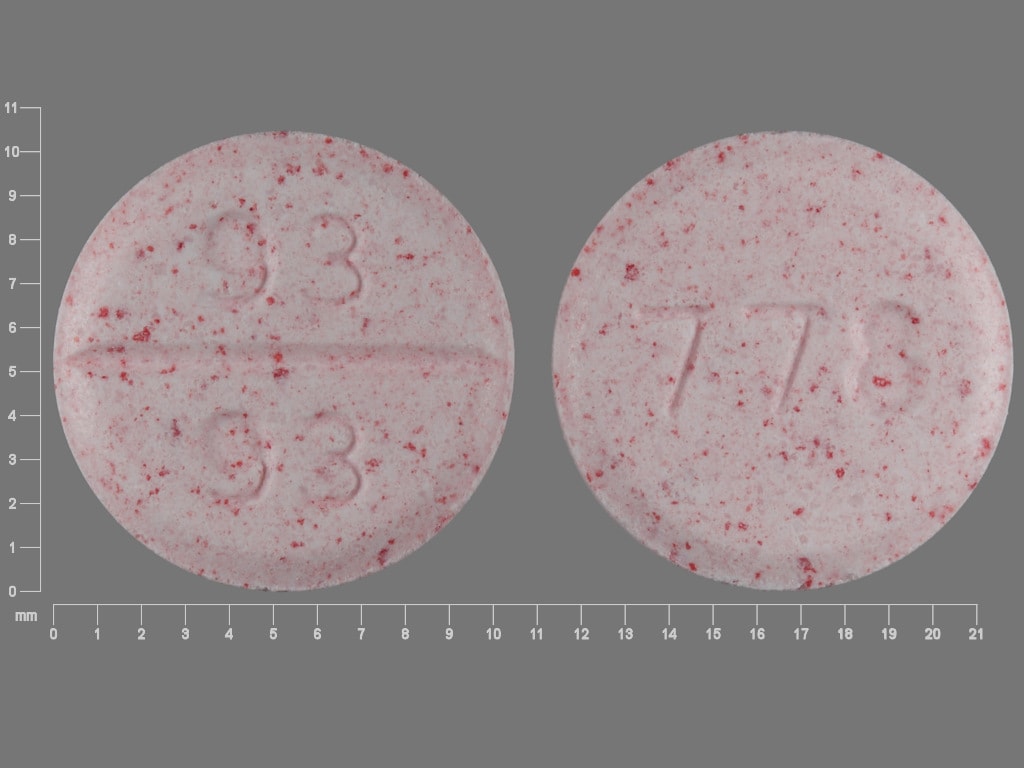
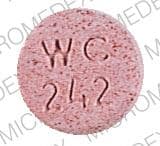
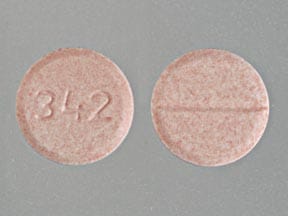
CarBAMazepine Images
Drug Interactions
Abemaciclib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Abemaciclib. Avoid combination
Abiraterone Acetate: CYP3A4 Inducers (Strong) may decrease the serum concentration of Abiraterone Acetate. Management: Avoid whenever possible. If such a combination cannot be avoided, increase abiraterone acetate dosing frequency from once daily to twice daily during concomitant use. Consider therapy modification
Acalabrutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Acalabrutinib. Management: Avoid co-administration of strong CYP3A inducers in patients taking acalabrutinib. If strong CYP3A inducers cannot be avoided, increase the dose of acalabrutinib to 200 mg twice daily. Consider therapy modification
Acetaminophen: CarBAMazepine may increase the metabolism of Acetaminophen. This may 1) diminish the effect of acetaminophen; and 2) increase the risk of liver damage. Monitor therapy
Adenosine: CarBAMazepine may enhance the adverse/toxic effect of Adenosine. Specifically, the risk of higher degree heart block may be increased. Management: Consider using a lower initial dose of adenosine in patients who are receiving carbamazepine. Consider therapy modification
Afatinib: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Afatinib. Management: Per US labeling: if requiring chronic use of P-gp inducers, increase afatinib dose by 10 mg as tolerated; reduce to original afatinib dose 2-3 days after stopping P-gp inducers. Per Canadian labeling: avoid combination if possible. Consider therapy modification
Albendazole: CarBAMazepine may decrease serum concentrations of the active metabolite(s) of Albendazole. Monitor therapy
Allopurinol: May increase the serum concentration of CarBAMazepine. Monitor therapy
Alpelisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Alpelisib. Avoid combination
Antihepaciviral Combination Products: CYP3A4 Inducers (Strong) may decrease the serum concentration of Antihepaciviral Combination Products. Avoid combination
Apalutamide: CYP3A4 Inducers (Strong) may decrease the serum concentration of Apalutamide. Monitor therapy
Apixaban: Inducers of CYP3A4 (Strong) and P-glycoprotein may decrease the serum concentration of Apixaban. Avoid combination
Apremilast: CYP3A4 Inducers (Strong) may decrease the serum concentration of Apremilast. Avoid combination
Aprepitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Aprepitant. Avoid combination
ARIPiprazole: CYP3A4 Inducers (Strong) may decrease the serum concentration of ARIPiprazole. Management: Double the oral aripiprazole dose and closely monitor. Reduce oral aripiprazole dose to 10-15 mg/day (for adults) if the inducer is discontinued. Avoid use of strong CYP3A4 inducers for more than 14 days with extended-release injectable aripiprazole. Consider therapy modification
ARIPiprazole Lauroxil: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of ARIPiprazole Lauroxil. Management: Patients taking the 441 mg dose of aripiprazole lauroxil increase their dose to 662 mg if used with a strong CYP3A4 inducer for more than 14 days. No dose adjustment is necessary for patients using the higher doses of aripiprazole lauroxil. Consider therapy modification
Artemether: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Artemether. Specifically, dihydroartemisinin concentrations may be reduced. CYP3A4 Inducers (Strong) may decrease the serum concentration of Artemether. Avoid combination
Asunaprevir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Asunaprevir. Avoid combination
Avapritinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Avapritinib. Avoid combination
Axitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Axitinib. Avoid combination
Bazedoxifene: CarBAMazepine may decrease the serum concentration of Bazedoxifene. This may lead to loss of efficacy or, if bazedoxifene is combined with estrogen therapy, an increased risk of endometrial hyperplasia. Monitor therapy
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bedaquiline: CYP3A4 Inducers (Strong) may decrease the serum concentration of Bedaquiline. Avoid combination
Benperidol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Benperidol. Monitor therapy
Benzhydrocodone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Benzhydrocodone. Specifically, the serum concentrations of hydrocodone may be reduced. Monitor therapy
Betrixaban: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Betrixaban. Avoid combination
Bictegravir: CarBAMazepine may decrease the serum concentration of Bictegravir. Management: When possible consider using an alternative anticonvulsant with concurrent bictegravir, emtricitabine, and tenofovir alafenamide. If the combination must be used, monitor closely for evidence of reduced antiviral effectiveness. Consider therapy modification
Bortezomib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Bortezomib. Avoid combination
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Bosutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Bosutinib. Avoid combination
Brentuximab Vedotin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be decreased. Monitor therapy
Brentuximab Vedotin: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be decreased. Monitor therapy
Brexpiprazole: CYP3A4 Inducers (Strong) may decrease the serum concentration of Brexpiprazole. Management: If brexpiprazole is used together with a strong CYP3A4 inducer, the brexpiprazole dose should gradually be doubled over the course of 1 to 2 weeks. Consider therapy modification
Brigatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Brigatinib. Avoid combination
Brivaracetam: May increase serum concentrations of the active metabolite(s) of CarBAMazepine. CarBAMazepine may decrease the serum concentration of Brivaracetam. Monitor therapy
Bromperidol: CarBAMazepine may decrease the serum concentration of Bromperidol. Monitor therapy
Buprenorphine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Buprenorphine. Monitor therapy
BusPIRone: CYP3A4 Inducers (Strong) may decrease the serum concentration of BusPIRone. Management: Consider alternatives to this combination. If coadministration of these agents is deemed necessary, monitor patients for reduced buspirone effects and increase buspirone doses as needed. Consider therapy modification
Cabozantinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cabozantinib. Management: Avoid use of strong CYP3A4 inducers with cabozantinib if possible. If combined, cabozantinib dose adjustments are recommended and vary based on the cabozantinib product used and the indication for use. See monograph for details. Consider therapy modification
Calcifediol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Calcifediol. Monitor therapy
Calcium Channel Blockers (Dihydropyridine): CarBAMazepine may increase the metabolism of Calcium Channel Blockers (Dihydropyridine). Management: Consider calcium channel blocker (CCB) dose adjustments or alternative therapy in patients receiving concomitant carbamazepine. Nimodipine Canadian labeling contraindicates concurrent use with carbamazepine. Exceptions: Clevidipine. Consider therapy modification
Calcium Channel Blockers (Nondihydropyridine): May increase the serum concentration of CarBAMazepine. CarBAMazepine may decrease the serum concentration of Calcium Channel Blockers (Nondihydropyridine). Management: Consider empiric reductions in carbamazepine dose with initiation of nondihydropyridine calcium channel blockers. Monitor for increased toxic effects of carbamazepine and reduced therapeutic effects of the calcium channel blocker. Consider therapy modification
Cannabidiol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cannabidiol. Monitor therapy
Cannabis: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cannabis. More specifically, tetrahydrocannabinol and cannabidiol serum concentrations may be decreased. Monitor therapy
Carbonic Anhydrase Inhibitors: May increase the serum concentration of CarBAMazepine. Exceptions: Brinzolamide; Dorzolamide. Monitor therapy
Cariprazine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cariprazine. Avoid combination
Caspofungin: Inducers of Drug Clearance may decrease the serum concentration of Caspofungin. Management: Consider using an increased caspofungin dose of 70 mg daily in adults (or 70 mg/m2, up to a maximum of 70 mg, daily in pediatric patients) when coadministered with known inducers of drug clearance. Consider therapy modification
Celiprolol: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Celiprolol. Monitor therapy
Cenobamate: May decrease the serum concentration of CarBAMazepine. Monitor therapy
Ceritinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ceritinib. Avoid combination
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Chlormethiazole: CarBAMazepine may decrease the serum concentration of Chlormethiazole. Monitor therapy
ChlorproPAMIDE: CYP3A4 Inducers (Strong) may decrease the serum concentration of ChlorproPAMIDE. Monitor therapy
Cimetidine: May increase the serum concentration of CarBAMazepine. The serum carbamazepine concentration might return to normal within one week of starting cimetidine. Monitor therapy
Ciprofloxacin (Systemic): May increase the serum concentration of CarBAMazepine. Monitor therapy
Citalopram: CarBAMazepine may decrease the serum concentration of Citalopram. Monitor therapy
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
Clarithromycin: CarBAMazepine may increase serum concentrations of the active metabolite(s) of Clarithromycin. Clarithromycin may increase the serum concentration of CarBAMazepine. CarBAMazepine may decrease the serum concentration of Clarithromycin. Management: Consider alternatives to this combination when possible. If combined, monitor for increased carbamazepine effects/toxicities and for reduced clarithromycin efficacy. Consider therapy modification
Clindamycin (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Clindamycin (Systemic). Refer to the specific clindamycin (systemic) - rifampin drug interaction monograph for information concerning that combination. Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
ClomiPRAMINE: CarBAMazepine may decrease the serum concentration of ClomiPRAMINE. Monitor therapy
CloZAPine: CarBAMazepine may enhance the myelosuppressive effect of CloZAPine. More specifically, the risk of bone marrow suppression with this combination may be increased due to the independent myelosuppressive effects of the drugs. CarBAMazepine may decrease the serum concentration of CloZAPine. Avoid combination
Cobicistat: CarBAMazepine may decrease the serum concentration of Cobicistat. Avoid combination
Cobimetinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cobimetinib. Avoid combination
Codeine: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Codeine. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Copanlisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Copanlisib. Avoid combination
Corticosteroids (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Corticosteroids (Systemic). Exceptions: Hydrocortisone (Systemic); PrednisoLONE (Systemic); PredniSONE. Monitor therapy
Crizotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Crizotinib. Avoid combination
CycloSPORINE (Systemic): CarBAMazepine may decrease the serum concentration of CycloSPORINE (Systemic). Management: Monitor frequently for decreased serum concentrations and therapeutic effects of cyclosporine if combined with carbamazepine. Increased cyclosporine doses will likely be needed to maintain adequate serum concentrations. Consider therapy modification
CYP2B6 Substrates (High risk with Inducers): CYP2B6 Inducers (Moderate) may decrease the serum concentration of CYP2B6 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of CarBAMazepine. Monitor therapy
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
CYP3A4 Substrates (High risk with Inducers): CYP3A4 Inducers (Strong) may increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Exceptions: Benzhydrocodone; Buprenorphine; CarBAMazepine; Etizolam; HYDROcodone; Mirtazapine; TraMADol; Zolpidem. Consider therapy modification
Dabigatran Etexilate: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Dabigatran Etexilate. Management: Avoid concurrent use of dabigatran with P-glycoprotein inducers whenever possible. Avoid combination
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Daclatasvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Daclatasvir. Avoid combination
Danazol: May decrease the metabolism of CarBAMazepine. Monitor therapy
Darolutamide: Inducers of CYP3A4 (Strong) and P-glycoprotein may decrease the serum concentration of Darolutamide. Avoid combination
Darunavir: May increase the serum concentration of CarBAMazepine. Monitor therapy
Dasabuvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dasabuvir. Avoid combination
Dasatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dasatinib. Management: Avoid when possible. If such a combination cannot be avoided, consider increasing dasatinib dose and monitor clinical response and toxicity closely. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Deflazacort: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Deflazacort. Avoid combination
Delamanid: CYP3A4 Inducers (Strong) may decrease the serum concentration of Delamanid. Avoid combination
Delavirdine: CarBAMazepine may decrease the serum concentration of Delavirdine. Avoid combination
Desmopressin: CarBAMazepine may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
DexAMETHasone (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of DexAMETHasone (Systemic). Management: Consider dexamethasone dose increases in patients receiving strong CYP3A4 inducers and monitor closely for reduced dexamethasone efficacy. Consider avoiding this combination when treating life threatening conditions (ie, multiple myeloma). Consider therapy modification
Dienogest: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dienogest. Management: Avoid use of dienogest for contraception when using medications that induce CYP3A4 and for at least 28 days after discontinuation of a CYP3A4 inducer. An alternative form of contraception should be used during this time. Avoid combination
Diethylstilbestrol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Diethylstilbestrol. Monitor therapy
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Dolutegravir: CarBAMazepine may decrease the serum concentration of Dolutegravir. Management: Increase dolutegravir dose to 50 mg twice daily when used together with carbamazepine. Patients with known or suspected integrase strand inhibitor resistance should use an alternative to carbamazepine when possible. Consider therapy modification
Doravirine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Doravirine. Avoid combination
Doxercalciferol: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Doxercalciferol. Monitor therapy
DOXOrubicin (Conventional): CYP3A4 Inducers (Strong) may decrease the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to strong CYP3A4 inducers in patients treated with doxorubicin. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
DOXOrubicin (Conventional): P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to P-glycoprotein inducers in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Doxycycline: CarBAMazepine may decrease the serum concentration of Doxycycline. Consider therapy modification
Dronabinol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dronabinol. Monitor therapy
Dronedarone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dronedarone. Avoid combination
Duvelisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Duvelisib. Avoid combination
Edoxaban: CarBAMazepine may decrease the serum concentration of Edoxaban. Management: Combined use of carbamazepine and edoxaban should generally be avoided. Consider therapy modification
Efavirenz: CarBAMazepine may decrease the serum concentration of Efavirenz. Efavirenz may decrease the serum concentration of CarBAMazepine. Avoid combination
Elagolix: CYP3A4 Inducers (Strong) may decrease the serum concentration of Elagolix. Monitor therapy
Elbasvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Elbasvir. Avoid combination
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Avoid combination
Eliglustat: CYP3A4 Inducers (Strong) may decrease the serum concentration of Eliglustat. Avoid combination
Elvitegravir: CarBAMazepine may decrease the serum concentration of Elvitegravir. Avoid combination
Encorafenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Encorafenib. Avoid combination
Enfortumab Vedotin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Enfortumab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be decreased. Monitor therapy
Entrectinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Entrectinib. Avoid combination
Enzalutamide: CYP3A4 Inducers (Strong) may decrease the serum concentration of Enzalutamide. Management: Consider using an alternative agent that has no or minimal CYP3A4 induction potential when possible. If this combination cannot be avoided, increase the dose of enzalutamide from 160 mg daily to 240 mg daily. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Eravacycline: CYP3A4 Inducers (Strong) may decrease the serum concentration of Eravacycline. Management: Increase the eravacycline dose to 1.5 mg/kg every 12 hours when combined with strong CYP3A4 inducers. Consider therapy modification
Erdafitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Erdafitinib. Avoid combination
Erlotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Erlotinib. Management: Avoid combination if possible. If combination must be used, increase erlotinib dose by 50 mg increments every 2 weeks as tolerated, to a maximum of 450 mg/day. Consider therapy modification
Erythromycin (Systemic): May increase the serum concentration of CarBAMazepine. Management: Consider alternative antimicrobial therapy in combination with carbamazepine. If combined, monitor for increased carbamazepine effects/toxicities. Consider therapy modification
Eslicarbazepine: CarBAMazepine may enhance the adverse/toxic effect of Eslicarbazepine. CarBAMazepine may decrease the serum concentration of Eslicarbazepine. Monitor therapy
Estriol (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Estriol (Systemic). Monitor therapy
Estriol (Topical): CYP3A4 Inducers (Strong) may decrease the serum concentration of Estriol (Topical). Monitor therapy
Estrogen Derivatives (Contraceptive): CarBAMazepine may diminish the therapeutic effect of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of a nonhormonal contraceptive is recommended. Consider therapy modification
Etizolam: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etizolam. Monitor therapy
Etoposide: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etoposide. Management: When possible, seek alternatives to strong CYP3A4-inducing medications in patients receiving etoposide. If combined, monitor patients closely for diminished etoposide response and need for etoposide dose increases. Consider therapy modification
Etoposide Phosphate: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etoposide Phosphate. Management: When possible, seek alternatives to strong CYP3A4-inducing medications in patients receiving etoposide phosphate. If these combinations cannot be avoided, monitor patients closely for diminished etoposide phosphate response. Consider therapy modification
Etravirine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etravirine. Avoid combination
Everolimus: CYP3A4 Inducers (Strong) may decrease the serum concentration of Everolimus. Management: Avoid concurrent use of strong CYP3A4 inducers if possible. If coadministration cannot be avoided, double the daily dose of everolimus using increments of 5 mg or less. Monitor everolimus serum concentrations closely when indicated. Consider therapy modification
Evogliptin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Evogliptin. Monitor therapy
Exemestane: CYP3A4 Inducers (Strong) may decrease the serum concentration of Exemestane. Management: Exemestane U.S. product labeling recommends using an increased dose (50 mg/day) in patients receiving concurrent strong CYP3A4 inducers. The Canadian product labeling does not recommend a dose adjustment with concurrent use of strong CYP3A4 inducers. Consider therapy modification
Ezogabine: CarBAMazepine may decrease the serum concentration of Ezogabine. Management: Consider increasing the ezogabine dose when adding carbamazepine. Monitor patients using the combination closely for evidence of adequate ezogabine therapy. Consider therapy modification
Fedratinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Fedratinib. Avoid combination
Felbamate: CarBAMazepine may decrease the serum concentration of Felbamate. Felbamate may decrease the serum concentration of CarBAMazepine. Management: In patients receiving carbamazepine, initiate felbamate at 1200 mg/day in divided doses 3-4 times daily while reducing carbamazepine dose by 20%. Monitor for reduced concentrations/effects of both drugs. Consider therapy modification
FentaNYL: CYP3A4 Inducers (Strong) may decrease the serum concentration of FentaNYL. Monitor therapy
Fingolimod: CarBAMazepine may decrease the serum concentration of Fingolimod. Monitor therapy
Flibanserin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Flibanserin. Avoid combination
Fluconazole: May increase the serum concentration of CarBAMazepine. Monitor therapy
Flunarizine: CarBAMazepine may decrease the serum concentration of Flunarizine. Monitor therapy
FLUoxetine: May increase the serum concentration of CarBAMazepine. Monitor therapy
FluvoxaMINE: May increase the serum concentration of CarBAMazepine. Monitor therapy
Fosaprepitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Fosaprepitant. Specifically, CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite aprepitant. Avoid combination
Fosnetupitant: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Fosnetupitant. Avoid combination
Fosphenytoin: May decrease the serum concentration of CarBAMazepine. CarBAMazepine may decrease the serum concentration of Fosphenytoin. CarBAMazepine may increase the serum concentration of Fosphenytoin. Possibly by competitive inhibition at sites of metabolism. Consider therapy modification
Fostamatinib: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Fostamatinib. Avoid combination
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Gefitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Gefitinib. Management: In the absence of severe adverse reactions, increase gefitinib dose to 500 mg daily in patients receiving strong CYP3A4 inducers; resume 250 mg dose 7 days after discontinuation of the strong inducer. Carefully monitor clinical response. Consider therapy modification
Gemigliptin: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Gemigliptin. CYP3A4 Inducers (Strong) may decrease the serum concentration of Gemigliptin. Avoid combination
Gestrinone: CarBAMazepine may decrease the serum concentration of Gestrinone. Monitor therapy
Gilteritinib: Combined Inducers of CYP3A4 and P-glycoprotein may decrease the serum concentration of Gilteritinib. Avoid combination
Glasdegib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Glasdegib. Avoid combination
Glecaprevir and Pibrentasvir: CarBAMazepine may decrease the serum concentration of Glecaprevir and Pibrentasvir. Avoid combination
Grapefruit Juice: May increase the serum concentration of CarBAMazepine. Monitor therapy
Grazoprevir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Grazoprevir. Avoid combination
GuanFACINE: CYP3A4 Inducers (Strong) may decrease the serum concentration of GuanFACINE. Management: Increase the guanfacine dose by up to double when initiating guanfacine in a patient taking a strong CYP3A4 inducer. Increase guanfacine dose gradually over 1 to 2 weeks if initiating strong CYP3A4 inducer therapy in a patient already taking guanfacine. Consider therapy modification
Haloperidol: CarBAMazepine may decrease the serum concentration of Haloperidol. Monitor therapy
HYDROcodone: CYP3A4 Inducers (Strong) may decrease the serum concentration of HYDROcodone. Monitor therapy
Hydrocortisone (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Hydrocortisone (Systemic). Monitor therapy
Ibrutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ibrutinib. Avoid combination
Idelalisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Idelalisib. Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ifosfamide: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Ifosfamide. CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Imatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Imatinib. Management: Avoid concurrent use of imatinib with strong CYP3A4 inducers when possible. If such a combination must be used, increase imatinib dose by at least 50% and monitor the patient's clinical response closely. Consider therapy modification
Irinotecan Products: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Irinotecan Products. Specifically, serum concentrations of SN-38 may be reduced. CYP3A4 Inducers (Strong) may decrease the serum concentration of Irinotecan Products. Avoid combination
Isavuconazonium Sulfate: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Isavuconazonium Sulfate. Specifically, CYP3A4 Inducers (Strong) may decrease isavuconazole serum concentrations. Avoid combination
Isoniazid: CarBAMazepine may enhance the hepatotoxic effect of Isoniazid. Isoniazid may increase the serum concentration of CarBAMazepine. Monitor therapy
Istradefylline: CYP3A4 Inducers (Strong) may decrease the serum concentration of Istradefylline. Avoid combination
Itraconazole: CYP3A4 Inducers (Strong) may decrease the serum concentration of Itraconazole. Avoid combination
Ivabradine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ivabradine. Avoid combination
Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ivacaftor. Avoid combination
Ivosidenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ivosidenib. Avoid combination
Ixabepilone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ixabepilone. Management: Avoid this combination whenever possible. If this combination must be used, a gradual increase in ixabepilone dose from 40 mg/m2 to 60 mg/m2 (given as a 4-hour infusion), as tolerated, should be considered. Consider therapy modification
Ixazomib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ixazomib. Avoid combination
Lacosamide: Antiepileptic Agents (Sodium Channel Blockers) may enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
LamoTRIgine: May enhance the adverse/toxic effect of CarBAMazepine. CarBAMazepine may increase the metabolism of LamoTRIgine. Consider therapy modification
Lapatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lapatinib. Management: If therapy overlap cannot be avoided, consider titrating lapatinib gradually from 1,250 mg/day up to 4,500 mg/day (HER2 positive metastatic breast cancer) or 1,500 mg/day up to 5,500 mg/day (hormone receptor/HER2 positive breast cancer) as tolerated. Avoid combination
Larotrectinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Larotrectinib. Management: Avoid use of strong CYP3A4 inducers with larotrectinib. If this combination cannot be avoided, double the larotrectinib dose. Reduced to previous dose after stopping the inducer after a period of 3 to 5 times the inducer half-life. Consider therapy modification
Ledipasvir: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Ledipasvir. Avoid combination
Lefamulin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin with strong CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lefamulin: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin with P-glycoprotein/ABCB1 inducers unless the benefits outweigh the risks. Consider therapy modification
Lefamulin (Intravenous): CYP3A4 Inducers (Strong) may decrease the serum concentration of Lefamulin (Intravenous). Management: Avoid concomitant use of lefamulin intravenous infusion with strong CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lefamulin (Intravenous): P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Lefamulin (Intravenous). Management: Avoid concomitant use of lefamulin (intravenous) with P-glycoprotein/ABCB1 inducers unless the benefits outweigh the risks. Consider therapy modification
Lemborexant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lemborexant. Avoid combination
Letermovir: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Letermovir. Avoid combination
Letermovir: May increase the serum concentration of UGT1A1 Inducers. Avoid combination
LevETIRAcetam: May enhance the adverse/toxic effect of CarBAMazepine. CarBAMazepine may decrease the serum concentration of LevETIRAcetam. Monitor therapy
Levomethadone: CarBAMazepine may decrease the serum concentration of Levomethadone. Monitor therapy
LinaGLIPtin: CYP3A4 Inducers (Strong) may decrease the serum concentration of LinaGLIPtin. Management: Strongly consider using an alternative to any strong CYP3A4 inducer in patients who are being treated with linagliptin. If this combination is used, monitor patients closely for evidence of reduced linagliptin effectiveness. Consider therapy modification
LinaGLIPtin: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of LinaGLIPtin. Management: Strongly consider using an alternative to any strong P-glycoprotein inducer in patients who are being treated with linagliptin. If this combination is used, monitor patients closely for evidence of reduced linagliptin effectiveness. Consider therapy modification
Lithium: CarBAMazepine may enhance the adverse/toxic effect of Lithium. Monitor therapy
Lopinavir: CarBAMazepine may decrease the serum concentration of Lopinavir. Management: Increased doses of lopinavir may be necessary when using these agents in combination. Do not use a once daily lopinavir/ritonavir regimen together with carbamazepine. Increase monitoring of therapeutic response in all patients using this combination. Consider therapy modification
Lorlatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lorlatinib. Avoid combination
Loxapine: May increase serum concentrations of the active metabolite(s) of CarBAMazepine. Monitor therapy
Lumacaftor and Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lumacaftor and Ivacaftor. Specifically, the serum concentration of ivacaftor may be decreased. Avoid combination
Lumateperone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lumateperone. Avoid combination
Lumefantrine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lumefantrine. Avoid combination
Lurasidone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lurasidone. Avoid combination
Macimorelin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Macimorelin. Avoid combination
Macitentan: CYP3A4 Inducers (Strong) may decrease the serum concentration of Macitentan. Avoid combination
Manidipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Manidipine. Management: Consider avoiding concomitant use of manidipine and strong CYP3A4 inducers. If combined, monitor closely for decreased manidipine effects and loss of efficacy. Increased manidipine doses may be required. Consider therapy modification
Maraviroc: CYP3A4 Inducers (Strong) may decrease the serum concentration of Maraviroc. Management: Increase maraviroc adult dose to 600 mg twice daily when used with strong CYP3A4 inducers. This does not apply to patients also receiving strong CYP3A4 inhibitors. Do not use maraviroc with strong CYP3A4 inducers in patients with CrCl less than 30 mL/min. Consider therapy modification
Mebendazole: CarBAMazepine may decrease the serum concentration of Mebendazole. Monitor therapy
Mefloquine: May diminish the therapeutic effect of Anticonvulsants. Mefloquine may decrease the serum concentration of Anticonvulsants. Management: Mefloquine is contraindicated for malaria prophylaxis in persons with a history of convulsions. Monitor anticonvulsant concentrations and treatment response closely with concurrent use. Consider therapy modification
Meperidine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Meperidine. Monitor therapy
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Methadone: CarBAMazepine may decrease the serum concentration of Methadone. Monitor therapy
Methylfolate: May decrease the serum concentration of CarBAMazepine. Monitor therapy
MethylPREDNISolone: CYP3A4 Inducers (Strong) may decrease the serum concentration of MethylPREDNISolone. Management: Consider methylprednisolone dose increases in patients receiving strong CYP3A4 inducers and monitor closely for reduced steroid efficacy. Consider therapy modification
Mianserin: May diminish the therapeutic effect of CarBAMazepine. CarBAMazepine may decrease the serum concentration of Mianserin. Monitor therapy
Midostaurin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Midostaurin. Avoid combination
MiFEPRIStone: CYP3A4 Inducers (Strong) may decrease the serum concentration of MiFEPRIStone. Avoid combination
Mirodenafil: CYP3A4 Inducers (Strong) may decrease the serum concentration of Mirodenafil. Management: Consider avoiding the concomitant use of mirodenafil and strong CYP3A4 inducers. If combined, monitor for decreased mirodenafil effects. Mirodenafil dose increases may be required to achieve desired effects. Consider therapy modification
Mirtazapine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Mirtazapine. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Monoamine Oxidase Inhibitors: CarBAMazepine may enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Management: Avoid concurrent use of carbamazepine during, or within 14 days of discontinuing, treatment with a monoamine oxidase inhibitor. Avoid combination
Naldemedine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Naldemedine. Avoid combination
Naloxegol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Naloxegol. Avoid combination
Nefazodone: May increase the serum concentration of CarBAMazepine. Also, concentrations of the active CarBAMazepine epoxide metabolite may be reduced. CarBAMazepine may decrease the serum concentration of Nefazodone. Concentrations of active Nefazodone metabolites may also be reduced. Avoid combination
Neratinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Neratinib. Avoid combination
Netupitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Netupitant. Avoid combination
Neuromuscular-Blocking Agents (Nondepolarizing): CarBAMazepine may decrease the serum concentration of Neuromuscular-Blocking Agents (Nondepolarizing). Monitor therapy
Nevirapine: CarBAMazepine may decrease the serum concentration of Nevirapine. Avoid combination
NIFEdipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of NIFEdipine. Avoid combination
Nilotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Nilotinib. Avoid combination
NiMODipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of NiMODipine. Avoid combination
Nintedanib: Combined Inducers of CYP3A4 and P-glycoprotein may decrease the serum concentration of Nintedanib. Avoid combination
Nisoldipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Nisoldipine. Avoid combination
OLANZapine: CarBAMazepine may decrease the serum concentration of OLANZapine. Monitor therapy
Olaparib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Olaparib. Avoid combination
Orlistat: May decrease the serum concentration of Anticonvulsants. Monitor therapy
Osimertinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Osimertinib. Consider therapy modification
OXcarbazepine: CYP3A4 Inducers (Strong) may decrease the serum concentration of OXcarbazepine. Specifically, the concentrations of the 10-monohydroxy active metabolite of oxcarbazepine may be decreased. Monitor therapy
Palbociclib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Palbociclib. Avoid combination
Paliperidone: CarBAMazepine may decrease the serum concentration of Paliperidone. Monitor therapy
Panobinostat: CYP3A4 Inducers (Strong) may decrease the serum concentration of Panobinostat. Avoid combination
PAZOPanib: CYP3A4 Inducers (Strong) may decrease the serum concentration of PAZOPanib. Avoid combination
Perampanel: CarBAMazepine may decrease the serum concentration of Perampanel. Management: Increase the perampanel starting dose to 4 mg/day when perampanel is used with carbamazepine. Patients receiving this combination should be followed closely for response, especially with any changes to carbamazepine therapy. Consider therapy modification
Pexidartinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pexidartinib. Avoid combination
P-glycoprotein/ABCB1 Substrates: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Exceptions: Betrixaban; Edoxaban. Monitor therapy
Phenytoin: CarBAMazepine may decrease the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of CarBAMazepine. CarBAMazepine may increase the serum concentration of Phenytoin. Possibly by competitive inhibition at sites of metabolism. Consider therapy modification
Pimavanserin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pimavanserin. Avoid combination
Piperaquine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Piperaquine. Avoid combination
Pitolisant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pitolisant. Management: For patients who are stable on pitolisant doses of 8.9 mg or 17.8 mg/day and who are also taking a strong CYP3A4 inducer, increase the pitolisant dose over 7 days to double the original dose (ie, to either 17.8 mg/day or 35.6 mg/day, respectively). Consider therapy modification
Polatuzumab Vedotin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Polatuzumab Vedotin. Exposure to unconjugated MMAE, the cytotoxic small molecule component of polatuzumab vedotin, may be decreased. Monitor therapy
PONATinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of PONATinib. Avoid combination
Pravastatin: CarBAMazepine may decrease the serum concentration of Pravastatin. Monitor therapy
Praziquantel: CYP3A4 Inducers (Strong) may decrease the serum concentration of Praziquantel. Management: Use of praziquantel with strong CYP3A4 inducers is contraindicated. Discontinue rifampin 4 weeks prior to initiation of praziquantel therapy. Rifampin may be resumed the day following praziquantel completion. Avoid combination
PrednisoLONE (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of PrednisoLONE (Systemic). Monitor therapy
PredniSONE: CYP3A4 Inducers (Strong) may decrease the serum concentration of PredniSONE. Monitor therapy
Pretomanid: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pretomanid. Avoid combination
Progestins (Contraceptive): CarBAMazepine may diminish the therapeutic effect of Progestins (Contraceptive). Contraceptive failure is possible. Management: Use of alternative, nonhormonal contraceptives is recommended. Consider therapy modification
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Propacetamol: CarBAMazepine may increase the metabolism of Propacetamol. This may 1) diminish the desired effects of propacetamol; and 2) increase the risk of liver damage. Monitor therapy
Propafenone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Propafenone. Monitor therapy
Protease Inhibitors: CarBAMazepine may increase the metabolism of Protease Inhibitors. Protease Inhibitors may decrease the metabolism of CarBAMazepine. Consider therapy modification
QUEtiapine: May increase serum concentrations of the active metabolite(s) of CarBAMazepine. CarBAMazepine may decrease the serum concentration of QUEtiapine. Management: Quetiapine dose increases to as much as 5 times the regular dose may be required to maintain therapeutic benefit. Reduce the quetiapine dose back to the previous/regular dose within 7 to 14 days of discontinuing carbamazepine. Consider therapy modification
QuiNINE: CarBAMazepine may decrease the serum concentration of QuiNINE. QuiNINE may increase the serum concentration of CarBAMazepine. Consider therapy modification
Radotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Radotinib. Management: Consider alternatives to this combination when possible as the risk of radotinib treatment failure may be increased. Consider therapy modification
Ramelteon: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ramelteon. Monitor therapy
Ranolazine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ranolazine. Avoid combination
Reboxetine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Reboxetine. Monitor therapy
Regorafenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Regorafenib. Avoid combination
Resveratrol: May increase the serum concentration of CarBAMazepine. Monitor therapy
Ribociclib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ribociclib. Avoid combination
Rilpivirine: CarBAMazepine may decrease the serum concentration of Rilpivirine. Avoid combination
RisperiDONE: CYP3A4 Inducers (Strong) may decrease the serum concentration of RisperiDONE. Management: Consider increasing the dose of oral risperidone (to no more than double the original dose) if a strong CYP3A4 inducer is initiated. For patients on IM risperidone, consider an increased IM dose or supplemental doses of oral risperidone. Consider therapy modification
Rivaroxaban: CYP3A4 Inducers (Strong) may decrease the serum concentration of Rivaroxaban. Avoid combination
Roflumilast: CYP3A4 Inducers (Strong) may decrease the serum concentration of Roflumilast. Management: Roflumilast U.S. prescribing information recommends against combining strong CYP3A4 inducers with roflumilast. The Canadian product monograph makes no such recommendation but notes that such agents may reduce roflumilast therapeutic effects. Avoid combination
Rolapitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Rolapitant. Management: Avoid rolapitant use in patients requiring chronic administration of strong CYP3A4 inducers. Monitor for reduced rolapitant response and the need for alternative or additional antiemetic therapy even with shorter-term use of such inducers. Consider therapy modification
RomiDEPsin: CYP3A4 Inducers (Strong) may decrease the serum concentration of RomiDEPsin. Avoid combination
Rosuvastatin: CarBAMazepine may decrease the serum concentration of Rosuvastatin. Monitor therapy
Rufinamide: May decrease the serum concentration of CarBAMazepine. CarBAMazepine may decrease the serum concentration of Rufinamide. Monitor therapy
Ruxolitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ruxolitinib. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
SAXagliptin: CYP3A4 Inducers (Strong) may decrease the serum concentration of SAXagliptin. Monitor therapy
Sertraline: CarBAMazepine may decrease the serum concentration of Sertraline. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Simeprevir. Avoid combination
Sirolimus: CYP3A4 Inducers (Strong) may decrease the serum concentration of Sirolimus. Management: Avoid concomitant use of strong CYP3A4 inducers and sirolimus if possible. If combined, monitor for reduced serum sirolimus concentrations. Sirolimus dose increases will likely be necessary to prevent subtherapeutic sirolimus levels. Consider therapy modification
Sofosbuvir: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Sofosbuvir. Avoid combination
Sonidegib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Sonidegib. Avoid combination
SORAfenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of SORAfenib. Avoid combination
Stiripentol: May increase the serum concentration of CarBAMazepine. Avoid combination
SUFentanil: CYP3A4 Inducers (Strong) may decrease the serum concentration of SUFentanil. Monitor therapy
Sulthiame: CarBAMazepine may decrease the serum concentration of Sulthiame. Monitor therapy
SUNItinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of SUNItinib. Management: Avoid when possible. If such a combination cannot be avoided, sunitinib dose increases are recommended, and vary by indication. See full monograph for details. Consider therapy modification
Tadalafil: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tadalafil. Management: Erectile dysfunction: monitor for decreased effectiveness - no standard dose adjustments recommended. Avoid use of tadalafil for pulmonary arterial hypertension in patients receiving a strong CYP3A4 inducer. Consider therapy modification
Tamoxifen: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Tamoxifen. CYP3A4 Inducers (Strong) may decrease the serum concentration of Tamoxifen. Management: Consider alternatives to concomitant use of strong CYP3A4 inducers and tamoxifen. If the combination cannot be avoided, monitor for reduced therapeutic effects of tamoxifen. Consider therapy modification
Tasimelteon: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tasimelteon. Avoid combination
Tazemetostat: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tazemetostat. Avoid combination
Telithromycin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Telithromycin. Avoid combination
Temsirolimus: CarBAMazepine may decrease the serum concentration of Temsirolimus. Concentrations of the active metabolite, sirolimus, are also likely to be decreased (and maybe to an even greater degree). Management: Temsirolimus prescribing information recommends against coadministration with strong CYP3A4 inducers such as carbamazepine; however, if concurrent therapy is necessary, an increase in temsirolimus adult dose to 50 mg/week should be considered. Consider therapy modification
Tenofovir Alafenamide: CarBAMazepine may decrease the serum concentration of Tenofovir Alafenamide. Avoid combination
Tetrahydrocannabinol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tetrahydrocannabinol. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tetrahydrocannabinol and Cannabidiol. Monitor therapy
Tezacaftor and Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tezacaftor and Ivacaftor. Avoid combination
Theophylline Derivatives: CarBAMazepine may decrease the serum concentration of Theophylline Derivatives. Theophylline Derivatives may decrease the serum concentration of CarBAMazepine. Management: Seek alternatives to this combination when possible. If these agents are used together, monitor closely for decreased serum concentrations/therapeutic effects of both medications. Exceptions: Dyphylline. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: May enhance the adverse/toxic effect of CarBAMazepine. Specifically, there may be an increased risk for hyponatremia. Monitor therapy
Thiotepa: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Thiotepa. CYP3A4 Inducers (Strong) may decrease the serum concentration of Thiotepa. Management: Thiotepa prescribing information recommends avoiding concomitant use of thiotepa and strong CYP3A4 inducers. If concomitant use is unavoidable, monitor for adverse effects. Consider therapy modification
Thiothixene: CarBAMazepine may decrease the serum concentration of Thiothixene. Monitor therapy
Thyroid Products: CarBAMazepine may decrease the serum concentration of Thyroid Products. Monitor therapy
TiaGABine: CYP3A4 Inducers (Strong) may decrease the serum concentration of TiaGABine. Management: Approximately 2-fold higher tiagabine doses and a more rapid dose titration will likely be required in patients concomitantly taking a strong CYP3A4 inducer. Consider therapy modification
Ticagrelor: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Ticagrelor. CYP3A4 Inducers (Strong) may decrease the serum concentration of Ticagrelor. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tofacitinib. Avoid combination
Tolvaptan: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tolvaptan. Management: If concurrent use is necessary, increased doses of tolvaptan (with close monitoring for toxicity and clinical response) may be needed. Avoid combination
Topiramate: CarBAMazepine may decrease the serum concentration of Topiramate. Consider therapy modification
Toremifene: CYP3A4 Inducers (Strong) may decrease the serum concentration of Toremifene. Avoid combination
Trabectedin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Trabectedin. Avoid combination
TraMADol: May enhance the CNS depressant effect of CarBAMazepine. TraMADol may diminish the therapeutic effect of CarBAMazepine. CarBAMazepine may decrease the serum concentration of TraMADol. Avoid combination
Tricyclic Antidepressants: CarBAMazepine may decrease the serum concentration of Tricyclic Antidepressants. Monitor therapy
Tropisetron: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tropisetron. Monitor therapy
Ubrogepant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ubrogepant. Avoid combination
Udenafil: CYP3A4 Inducers (Strong) may decrease the serum concentration of Udenafil. Monitor therapy
Ulipristal: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ulipristal. Avoid combination
Upadacitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Upadacitinib. Avoid combination
Valbenazine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Valbenazine. Avoid combination
Valproate Products: May increase serum concentrations of the active metabolite(s) of CarBAMazepine. Parent carbamazepine concentrations may be increased, decreased, or unchanged. CarBAMazepine may decrease the serum concentration of Valproate Products. Monitor therapy
Vandetanib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vandetanib. Avoid combination
Vecuronium: CarBAMazepine may decrease the serum concentration of Vecuronium. Monitor therapy
Velpatasvir: CYP2B6 Inducers (Moderate) may decrease the serum concentration of Velpatasvir. Avoid combination
Velpatasvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Velpatasvir. Avoid combination
Velpatasvir: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Velpatasvir. Avoid combination
Vemurafenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vemurafenib. Management: Avoid concurrent use of vemurafenib with a strong CYP3A4 inducer and replace with another agent when possible. If a strong CYP3A4 inducer is indicated and unavoidable, the dose of vemurafenib may be increased by 240 mg (1 tablet) as tolerated. Consider therapy modification
Venetoclax: CYP3A4 Inducers (Strong) may decrease the serum concentration of Venetoclax. Avoid combination
Vilazodone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vilazodone. Management: Consider increasing vilazodone dose by as much as 2-fold (do not exceed 80 mg/day), based on response, in patients receiving strong CYP3A4 inducers for > 14 days. Reduce to the original vilazodone dose over 1-2 weeks after inducer discontinuation. Consider therapy modification
VinCRIStine (Liposomal): CYP3A4 Inducers (Strong) may decrease the serum concentration of VinCRIStine (Liposomal). Avoid combination
VinCRIStine (Liposomal): P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of VinCRIStine (Liposomal). Avoid combination
Vinflunine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vinflunine. Avoid combination
Vitamin K Antagonists (eg, warfarin): CarBAMazepine may decrease the serum concentration of Vitamin K Antagonists. Management: Monitor for decreased INR and effects of vitamin K antagonists if carbamazepine is initiated/dose increased, or increased INR and effects if carbamazepine is discontinued/dose decreased. Warfarin dose adjustments will likely be required. Consider therapy modification
Vorapaxar: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vorapaxar. Avoid combination
Voriconazole: CarBAMazepine may decrease the serum concentration of Voriconazole. Avoid combination
Vortioxetine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vortioxetine. Management: Consider increasing the vortioxetine dose to no more than 3 times the original dose when used with a strong drug metabolism inducer for more than 14 days. The vortioxetine dose should be returned to normal within 14 days of stopping the strong inducer. Consider therapy modification
Voxelotor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Voxelotor. Management: Avoid concomitant use of voxelotor and strong CYP3A4 inducers. If concomitant use is unavoidable, increase the voxelotor dose to 2,500 mg once daily. Consider therapy modification
Voxilaprevir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Voxilaprevir. Avoid combination
Zaleplon: CYP3A4 Inducers (Strong) may decrease the serum concentration of Zaleplon. Management: Consider the use of an alternative hypnotic that is not metabolized by CYP3A4 in patients receiving strong CYP3A4 inducers. If zalephon is combined with a strong CYP3A4 inducer, monitor for decreased effectiveness of zaleplon. Consider therapy modification
Zanubrutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Zanubrutinib. Avoid combination
Ziprasidone: CarBAMazepine may decrease the serum concentration of Ziprasidone. Monitor therapy
Zolpidem: May enhance the CNS depressant effect of CarBAMazepine. CarBAMazepine may decrease the serum concentration of Zolpidem. Management: Monitor zolpidem response closely. Reduce the Intermezzo brand sublingual zolpidem dose to 1.75 mg for men who are also receiving carbamazepine. No such dose change is recommended for women. Monitor therapy
Zuclopenthixol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Zuclopenthixol. Monitor therapy
Test Interactions
May cause false-positive serum TCA screen; may interact with some pregnancy tests
Adverse Reactions
>10%:
Central nervous system: Dizziness (44%), drowsiness (32%), ataxia (15%)
Gastrointestinal: Nausea (29%), vomiting (18%)
1% to 10%:
Cardiovascular: Hypertension (3%)
Central nervous system: Speech disturbance (6%), abnormality in thinking (2%), paresthesia (2%), twitching (2%), vertigo (2%)
Dermatologic: Pruritus (8%), skin rash (7%)
Gastrointestinal: Constipation (10%), xerostomia (8%)
Neuromuscular & skeletal: Weakness (8%), tremor (3%)
Ophthalmic: Blurred vision (5% to 6%)
Frequency not defined:
Cardiovascular: Arterial insufficiency (cerebral artery), atrioventricular block, cardiac arrhythmia, cardiac failure, collapse, coronary artery disease (aggravation), edema, exacerbation of hypertension, hypotension, pulmonary embolism, syncope, thromboembolism, thrombophlebitis
Central nervous system: Agitation, chills, confusion, depression, fatigue, headache, hyperacusis, involuntary body movements, neuroleptic malignant syndrome, peripheral neuritis, talkativeness, unsteadiness, visual hallucination
Dermatologic: Acute generalized exanthematous pustulosis, alopecia, diaphoresis, dyschromia, erythema multiforme, erythema nodosum, erythematous rash, exfoliative dermatitis, maculopapular rash, onychomadesis, pruritic rash, skin photosensitivity, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Endocrine & metabolic: Acute porphyria, albuminuria, decreased serum calcium, glycosuria, hirsutism, hyponatremia, porphyria cutanea tarda, porphyria (variegate), SIADH
Gastrointestinal: Abdominal pain, anorexia, diarrhea, gastric distress, glossitis, pancreatitis, stomatitis
Genitourinary: Acute urinary retention, azotemia, defective spermatogenesis, impotence, microscopic urine deposits, oliguria, reduced fertility (male), urinary frequency
Hematologic & oncologic: Adenopathy, agranulocytosis, aplastic anemia, bone marrow depression, eosinophilia, hypogammaglobulinemia, leukocytosis, leukopenia, lymphadenopathy, pancytopenia, purpura, thrombocytopenia
Hepatic: Abnormal hepatic function tests, cholestatic jaundice, hepatic failure, hepatitis, hepatocellular jaundice, increased liver enzymes
Hypersensitivity: Hypersensitivity reaction
Immunologic: DRESS syndrome
Neuromuscular & skeletal: Arthralgia, exacerbation of systemic lupus erythematosus, leg cramps, lupus-like syndrome, myalgia, osteoporosis
Ophthalmic: Conjunctivitis, diplopia, increased intraocular pressure, punctate cataract, nystagmus, oculomotor disturbance
Otic: Tinnitus
Renal: Increased blood urea nitrogen, renal failure
Respiratory: Dry throat, pulmonary hypersensitivity
Miscellaneous: Fever
<1%, postmarketing, and/or case reports: Anaphylaxis, angioedema, aseptic meningitis, decreased thyroid hormones, dysgeusia (Syed 2016), eyelid edema, glottis edema, hepatotoxicity (idiosyncratic: Chalasani 2014), intrahepatic cholestasis (vanishing bile duct syndrome), laryngeal edema, lip edema, suicidal tendencies
Warnings/Precautions
Concerns related to adverse effects:
- Blood dyscrasias: [US Boxed Warning]: The risk of developing anemia or agranulocytosis is increased during treatment. Complete pretreatment hematological testing should be obtained prior to use; monitor patient closely if white blood cells or platelet counts decrease during therapy; discontinue if significant bone marrow suppression occurs. A spectrum of hematologic effects has been reported with use (eg, agranulocytosis, aplastic anemia, neutropenia, leukopenia, thrombocytopenia, pancytopenia, and anemias); patients with a previous history of adverse hematologic reaction to any drug may be at increased risk. Early detection of hematologic change is important; advise patients of early signs and symptoms including fever, sore throat, mouth ulcers, infections, easy bruising, and petechial or purpuric hemorrhage.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Dermatologic toxicity: [US Boxed Warning]: Severe and sometimes fatal dermatologic reactions, including toxic epidermal necrolysis (TEN) and Stevens-Johnson syndrome (SJS), may occur during therapy. The risk is increased in patients with the variant HLA-B*1502 allele, found most often in patients of Asian ancestry. Patients with an increased likelihood of carrying this allele should be screened prior to initiating therapy. Avoid use in patients testing positive for the allele; discontinue therapy in patients who have a serious dermatologic reaction. The risk of SJS or TEN may also be increased if carbamazepine is used in combination with other antiepileptic drugs associated with these reactions. Presence of the HLA-B*1502 allele has not been found to predict the risk of less serious dermatologic reactions such as anticonvulsant hypersensitivity syndrome or nonserious rash.
- Hepatotoxicity: Hepatotoxicity ranging from slight elevations in liver enzymes to rare hepatic failure has been reported and may occur concomitantly with other immunoallergenic syndromes such as multiorgan hypersensitivity (DRESS syndrome) and serious dermatologic reactions including SJS; monitor baseline and periodic liver function, particularly in patients with a history of liver disease; discontinue carbamazepine immediately in cases of aggravated liver dysfunction or active liver disease. In some cases, hepatic effects may progress despite discontinuation of carbamazepine. Rare cases of a hepatic failure and vanishing bile duct syndrome involving destruction and disappearance of the intrahepatic bile ducts have been reported. Clinical courses of vanishing bile duct syndrome have been variable ranging from fulminant to indolent.
- Hypersensitivity reactions: The risk of developing a hypersensitivity reaction may be increased in patients with the variant HLA-A*3101 allele. These hypersensitivity reactions include SJS/TEN, maculopapular eruptions, and drug reaction with eosinophilia and systemic symptoms (DRESS/multiorgan hypersensitivity). The HLA-A*3101 allele may occur more frequently in patients of African-American, Asian, European, Indian, Arabic, Latin American, and Native American ancestry. Hypersensitivity has also been reported in patients experiencing reactions to other anticonvulsants; the history of hypersensitivity reactions in the patient or their immediate family members should be reviewed. Approximately 25% to 30% of patients allergic to carbamazepine will also have reactions with oxcarbazepine. Also, rare cases of anaphylaxis and angioedema have been reported; may occur after first dose or subsequent doses. Discontinue therapy if symptoms occur. Do not rechallenge patients if such reactions occur; initiate alternative treatment.
- Hyponatremia: Hyponatremia may occur and is often caused by the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Risk of SIADH appears to be dose-related. Elderly or patients taking diuretics are at increased risk for hyponatremia. Consider discontinuing therapy in patients with symptomatic hyponatremia.
- Multiorgan hypersensitivity reactions: Potentially serious, sometimes fatal multiorgan hypersensitivity reactions (also known as drug reaction with eosinophilia and systemic symptoms [DRESS]) have been reported with some antiepileptic drugs; including carbamazepine; monitor for signs and symptoms of possible disparate manifestations associated with lymphatic, hepatic, renal, and/or hematologic organ systems; gradual discontinuation and conversion to alternate therapy may be required.
- Psychiatric effects: May activate latent psychosis and/or cause confusion or agitation; elderly patients may be at an increased risk for psychiatric effects.
- Renal toxicity: Renal toxicity has been reported; monitor renal function at baseline and periodically thereafter.
- Suicidal ideation: Pooled analysis of trials involving various antiepileptics (regardless of indication) showed an increased risk of suicidal thoughts/behavior (incidence rate: 0.43% treated patients compared to 0.24% of patients receiving placebo); risk observed as early as 1 week after initiation and continued through duration of trials (most trials ≤24 weeks). Monitor all patients for notable changes in behavior that might indicate suicidal thoughts or depression; notify healthcare provider immediately if symptoms occur.
Disease-related concerns:
- Anticholinergic sensitivity: Has mild anticholinergic activity; use with caution in patients with sensitivity to anticholinergic effects (urinary retention, increased intraocular pressure, constipation).
- Cardiovascular disease: May cause conduction abnormalities, including AV heart block; use caution in patients with underlying ECG abnormalities, preexisting cardiac damage, or patients who are at risk for conduction abnormalities. In a scientific statement from the American Heart Association, carbamazepine has been determined to be an agent that may exacerbate underlying myocardial dysfunction (magnitude: major) in patients with heart failure (AHA [Page 2016]).
- Hepatic impairment: Use with caution in patients with hepatic impairment; avoid use in patients with hepatic porphyria (eg, acute intermittent porphyria, variegate porphyria, porphyria cutanea tarda).
- Renal impairment: Use with caution in patients with renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Asian ancestry: [US Boxed Warning]: Patients with an increased likelihood of carrying the HLA-B*1502 allele, such as those of Asian descent, should be screened for the variant HLA-B*1502 allele prior to initiating therapy. This genetic variant has been associated with a significantly increased risk of developing Stevens-Johnson syndrome and/or toxic epidermal necrolysis. Patients with a positive result should not be started on carbamazepine.
- Elderly: May activate latent psychosis, confusion, or agitation.
- Pediatric: Exacerbation of certain seizure types have been seen after initiation of therapy in children with mixed seizure disorders.
Dosage form specific issues:
- Sorbitol: The suspension may contain sorbitol; avoid use in patents with hereditary fructose intolerance.
- Suspension: Administration of the suspension will yield higher peak and lower trough serum levels than an equal dose of the tablet form; consider a lower starting dose given more frequently (same total daily dose) when using the suspension.
Other warnings/precautions:
- Appropriate use: Not effective in absence, myoclonic, or akinetic seizures; carbamazepine administration may increase the frequency of seizures in patients with these types of seizures.
- Withdrawal: Anticonvulsants should not be discontinued abruptly because of the possibility of increasing seizure frequency; therapy should be withdrawn gradually to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal.
Monitoring Parameters
Baseline and periodic: CBC with platelet count and differential, reticulocytes, serum iron, liver and renal function tests, urinalysis, BUN, serum sodium, ophthalmic exam including intraocular pressure.
As appropriate: Lipid panel, serum carbamazepine levels, thyroid function tests; pregnancy test; observe patient for excessive sedation, especially when instituting or increasing therapy; signs of rash; HLA-B*1502 and HLA-A*3101 genotype screening prior to therapy initiation in patients with ancestry in genetically at-risk populations; suicidality (eg, suicidal thoughts, depression, behavioral changes)
Pregnancy
Pregnancy Considerations
Carbamazepine and its active metabolite cross the placenta; concentrations are variable but correlate with maternal serum concentrations (Kacirova 2016).
Carbamazepine may be associated with teratogenic effects, including spina bifida, craniofacial defects, and cardiovascular malformations. Data from the International Registry of Antiepileptic Drugs and Pregnancy (EURAP) and the UK and Ireland Epilepsy Pregnancy Registers (UKEPR) note the risk of congenital malformations increases with higher doses (Campbell 2014; Tomson 2011). The risk of teratogenic effects is higher with anticonvulsant polytherapy than monotherapy. Developmental delays have also been observed following in utero exposure to carbamazepine (per manufacturer).
Due to pregnancy-induced physiologic changes, some pharmacokinetic properties of carbamazepine may be altered; however, available studies have slightly conflicting results (Deligiannidis 2014; Tomson 2013). Therapeutic drug monitoring of carbamazepine is recommended in pregnant women (Harden 2009; Hiemke 2018).
Carbamazepine is not recommended for the treatment of bipolar disorder in pregnancy (Larsen 2015).
Carbamazepine may decrease plasma concentrations of hormonal contraceptives; alternate or back-up methods of contraception should be considered. Carbamazepine may interfere with some pregnancy tests.
Patients exposed to carbamazepine during pregnancy are encouraged to enroll themselves into the North American Antiepileptic Drug (NAAED) Pregnancy Registry by calling 1-888-233-2334. Additional information is available at www.aedpregnancyregistry.org.
Patient Education
What is this drug used for?
- It is used to treat seizures.
- It is used to treat pain caused by a problem with a nerve in the face.
- It is used to treat bipolar problems.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Dizziness
- Fatigue
- Nausea
- Vomiting
- Dry mouth
- Loss of strength and energy
- Constipation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Swelling in your throat
- Infection
- Aplastic anemia like fever, sore throat, mouth sores, infections, bruising, or purple skin splotches.
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Low sodium like headache, difficulty focusing, trouble with memory, confusion, weakness, seizures, or change in balance.
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- DVT like edema, warmth, numbness, change in color, or pain in the extremities.
- Neuroleptic malignant syndrome like fever, muscle cramps or stiffness, dizziness, severe headache, confusion, change in thinking, fast heartbeat, abnormal heartbeat, or sweating a lot.
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Agitation
- Irritability
- Panic attacks
- Mood changes
- Heart problems like cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out.
- Seizures
- Change in speech
- Sensing things that seem real but are not
- Involuntary eye movements
- Slow heartbeat
- Vision changes
- Swollen glands
- Severe muscle pain
- Severe joint pain
- Abnormal movements
- Burning or numbness feeling
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.
Patient Education
What is this drug used for?
Frequently reported side effects of this drug
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.